This article has been
cited by other articles in ScienceCentral.
ABSTRACT
A 25-year-old female visited the clinic with abdominal pain and poor oral intake.
She was diagnosed with Crohn’s disease and had a history of using
infliximab for 4 years. She had no previous operative history. Magnetic
resonance enterography demonstrated the progression of a penetrating
complication that involved the distal ileum and complex entero-enteric fistula
between the terminal ileum and sigmoid colon. Surgery was conducted using the da
Vinci SP surgical system. In the operative field, severe adhesion was observed
between the terminal ileum, adjacent ileum, cecum, and the sigmoid colon. After
adhesiolysis of the small bowel and right colon was performed, the fistula tract
between the sigmoid colon and terminal ileum was identified and resected. Then,
simultaneous ileocecectomy and anterior resection was performed. The operation
was completed without any intraoperative complications and patient’s
recovery was uneventful. She was discharged postoperatively, after 8 days.
Keywords: da Vinci SP, Robotic surgical procedures, Crohn disease, Digestive system fistula
Introduction
Minimally invasive surgery for Crohn’s Disease (CD) can be challenging due to
thickened and friable mesentery, enteric fistulas, bowel perforation, and frequent
occurrence of intra-abdominal abscess. Difficulties in the operative field are
reflected by a high rate of conversions and complications following surgical
treatment in patients with inflammatory bowel disease [
1]. Nevertheless, laparoscopic surgery for patients with
intra-abdominal lesions as a result of CD has been widely adopted [
2,
3].
Moreover, robotic ileocecal resection in patients with CD has been also reported
[
3–
5].
In 2018, Intuitive Surgical launched the da Vinci SP (dVSP) surgical system, which
was designed for pure robotic single-incision surgery. It overcame the problem of
requiring multiple ports in conventional robotic surgery and addressed concerns
involving triangulation and retraction in single-incision laparoscopic surgery. To
conduct surgery with a single port, a cannula, which consists of four channels, was
applied. Three instruments and one camera can be inserted through a single cannula.
Further, the 360° boom can reach anywhere in the abdominal cavity regardless
of the surgical target without the need for redocking. For proper triangulation and
retraction, each instrument has two joints called the elbow and the wrist joint. In
addition, articulating endoscope was adopted to eliminate instrument crashes.
Thus far, there are several reports on the results of minimally invasive approaches,
which include laparoscopic and robotic surgery in patients with intra-abdominal CD
[
3–
5]. However, to the best of our knowledge, there has been no report on
the application of the dVSP surgical system. Here we report the patient with
intra-abdominal CD who underwent simultaneous ileocecectomy and anterior resection
due to the fistula between the distal ileum and sigmoid colon.
Case
A 25-year-old female visited the clinic with abdominal pain and poor oral intake. She
was diagnosed with CD 4 years ago and had been taking infliximab ever since. She had
no previous operative history. On admission, her vital signs were non-specific. The
blood examination revealed mild elevated leukocyte count (10,010 /mm
3;
normal, 4.000–10,000 /mm
3) and mild elevated C-reactive protein
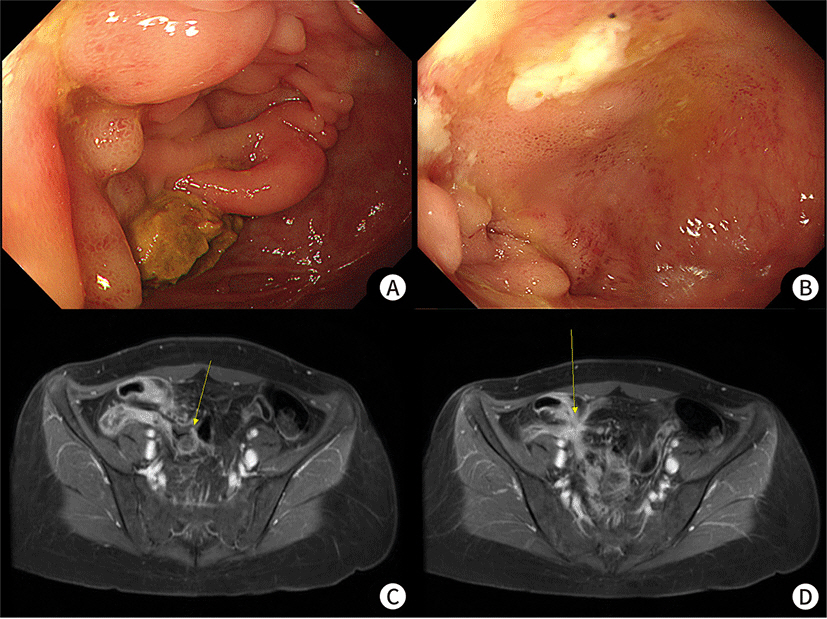
level (3.36 mg/dL; normal, 0–0.5 mg/dL). Colonoscopy showed a whitish scar
with inflammatory pseudopolyps in the cecum and a mild structure was observed in the
ileocecal valve, although scope passing was possible (
Fig. 1A). In the terminal ileum, an ulcer with edematous mucosa and
stenosis was observed; here, scope pass was impossible (
Fig. 1B). Magnetic resonance enterography demonstrated the
progression of a penetrating complication that involved distal ileum with a complex
entero-enteric fistula between the terminal ileum and sigmoid colon (
Fig. 1C) as well as suspicions regarding another
fistula between the distal ileum (
Fig. 1D).
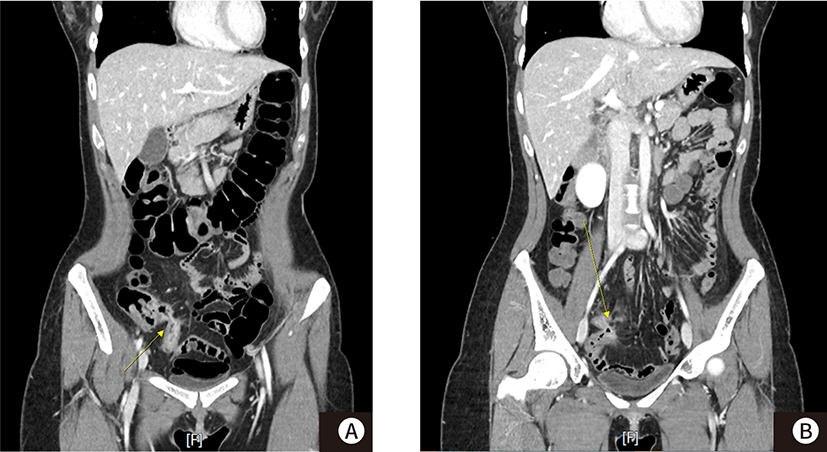
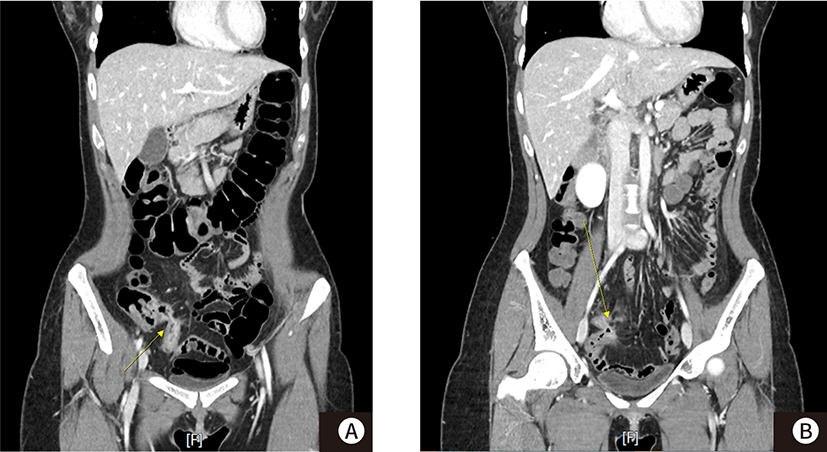
Despite conservative treatment with bowel rest and antibiotics for 2 weeks, the
patient could not tolerate the diet although abdominal pain was relieved.
Contrast-enhanced abdominopelvic CT, following conservative treatment, clearly
revealed entero-enteric fistula despite improvements in the inflammatory change in
the ileum relative to the previous magnetic resonance enterography (
Fig. 2). Hence, consultation with the surgical
department was conducted.
Fig. 1.
Colonoscopy (A,B) and magnetic resonance enterography (C,D) images. (A)
Colonoscopy shows a whitish scar with inflammatory pseudopolyps in cecum and
mild stricture is observed in ileocecal valve, (B) in terminal ileum, ulcer
with edematous mucosa and stenosis is observed, (C) the magnetic resonance
enterography shows progression of a penetrating complication that involved
distal ileum with complex entero-enteric fistula between terminal ileum and
sigmoid colon, (D) another fistula tract is suspicious between distal
ileum.
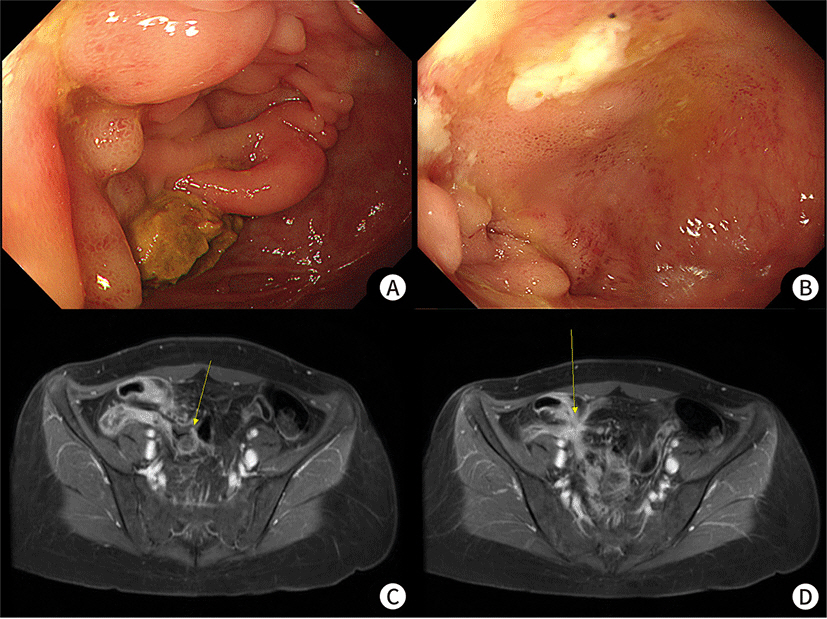
Fig. 2.
Contrast-enhanced CT image after conservative management for 2 weeks. (A)
Contrast-enhanced CT clearly reveals entero-enteric fistula despite
improvements in the inflammatory change in the ileum (B) another fistula
tract is also observed clearly.
After careful discussion on surgical treatment with the patient and her family, an
operation with the dVSP surgical system was performed. After making a vertical
umbilical skin incision of 3.5 cm, the fascia layer was opened using the open Hasson
technique. The single-port entry system was applied through the wound opening and
CO2 gas to 12 mmHg was insufflated. The patient was placed in the
Lloyd-Davies position (i.e., head-down lithotomy with hips flexed) with a steep
Trendelenburg position to expose the surgical target (right lower abdomen and
pelvis) clearly. The patient cart of the dVSP surgical system was placed on her
right side. The dVSP cannula, which consists of four channels, was inserted into the
single-port entry system. Three 6-mm robotic instruments (dVSP monopolar curved
scissor, fenestrated bipolar forceps, and Cadiere forceps), along with a 12-mm
articulating camera, were inserted into each channel. After the completion of
docking, the surgeon started to perform robotic surgery in the console. During the
console time, the assistant performed endoscopic suction, inserted suture materials
into the abdominal cavity, and stapled for distal sigmoid colon resection through
the remaining trocar of the single-port entry system.
In the operative field, severe adhesion among terminal ileum, adjacent ileum, and
sigmoid colon was observed. To clarify the exact anatomical state, adhesiolysis of
the small bowel and right colon was performed. After mobilizing the bowel, the
fistula tract between the sigmoid colon and distal ileum was identified and
resected. The hole in the sigmoid colon was closed by robotic suture. To perform
ileocecectomy, which included lesions of the distal ileum, right colon mobilization
to the hepatic flexure was conducted from the right paracolic gutter, duodenum, and
Gerota’s fascia. After completing right colon mobilization, sigmoid colon
mobilization was performed for the anterior resection, which included the fistula
tract. After medial dissection followed by lateral dissection was conducted, the
distal sigmoid colon was resected, which included the hole of the fistula tract with
a linear stapler intracorporeally administered by an assistant. The proximal sigmoid
colon was exteriorized through an umbilical incision and the anvil of the circular
stapler was inserted. The bowel was placed back into the abdominal cavity and
intracorporeal colo-colic end-to-end anastomosis was performed using a circular
stapler (Video clip). Then mobilized right colon and the small bowel were
exteriorized through an umbilical incision. Extracorporeal end-to-side anastomosis
was performed using a circular and a linear stapler after excision of bowel
mesentery with vessel sealer for devascularization. At this point, extensive small
bowel exploration was conducted to identify small bowel lesions such as obstruction
and stricture due to CD. Although multiple skipped strictures were observed in the
ileum and jejunum, strictureplasty is unnecessary because the passage was possible.
The operation was over as the drain insertion through the umbilical wound and
closure of the main wound was completed (
Fig.
3, Supplementary Video 1). Docking, console, and total operation times were
12, 200, and 260 mins, respectively. Estimated blood loss was 50 cc and
intraoperative transfusion was not necessary. Ileocecectomy and anterior resection
without lymph node dissection were performed simultaneously without any
intraoperative events.
Fig. 3.
Immediate wound postoperatively. Drain is inserted through main wound
used for single-incision robotic surgery with the da Vinci SP
system.

Diet built up in the order of clear liquid, low residue, and regular diet were 1, 2,
and 3 postoperative days, respectively. Gas passing and stool passing was detected
postoperatively after 4 days. The Foley catheter was removed postoperatively on the
first day. Intravenous patient-controlled analgesia and opioids were held on the
first postoperative day. The recovery of the patient was uneventful. She was
discharged postoperatively on the 8th day. She has been following up with a
physician for CD. During the 18-month follow-up period, the CD was well controlled
without postoperative complications.
Discussion
Ileocecal resection and primary reconstruction are the most common surgical
procedures in patients with CD of the distal ileum and/or the ileo-colon. Surgery in
CD can be challenging due to thickened and friable mesentery, enteric fistulas,
bowel perforation, and frequent occurrence of intra-abdominal abscesses. However, in
selected patients with CD, laparoscopy offers well-described short-term benefits
such as decreased pain, lower wound complication rates, earlier resumption of diet
and bowel function, better cosmesis, and shorter hospital stay [
2,
3]. In
addition, reduced formation of postoperative adhesions was useful, particularly in
young patients who are at significant risk of multiple surgeries [
6]. Moreover, Maeda et al. [
7] reported the results of single-incision
laparoscopic ileocecal resection for CD in their systematic review, suggesting that
it may be feasible and safe.
Robotic ileocecal resection has been also attempted in patients with CD. Recently,
the results of robotic surgery for CD have been published [
3–
5]. Hota et al.
[
3] analyzed and performed a retrospective
review of the National Surgical Quality Improvement Program (NSQIP) database to
select 5,158 patients with CD who underwent ileocecal resection (open, laparoscopic,
or robotic-assisted). In this analysis, the robotic group was composed of 121
patients. Though the robotic-assisted group had significantly longer operative times
relative to the laparoscopic surgery group, there was no difference in terms of the
postoperative short-term outcomes. Hande Aydinli et al. [
4] also reported the safety and feasibility of robotic ileocolic
resection for CD compared with laparoscopic approaches. This was accomplished with
no leaks, major morbidity/mortality, and comparable length of stay, with a 1-day
shorter return of bowel function and lower overall complication rates in 33 robotic
patients.
However, previous reports were performed with the two most often used robotic
platforms, the da Vinci Si and the da Vinci Xi. There has been no report on robotic
surgery with the dVSP surgical system in patients with intra-abdominal CD. We
thought that dVSP would have advantages for surgery in patients with CD than
previous version of the robotic surgical system. As we use the umbilicus for a
single-entry site, all procedures could be performed regardless of the
lesion’s location. In particular, it is possible to predict various surgical
conditions due to the disease characteristics of CD. Previous versions of robotic
systems have limitations in docking multiple devices in this situation. In addition,
re-docking is necessary to perform concomitant procedures, such as in our case. As
we used the 360° rotation of single-arm devices, we could perform surgery
without re-docking for the different workplaces. Many ports and several re-dockings
were inevitable if the operation in our case was performed with the previous version
of a robotic system or laparoscopic surgery.
Current dVSP model lacks robotic advanced energy instruments and staplers. Advanced
energy devices could help simplify the surgery and reduce the operative time.
Inflammation can cause bleeding in the mesentery, particularly in patients suffering
from CD. In addition, a robot stapler can make intracorporeal anastomosis easier.
Gunnells et al. [
8] suggested that extensive
mesenteric mobilization is not necessary in case the mesentery is intracorporeally
divided and an intracorporeal anastomosis is performed. Also, Calini et al. [
5] reported that intracorporeal anastomosis was
associated with a faster return to bowel function without any impact on the length
of stay or 30-day complications compared with extracorporeal anastomosis in patients
who underwent robotic ileocecectomy for intra-abdominal CD. The advantages of
single-incision robotic surgery can be maximized if robotic advanced energy
instruments and staplers are available.
We thought that the dVSP surgery could be performed in patients who can be adapted to
other minimally invasive surgical techniques. However, the robotic approach is
limited in terms of extensive intracorporeal small bowl explorations due to the
docking system, as opposed to the laparoscopic approach, which allows for more
freedom of port placement. In particular, dVSP has a hardness in the intracorporeal
exploration of the small bowel due to the limitation of movement, relative to
previous robotic systems. However, as in our case, if the patient does not have
adhesions and has a first-time surgery, an extracorporeal exploration can be
performed with the main wound used for trocar insertion.
In conclusion, we successfully performed simultaneous ileocecectomy and anterior
resection with the dVSP surgical system for enteric-enteric fistula in a patient
with CD. There were no intraoperative events and the patient recovered well without
any post-operative complications. To the best of our knowledge, there has been no
report on dVSP surgery in patients with intra-abdominal CD. Although more cases are
essential for evaluating the feasibility of dVSP surgery in patients with
intra-abdominal CD, it can be used in patients who can be adapted to other minimally
invasive surgical techniques.
Acknowledgements
Not applicable.
Ethics Approval and Consent to Participate
Supplementary Materials
Supplementary materials are available from: https://doi.org/10.12771/emj.2022.e16.
Supplementary Video 1. Simultaneous ileocecectomy and anterior resection with the
da Vinci SP surgical system.
References
1. Lu KC, Cone MM, Diggs BS, Rea JD, Herzig DO. Laparoscopic converted to open colectomy: predictors and outcomes
from the Nationwide Inpatient Sample. Am J Surg. 2011; 201(5):634–639. DOI:
10.1016/j.amjsurg.2011.01.009. PMID:
21545913.

2. Wan J, Liu C, Yuan XQ, Yang MQ, Wu XC, Gao RY, et al. Laparoscopy for Crohn's disease: a comprehensive
exploration of minimally invasive surgical techniques. World J Gastrointest Surg. 2021; 13(10):1190–1201. DOI:
10.4240/wjgs.v13.i10.1190. PMID:
34754387. PMCID:
PMC8554722.

3. Hota S, Parascandola S, Smith S, Tampo MM, Amdur R, Obias V. Robotic and laparoscopic surgical techniques in patients with
Crohn's disease. Surg Endosc. 2021; 35(8):4602–4608. DOI:
10.1007/s00464-020-07885-x. PMID:
32789588.

4. Hande Aydinli H, Anderson M, Hambrecht A, Bernstein MA, Grucela AL. Robotic ileocolic resection with intracorporeal anastomosis for
Crohn's disease. J Robot Surg. 2021; 15(3):465–472. DOI:
10.1007/s11701-020-01125-z. PMID:
32725327.
5. Calini G, Abdalla S, Abd El Aziz MA, Saeed HA, D'Angelo ALD, Behm KT, et al. Intracorporeal versus extracorporeal anastomosis for robotic
ileocolic resection in Crohn's disease. J Robot Surg. 2022; 16(3):601–609. DOI:
10.1007/s11701-021-01283-8. PMID:
34313950.

7. Maeda K, Nagahara H, Shibutani M, Fukuoka T, Inoue T, Ohira M. A review of reports on single-incision laparoscopic surgery for
Crohn's disease. Surg Today. 2019; 49(5):361–368. DOI:
10.1007/s00595-018-1732-x. PMID:
30805721.






 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download