Abstract
Purpose
This study was performed to investigate the role of the perioperative neutrophil-to-lymphocyte ratio (NLR) as an early predictor of major postoperative complications after total gastrectomy for gastric cancer.
Methods
This single-center, retrospective study reviewed consecutive patients with gastric cancer who underwent total gastrectomy at a single institution from March 2009 to March 2021. The postoperative complications were graded according to the Clavien-Dindo classification. We analyzed the patient demographics and surgical outcomes according to the grade of postoperative complications in the major complications group (≥grade III) and the no major complications group (<grade III and no complication). Laboratory tests were performed preoperatively and on postoperative days (POD) 2 and 5 to determine the NLR.
Results
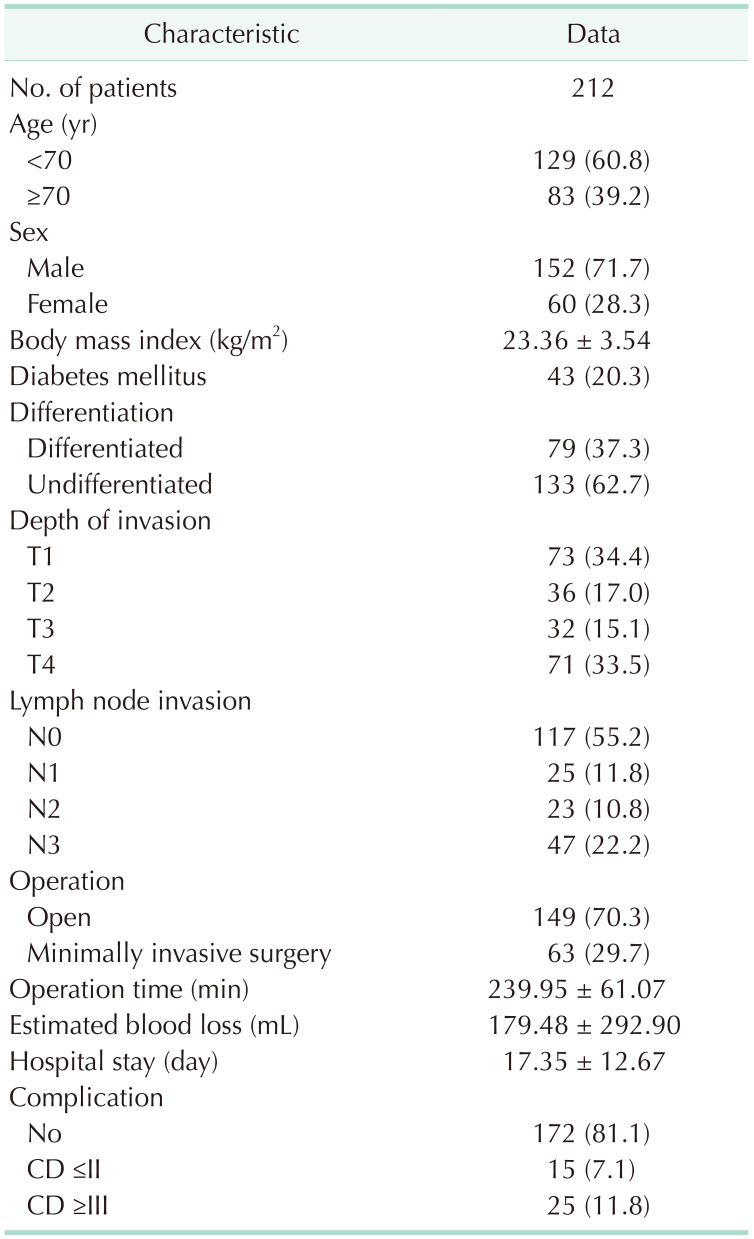
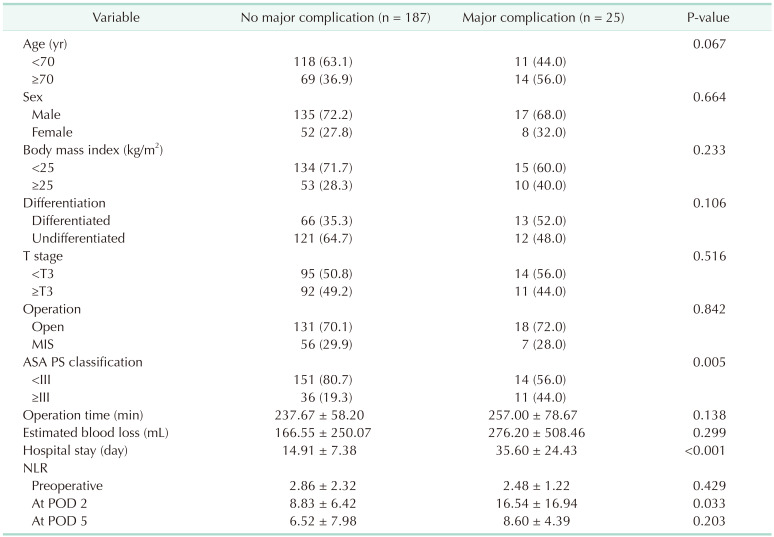
Out of 212 patients (mean age, 64.1 years; 152 male [71.7%]), 63 (29.7%) underwent minimally invasive surgery. Twenty-five (11.8%) were in the major complications group and 187 (88.2%) were in the no major complications group. There was a significant difference in the NLR on POD 2 (16.54 vs. 8.83, P = 0.033) between the 2 groups. According to the receiver operating characteristic curve for the NLR on POD 2, the cutoff was calculated to be 9.6. In multivariate analysis, an NLR on POD 2 of ≥9.6 and an American Society of Anesthesiologists physical status classification of ≥III were statistically significant predictors of major postoperative complications.
Gastric cancer is the third most common cause of cancer death worldwide, with an estimated 770,000 deaths each year [1]. Surgical resection with radical lymphadenectomy is still the standard treatment for gastric cancer, although some early gastric cancers can be treated endoscopically [2]. However, the incidence rate of postoperative complications after radical gastrectomy is somewhat frequent, ranging from 12.8% to 46% [34567]. Many studies have reported that postoperative complications were correlated with poor overall survival and recurrence-free survival after radical gastrectomy for gastric cancer [368910111213]. Therefore, it is important to investigate the predictive factors for postoperative complications and make an early diagnosis of complications to minimize the negative effect of postoperative complications on the patient’s prognosis.
Several studies have investigated the factors predictive of postoperative complications in patients who underwent radical gastrectomy. These predictive factors included cancer-related, host-related, and surgery-related factors, and systemic inflammatory response markers. However, most of the studies only confirmed preoperative and intraoperative factors [14151617].
Recently, some studies reported that postoperative systemic inflammatory biomarkers such as CRP, the neutrophil-to-lymphocyte ratio (NLR), and the platelet-to-lymphocyte ratio were also been found to be independent predictors of postoperative complications in various fields of surgery [181920]. Among these biomarkers, the NLR is the most well-known biomarker, and many previous studies have reported the predictive value of the NLR as an indicator related to cancer prognosis [2122].
However, the correlation between the NLR and postoperative complications is still unclear. Therefore, our study aimed to evaluate the role of the perioperative NLR for predicting major postoperative complications after total gastrectomy for gastric cancer.
This study was approved by the Institutional Review Board of Konyang University Hospital, and the requirement of obtaining informed consent was waived due to the retrospective study design (No. 2021-10-017).
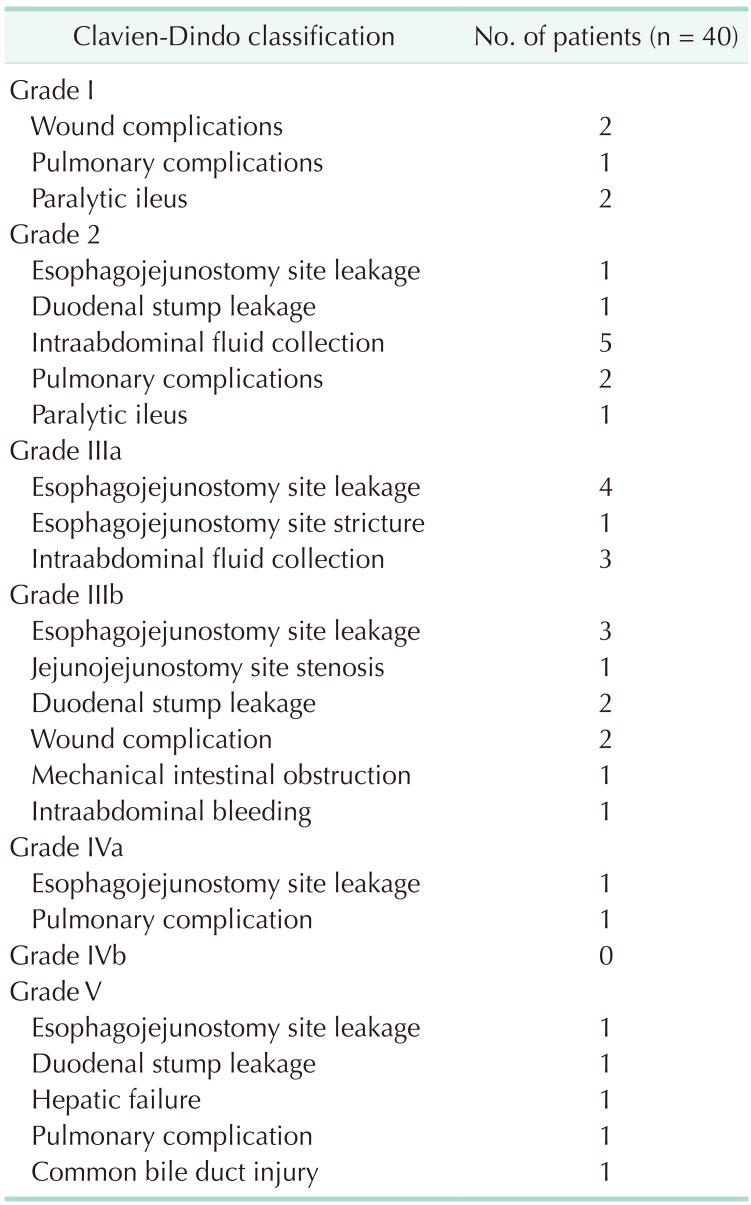
We retrospectively reviewed the data collected from patients who underwent total gastrectomy for gastric cancer at a single institution between March 2009 and March 2021. We excluded patients with a history of other malignancies and inadequate laboratory and medical records. The postoperative complications were classified according to the Clavien-Dindo classification system. The patients were divided into 2 groups according to the severity of complications; the major complications group and the no major complications group. The major complications group included patients with Clavien-Dindo classifications of III or higher, and the no major complications group included patients with Clavien-Dindo classifications of I or II and no complications. We compared their clinicopathological data and systemic inflammatory biomarkers.
Preoperative blood samples were obtained within 4 weeks before surgery, while postoperative blood samples were obtained on the day of surgery and on postoperative days (PODs) 2 and 5. The blood sample tests included WBC, neutrophil, and lymphocyte counts. The NLR was calculated as neutrophil count (number/L)/lymphocyte count (number/L).
All patients included in this study underwent total gastrectomy with Roux-en Y reconstruction. The surgical approaches including open, laparoscopic-assisted, and totally laparoscopic approaches were determined based on the patient’s abdominal surgical history, the degree of cancer progression, and the surgeon’s preferred surgical method.
Patients started water intake on POD 4. If there were no specific symptoms after water intake, the patients were started on liquid and soft diet on PODs 5 and 6, respectively. The Jackson-Pratt drain was removed on POD 6 and the patients were discharged on POD 7.
All statistical analyses were performed using IBM SPSS Statistics ver. 25.0 (IBM Corp., Armonk, NY, USA). To compare the differences between no/minor complications and major complications, the categorical variables were analyzed using the chi-square test, and the continuous variables were analyzed using the Student t-test. The ideal cutoff NLR value was calculated using receiver operating characteristic curves. Univariate and multivariate logistic regression analyses were performed to identify the predictive value for major postoperative complications. A P-value of <0.05 was considered to indicate statistical significance.
The 212 included patients and baseline patient characteristics are summarized in Table 1. Among the patients, 83 (39.2%) were over 70 years of age, and 152 (71.7%) were male. The mean body mass index (BMI) was 23.36 kg/m2. There were 43 patients (20.3%) with diabetes mellitus. Sixty-three patients (29.7%) underwent minimally invasive surgery. The mean operation time was 239 minutes and the mean estimated blood loss (EBL) was 179 mL. The mean hospital stay was 17 days. The major complications group and the no major complications group included 25 and 187 patients, respectively.
The postoperative complications are summarized in Table 2. Postoperative complications occurred in 40 patients (18.9%). Among them, 25 patients (11.8%) experienced major complications.
There were significant differences between the 2 groups in the NLR on POD 2, American Society of Anesthesiologists (ASA) physical status (PS) classification, and the duration of hospital stay. However, there were no significant differences between the 2 groups in the preoperative NLR, the NLR on POD 5, age, sex, BMI, T stage, surgical approach, operation time, and EBL (Table 3).
The area under the curve of the NLR on POD 2 was 0.723 (P < 0.001), and a cutoff value of 9.6 yielded 64.0% sensitivity and 67.9% specificity (Fig. 1).
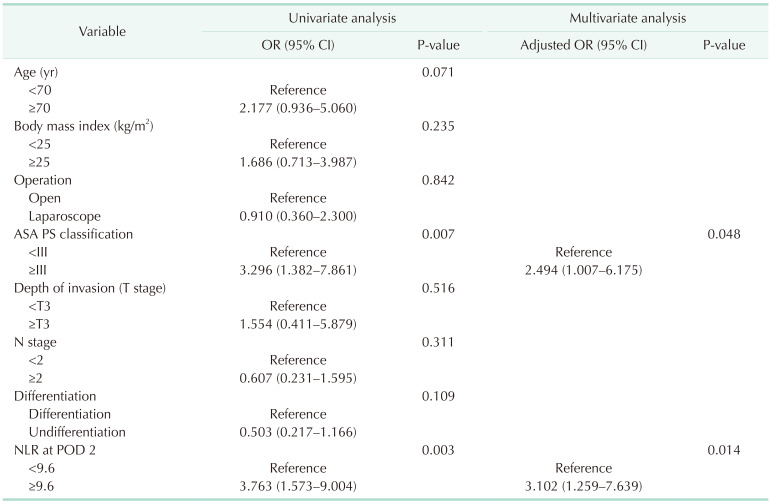
The results of univariate and multivariate analyses for factors related to major postoperative complications after total gastrectomy are shown in Table 4. In univariate analysis, an ASA PS classification of ≥III (P = 0.007) and an NLR on POD 2 of ≥9.6 (P = 0.003) were significantly associated with major postoperative complications.
In multivariate analysis, an ASA PS classification of ≥III (adjusted odds ratio [OR], 2.494; 95% confidence interval [CI], 1.007–6.175; P = 0.048) and an NLR on POD 2 of ≥9.6 (adjusted OR, 3.102; 95% CI, 1.259–7.639; P = 0.014) were significantly associated with major postoperative complications.
Several studies have identified the association between the preoperative NLR and long-term and short-term outcomes, but the association between the postoperative NLR and long-term and short-term outcomes has not yet been clearly elucidated. As a result of this study, the NLR on POD 2 and the ASA PS classification were identified as independent factors predictive of major postoperative complications. However, no significant relationship was found between major postoperative complications and the preoperative NLR and the NLR on POD 5. And there was no significant relationship between major postoperative complications and age, BMI, surgical approach, or T stage.
The NLR is the number of neutrophils divided by the number of lymphocytes. The NLR is an easily accessible value considering that the complete blood count test is a common blood test and the calculation method is easy. In physiologic stress, the secretion of endogenous cortisol and catecholamines increases the neutrophil count while decreasing the lymphocyte count, resulting in a more sensitive change in the NLR level to better reflect acute stress than other laboratory values [2324]. Therefore, many studies have been conducted to predict postoperative complications and prognosis using the perioperative NLR [17222526].
Although inflammatory markers will increase when complications occur after surgery, we need significant parameters that can predict major postoperative complications using routine laboratory tests. In this study, we investigated whether major postoperative complications could be predicted using the perioperative NLR. We found that the NLR on POD 2 was a significant predictive factor for the occurrence of major complications.
In this study, major postoperative complications occurred before POD 2 in 1 case, and reoperation was performed on the day of surgery due to operative site bleeding. The other major complications occurred after POD 2 and major complications emerged most frequently on PODs 8 and 9. Thus, the risk of major complications can be predicted by the NLR on POD 2 and if the NLR is high, the patients can be closely monitored and, when the development of a complication is suspected, immediate examinations or treatments can be performed to prevent a poor prognosis.
Our findings on the association between the NLR and the occurrence of major postoperative complications were similar to those in previous studies. Benlice et al. [25] evaluated the association between the preoperative and postoperative NLR and 30-day postoperative complications after colorectal surgery and found that an NLR on POD 2 of ≥9.2 (OR, 1.43; 95% CI, 1.03–1.98; P = 0.02) was significantly related to the development of postoperative complications.
In previous studies, the preoperative NLR and postoperative complications and prognosis were found to be related. Miyamoto et al. [26] suggested that a preoperative NLR of >3.50 was associated with a significantly increased risk of complications and poor survival. However, in our study, there was no association between the preoperative NLR and postoperative complications after gastrectomy.
ASA PS classification was identified as an independent factor related to the development of major postoperative complications in this study. Several studies also found that postoperative complications increased when the ASA PS classification was III or higher [2728]. Simões et al. [27] confirmed an ASA PS classification of ≥III (OR, 2.61; 95% CI, 1.34–5.49; P = 0.004) as a predictor of major complications in elective abdominal surgery in cancer patients.
There were several limitations associated with this study. First, as the present study was a retrospective, single-institution study, our results could be biased. Second, there are several inflammatory markers, but only NLR was considered in this study because other markers did not show significant differences in results or did not have sufficient medical records for analysis. Third, long-term surgical outcomes were not evaluated. Therefore, a further large-scale prospective study is required in the future.
According to our results, an NLR over 9.6 on POD 2 and an ASA PS classification of III or higher were independent factors predicting major complications after total gastrectomy for gastric cancer. In conclusion, we suggest that the measurement of NLR on POD 2 is simple and useful for the early prediction of major complications after total gastrectomy.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–249. PMID: 33538338.

2. Ott K, Lordick F, Blank S, Büchler M. Gastric cancer: surgery in 2011. Langenbecks Arch Surg. 2011; 396:743–758. PMID: 21234760.

3. Wang S, Xu L, Wang Q, Li J, Bai B, Li Z, et al. Postoperative complications and prognosis after radical gastrectomy for gastric cancer: a systematic review and meta-analysis of observational studies. World J Surg Oncol. 2019; 17:52. PMID: 30885211.

4. Watanabe M, Miyata H, Gotoh M, Baba H, Kimura W, Tomita N, et al. Total gastrectomy risk model: data from 20,011 Japanese patients in a nationwide internet-based database. Ann Surg. 2014; 260:1034–1039. PMID: 25072429.
5. Yasunaga H, Horiguchi H, Kuwabara K, Matsuda S, Fushimi K, Hashimoto H, et al. Outcomes after laparoscopic or open distal gastrectomy for early-stage gastric cancer: a propensity-matched analysis. Ann Surg. 2013; 257:640–646. PMID: 23023204.
6. Yu J, Hu J, Huang C, Ying M, Peng X, Wei H, et al. The impact of age and comorbidity on postoperative complications in patients with advanced gastric cancer after laparoscopic D2 gastrectomy: results from the Chinese laparoscropic gastrointestinal surgery study (CLASS) group. Eur J Surg Oncol. 2013; 39:1144–1149. PMID: 23850088.

7. Lee SE, Ryu KW, Nam BH, Lee JH, Kim YW, Yu JS, et al. Technical feasibility and safety of laparoscopy-assisted total gastrectomy in gastric cancer: a comparative study with laparoscopy-assisted distal gastrectomy. J Surg Oncol. 2009; 100:392–395. PMID: 19598150.
8. Kubota T, Hiki N, Sano T, Nomura S, Nunobe S, Kumagai K, et al. Prognostic significance of complications after curative surgery for gastric cancer. Ann Surg Oncol. 2014; 21:891–898. PMID: 24254205.

9. Li QG, Li P, Tang D, Chen J, Wang DR. Impact of postoperative complications on long-term survival after radical resection for gastric cancer. World J Gastroenterol. 2013; 19:4060–4065. PMID: 23840153.

10. Sierzega M, Kolodziejczyk P, Kulig J. Polish Gastric Cancer Study Group. Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg. 2010; 97:1035–1042. PMID: 20632269.

11. Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Terashima M. Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann Surg Oncol. 2013; 20:1575–1583. PMID: 23076557.

12. Tsujimoto H, Ichikura T, Ono S, Sugasawa H, Hiraki S, Sakamoto N, et al. Impact of postoperative infection on long-term survival after potentially curative resection for gastric cancer. Ann Surg Oncol. 2009; 16:311–318. PMID: 19037699.

13. Yoo HM, Lee HH, Shim JH, Jeon HM, Park CH, Song KY. Negative impact of leakage on survival of patients undergoing curative resection for advanced gastric cancer. J Surg Oncol. 2011; 104:734–740. PMID: 21792945.

14. Inokuchi M, Kato K, Sugita H, Otsuki S, Kojima K. Impact of comorbidities on postoperative complications in patients undergoing laparoscopy-assisted gastrectomy for gastric cancer. BMC Surg. 2014; 14:97. PMID: 25416543.

15. Kim MC, Kim W, Kim HH, Ryu SW, Ryu SY, Song KY, et al. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale korean multicenter study. Ann Surg Oncol. 2008; 15:2692–2700. PMID: 18663532.

16. Mohri Y, Tanaka K, Toiyama Y, Ohi M, Yasuda H, Inoue Y, et al. Impact of preoperative neutrophil to lymphocyte ratio and postoperative infectious complications on survival after curative gastrectomy for gastric cancer: a single institutional cohort study. Medicine (Baltimore). 2016; 95:e3125. PMID: 26986164.
17. Moyes LH, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC. Preoperative systemic inflammation predicts postoperative infectious complications in patients undergoing curative resection for colorectal cancer. Br J Cancer. 2009; 100:1236–1239. PMID: 19319134.

18. McSorley ST, Ramanathan ML, Horgan PG, McMillan DC. Postoperative C-reactive protein measurement predicts the severity of complications following surgery for colorectal cancer. Int J Colorectal Dis. 2015; 30:913–917. PMID: 25922147.

19. Jing X, Huang C, Zhou H, Li C, Fan L, Chen J, et al. Association between serum C-reactive protein value and prognosis of patients with non-small cell lung cancer: a meta-analysis. Int J Clin Exp Med. 2015; 8:10633–10639. PMID: 26379854.
20. Kim EY, Yim HW, Park CH, Song KY. C-reactive protein can be an early predictor of postoperative complications after gastrectomy for gastric cancer. Surg Endosc. 2017; 31:445–454. PMID: 27734201.

21. Zahorec R. Ratio of neutrophil to lymphocyte counts: rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001; 102:5–14. PMID: 11723675.
22. Cupp MA, Cariolou M, Tzoulaki I, Aune D, Evangelou E, Berlanga-Taylor AJ. Neutrophil to lymphocyte ratio and cancer prognosis: an umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med. 2020; 18:360. PMID: 33213430.

23. Onsrud M, Thorsby E. Influence of in vivo hydrocortisone on some human blood lymphocyte subpopulations. I. Effect on natural killer cell activity. Scand J Immunol. 1981; 13:573–579. PMID: 7313552.

24. Honda T, Uehara T, Matsumoto G, Arai S, Sugano M. Neutrophil left shift and white blood cell count as markers of bacterial infection. Clin Chim Acta. 2016; 457:46–53. PMID: 27034055.

25. Benlice C, Onder A, Babazade R, Hrabe J, Stocchi L, Steele S, et al. Is the neutrophil-to-lymphocyte ratio associated with increased morbidity after colorectal surgery? Surg Laparosc Endosc Percutan Tech. 2019; 29:36–39. PMID: 30358649.

26. Miyamoto R, Inagawa S, Sano N, Tadano S, Adachi S, Yamamoto M. The neutrophil-to-lymphocyte ratio (NLR) predicts short-term and long-term outcomes in gastric cancer patients. Eur J Surg Oncol. 2018; 44:607–612. PMID: 29478743.

27. Simões CM, Carmona MJ, Hajjar LA, Vincent JL, Landoni G, Belletti A, et al. Predictors of major complications after elective abdominal surgery in cancer patients. BMC Anesthesiol. 2018; 18:49. PMID: 29743022.

28. Jakobson T, Karjagin J, Vipp L, Padar M, Parik AH, Starkopf L, et al. Postoperative complications and mortality after major gastrointestinal surgery. Medicina (Kaunas). 2014; 50:111–117. PMID: 25172605.

Fig. 1
Receiver operating characterisitcs (ROC) curves for neutrophil-to-lymphocyte ratio on postoperative day 2 (area under the curve: 0.723, cutoff value: 9.6, P < 0.001; sensitivity: 64.0%; specificity: 67.9%).





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download