Abstract
Purpose
The objective of this study is to evaluate the effect of the coronavirus disease 2019 (COVID-19) pandemic on elective and emergent colorectal surgical practice.
Methods
The population of this retrospective observational study consisted of all consecutive patients who underwent emergent or elective colorectal surgery between March 2019 and March 2021. The patients were divided into 2 groups: the prepandemic group who were treated between March 2019 and March 10, 2020, and the pandemic group who were treated between March 11, 2020 and March 2021. The rate of emergent operations was the primary outcome. The groups were compared based on the frequency of operations, distribution of tumoral features in malignant cases, and 90th-day mortality rates.
Results
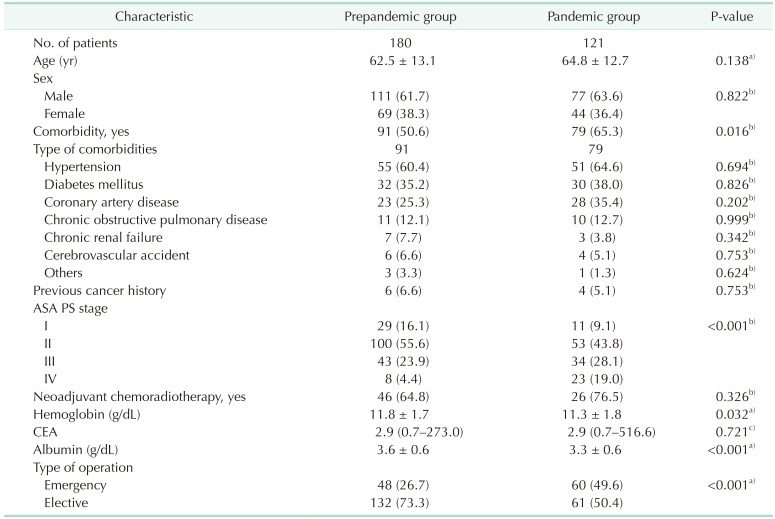
There were 180 and 121 patients in the prepandemic and pandemic groups, respectively. There were significantly more patients of the American Society of Anesthesiologists physical status stage IV with comorbidity in the pandemic group than in the prepandemic group (P = 0.016 and P < 0.001, respectively). The rate of emergent operations was significantly higher in the pandemic group than in the prepandemic group (49.6% vs. 26.7%, P < 0.001). There were significantly more patients who received non-resectional surgery in the pandemic group than in the prepandemic group (P = 0.002). Additionally, there were significantly more patients without resection among patients with a defunctioning stoma (P = 0.001). The length of hospital stay (LoS) was significantly shorter in the pandemic group than in the prepandemic group (P = 0.039). On the other hand, the mortality rate was significantly higher in the pandemic group than in the prepandemic group (15.7% vs. 6.1%, P = 0.011).
There have been significant changes in the surgical treatments of several life-threatening diseases, including colorectal emergencies and tumors, since the coronavirus disease 2019 (COVID-19) broke out [1]. The most significant change was a decrease in the general public’s access to healthcare services [1234]. The negative effect of the pandemic on the number of primary care referrals and admissions for suspected colorectal cancer has been reported [5]. It has been speculated that the decrease in the general public’s access to healthcare services might cause an increase in deaths from colorectal cancer, which would otherwise be avoidable [67].
In March 2020, the Turkish Ministry of Health declared that all elective surgical procedures would be delayed as per the precautions taken to cope with the surging coronavirus cases [8]. The diversion of healthcare resources to treat COVID-19 patients, fear of contracting the coronavirus while in hospital, and the changes in healthcare-seeking behavior of the patients who show symptoms of colorectal diseases have likely delayed and complicated the clinical presentations associated with these diseases [910]. In addition, significant changes might have occurred in the routine care of benign and malignant colorectal diseases in the colorectal surgery units [1112]. The pandemic conditions, limited healthcare resources in the colorectal surgery units, and the lockdowns might have caused many patients to be operated on who would not have been operated on otherwise [12]. As the length of this delay increases, we could expect to see more emergent presentations of both benign and malignant diseases and more advanced colorectal cancer presentations.
Changes in urgent referral or diagnostic testing of colorectal diseases may be associated with poor surgical and oncological outcomes [413]. In some healthcare institutions, an increase in the number of patients who presented with bowel obstruction has been reported leading to higher postoperative morbidity and mortality rates [13]. A comparison of the surgical activities of the colorectal surgery units during 2 different periods, that is, before the pandemic and during the pandemic, would allow the evaluation of the treatment patterns and outcomes of the surgical colorectal diseases.
In this context, it is aimed in this study to analyze the effect of the COVID-19 pandemic on elective and emergent colorectal surgical practices and to determine the changes in the emergent operations and stages of colorectal cancer cases in Turkey.
This study was carried out as a retrospective observational study. The study population comprised all consecutive patients who underwent colorectal surgery in Haydarpaşa Numune Training and Research Hospital between March 2019 and March 2021. The ethics committee approval of the study was obtained from the Haydarpaşa Numune Training and Research Hospital (No. HNEAH-KAEK 2021/50-3174). The study was carried out in accordance with the principles outlined in the Declaration of Helsinki. Written consent could not be taken from the patients due to the study’s retrospective design and the unanimity of the data.
All patients who underwent emergent or elective colorectal surgery for benign and/or malignant colorectal diseases were evaluated within the scope of the study. The patients treated between March 11, 2020 and March 2021 were classified as the pandemic group. Additionally, a control group (the prepandemic group) consisted of the patients who underwent surgical treatment between March 2019 and March 10, 2020. The cutoff date was determined based on the date the World Health Organization declared COVID-19 as a pandemic, which was also the date when the first documented COVID-19 positive case was reported in our country [814].
The COVID-19 infection status of the patients was evaluated after March 2020 using the reverse transcriptase-polymerase chain reaction analysis of the oropharyngeal and nasal swabs at the time of hospitalization.
Patient demographic characteristics such as age and sex and clinical characteristics such as comorbidities, the American Society of Anesthesiologists (ASA) physical status (PS) stage, COVID-19 infection statuses, and neoadjuvant chemotherapy histories of patients were obtained from the hospital information system and recorded. Additionally, preoperative hemoglobin and serum albumin levels, tumoral data (tumor size and location, TNM stage, diagnosis), operative characteristics (type of presentation, whether emergent or elective, surgical approach, type of colectomy, and ostomy formation), and surgical outcomes (length of stay [LoS] in the intensive care unit and hospital, postoperative in-hospital morbidity, and mortality) were recorded [15]. The Clavien-Dindo classification was used to grade the complications observed during hospitalization to determine the morbidity rate [16]. The overall mortality rate was determined at the end of the 90th postoperative day. The causes of mortality were categorized as COVID-19, surgical and medical complications. The follow-up data were obtained from the medical records of the hospital. Telephone calls were made to the patients whose follow-up examination data were not available for confirmation of their health status and to determine 90th-day mortality.
The study’s primary outcome was the rate of emergent operations in the study groups. The secondary outcomes were the frequency of operations and 90th-day mortality rates.
Descriptive statistics were expressed as mean ± standard deviation values or median values along with range depending on whether they conformed to the normal distribution. On the other hand, categorical variables were expressed as numbers and percentages. Shapiro-Wilk, Kolmogorov-Smirnov, and Anderson-Darling tests were used to determine whether the numerical variables conformed to the normal distribution.
The independent samples t-test was used to compare 2 independent groups featuring numerical variables determined to conform to the normal distribution. On the other hand, the Mann-Whitney U-test was used for variables that were determined not to conform to the normal distribution. Pearson chi-square and Fisher exact tests were used to comparing the differences between categorical variables in 2 × 2 tables. The Fisher-Freeman-Halton test was used in R × C tables.
For statistical analysis, the Jamovi project (2021), Jamovi (computer software, ver. 2.2.5.0; retrieved from https://www.Jamovi.org), and JASP (version 0.16; retrieved from https://jasp-stats.org) were used. The P-values of ≤0.05 were deemed to indicate statistical significance in all statistical analyses.
There were 180 and 121 patients in the prepandemic and pandemic groups, respectively. Eleven patients (9.1%) from the pandemic group tested positive for COVID-19. There were significant differences between the groups in demographic, clinical, and laboratory characteristics (Table 1). The age and sex distributions were similar between the groups (P = 0.138 and P = 0.822, respectively). There were significantly more ASA PS stage IV patients with comorbidity in the pandemic group than in the prepandemic group (P = 0.016 and P < 0.001, respectively). The patients in the pandemic group had significantly lower albumin levels than those in the prepandemic group (P < 0.001). The rate of emergent operations was significantly higher in the pandemic group than in the prepandemic group (49.6% vs. 26.7%, P < 0.001).
Obstruction was the most common indication for the emergent surgical treatment for both groups (70.8% in the prepandemic group and 85% in the pandemic group). More patients underwent emergent surgery for perforation in the prepandemic period (18.4% vs. 8.3%). Nevertheless, there was no significant difference in the distribution of the surgical indications for the emergent surgical treatment between the groups (P = 0.226).
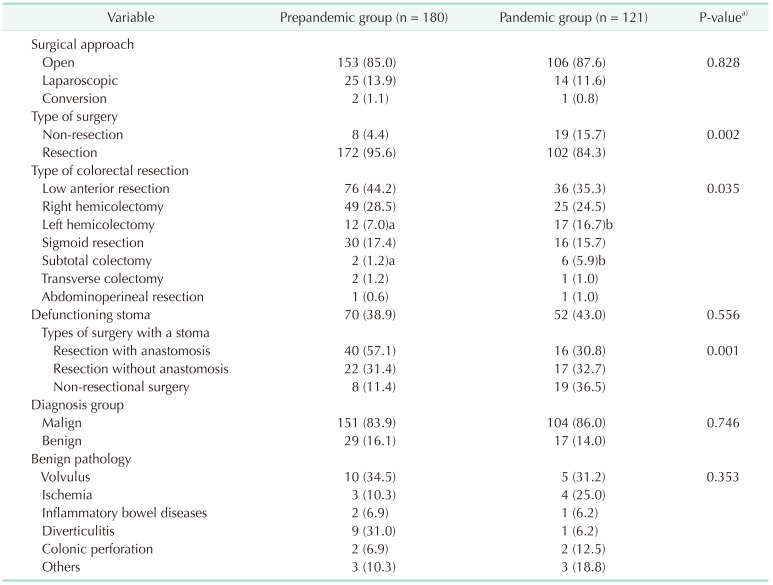
Non-resectional surgery was more frequently performed in the pandemic group (19 [15.7%] vs. 8 [4.4%], P = 0.002). Left hemicolectomy and subtotal colectomy rates were significantly higher in the pandemic group (P = 0.035). There was no difference in the rates of defunctioning stoma between the groups (38.9% vs. 43.0%, P = 0.556).
Grouping of the patients with a defunctioning stoma (n = 70) revealed a significant difference between the groups in the distribution of the patients by the type of surgery (P = 0.001). The colectomy rate with anastomosis was higher in the prepandemic group (57.1% vs. 30.8%). In association with a defunctioning stoma in all patients without resection (8 for the prepandemic group and 19 for the pandemic group), the rate of non-resectional surgery in patients with a defunctioning stoma was higher in the pandemic group (36.5% vs. 11.4%) (Table 2).
There was no significant difference between the groups in the frequency of malignant and benign pathologies (P = 0.746). In addition, the distribution of the benign pathologies did not reveal any significant difference between the groups (P = 0.353). There were no significant differences between the groups in terms of the number of patients with T, M, and TNM stages except for the number of patients with the N stage. The rate of patients with the N0 stage was higher in the prepandemic period than in the pandemic period (61.5% vs. 45.9%, P = 0.043).
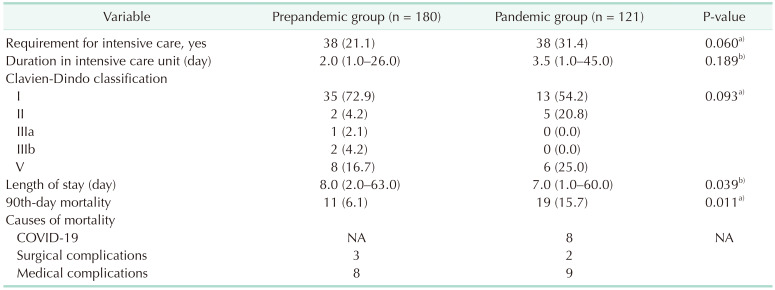
The LoS was significantly shorter in the pandemic group than in the prepandemic group (P = 0.039). The distribution of the postoperative in-hospital complications, which were determined based on the Clavien-Dindo classification, was similar between the groups (P = 0.093). The mortality rate (15.7%) was significantly higher in the pandemic group than in the prepandemic group (P = 0.011). There were 8 COVID-19–related mortalities in the pandemic group. Medical causes were seen in 8 and 9 patients in the prepandemic and pandemic groups, respectively (Table 3).
The findings of this study revealed that the incidence of emergent operations and the non-resectional type of colorectal surgical procedures with defunctioning stoma were significantly higher in the pandemic group. In addition, the mortality rate was also higher among the patients who were surgically treated during the COVID-19 pandemic period. These findings were regarded as the adverse effects of the pandemic on colorectal surgical practice.
Most of the relevant studies available in the literature addressed the outcomes of the surgical treatment of colorectal cancer cases during the COVID-19 pandemic [117181920]. In comparison, this study addressed all colorectal cases, including those with malignant and benign pathologies and those who underwent elective and emergent admissions/operations during the prepandemic and pandemic periods. Additionally, the tumoral features of the cases were also analyzed in this study. A similar methodology was used in a study by Sobrado et al. [21], in which they evaluated the elective colorectal surgical procedures used during the COVID-19 pandemic. In said study, the malignant cases comprised the majority (90.9%) of cases. They concluded that it is safe to perform elective colorectal surgical procedures during the pandemic period provided that the necessary precautions are taken. In this context, this study’s authors believed that investigating both malignant and benign cases would reflect a better picture of the changes in colorectal surgical practice during the COVID-19 pandemic period.
The COVID-19 pandemic likely caused some diversions in surgical approaches. In parallel, significant changes were observed in this study in the number of emergent presentations and the type of surgical approaches, including non-resectional colorectal operations and stoma formation. This result contradicts some of the relevant results reported in the literature [4101322]. It has also been reported that the use of laparoscopy decreased significantly during the pandemic period [49192022]. The belief that there is a risk of becoming infected with COVID-19 during laparoscopic procedures has been regarded as the primary reason for its avoidance during the pandemic period, even though it is not based on scientific evidence [17]. The finding of the relatively lower laparoscopy rates in all colorectal operations performed during the prepandemic period in this study might be another reason for the similar rates of laparoscopy observed in the study groups, contrary to some of the relevant results reported in the literature [1017].
In a national cohort study carried out in Ireland, Donlon et al. [19] reported a considerable decrease in operations without an increase in the defunctioning stomas. In comparison, there were more patients with non-resectional colorectal procedures in this study with a higher rate of defunctioning stoma formation. Similar to the findings of this study, a substantial shift from anterior resection with anastomosis toward Hartmann’s procedure with a colostomy for rectal cancer was shown in another study [9]. The healthcare systems were overwhelmed by the unexpected and unplanned hospital admissions due to the surge in the number of COVID-19 cases. Accordingly, it is essential that the characteristics of the respective patient population and the overall healthcare system of the respective country are considered while evaluating such findings.
The histopathological upstaging of colorectal cancer is another issue that has been speculated to be associated with delays in recognizing the symptoms of colorectal cancer, its diagnosis, and colorectal cancer surgery during the pandemic period [113182324]. In Uyan et al.’s study [1], for instance, the authors found higher rates of emergency operations and more patients with N and M stages for colorectal cancer during the COVID-19 pandemic. They speculated that the increase in the number of advanced cancer cases was associated with the pandemic [1]. Along these lines, Choi et al. [4] demonstrated that surgical aggressiveness, including combined multiorgan resections, was associated with the pandemic. In comparison, there were no significant differences between the groups in terms of the stages of colorectal cancer in this study. Similar findings have been reported by others [41825]. For instance, in Lim et al.’s study [25], the rates of stage IV colorectal cancer cases in the prepandemic and pandemic groups were comparable. Nevertheless, they detected more stage IV patients with initially unresectable tumors. They concluded that disease progression and delayed diagnosis were frequent during the COVID-19 pandemic. No correlations were found in this study between the variables that were determined to be significantly different between the study groups, i.e., the higher rates of emergent operations, non-resectional procedures with a defunctioning stoma, mortality, and similar tumor stages. Hence, it may be that other patient- and tumor-related factors may be the reason for these significant differences. A balanced approach should be used to weigh the risk of surgery against the delay in diagnosis and treatment [17].
The postoperative mortality rate in COVID-19 patients remains controversial [419]. There are considerable methodological differences between the studies that evaluated the mortality outcomes during the pandemic [4]. Previous studies failed to show clinically significant changes in postoperative morbidity and mortality rates, except for a few studies which reported slightly higher 30th-day surgical mortality rates [1720]. Kuryba et al. [9] reported that the already high surgical mortality rates following the elective resections for colorectal cancer increased even more in the case of emergency resections for colorectal cancer. Similarly, an increase was observed in the mortality rate during the pandemic period in this study. Given the study’s retrospective design, the number of positive COVID-19 cases was not enough to investigate the effect of COVID-19 on the mortality rates. The delayed presentations likely led to a higher number of emergent operations and poorer prognosis, which caused an increase in the comorbidity rates and the number of ASA PS stage IV patients, resulting in an increase in the mortality rates. Therefore, large-scale studies are needed to elucidate the effect of the pandemic on postoperative mortality rates following colorectal surgery.
The retrospective design in a single institution was a major limitation of the study. Then again, retrospective studies conducted during the pandemic period also have some inherent limitations. The findings of this study pertained only to the first wave of the COVID-19 pandemic. Depending on the various waves of the pandemic, there might be different trends for patients and global health care in each country regarding the pandemic. Additionally, each country has different characteristics. Hence, the results of this study may not be generalized to larger populations [626]. The relatively small sample size was another limitation limiting the significance levels of the findings. We also did not evaluate the impact of COVID-19 infection on the mortality due to the lack of prospective data.
All the benign and malignant colorectal pathologies were included in the cohort of this study. In this way, the aim was to assess the effect of the COVID-19 pandemic on the overall colorectal surgery practices. The relationship between appendectomy due to acute appendicitis and the COVID-19 pandemic has been previously investigated in the literature. However, such cases were not included in this study [27].
In conclusion, it was determined that the COVID-19 pandemic had significantly affected colorectal surgical practices, leading to more frequent emergent operations and non-resectional procedures with stoma formation. Additionally, the mortality rates increased dramatically during the pandemic. Large-scale multi-center studies with a more extended observation period are needed to corroborate the negative effect of the COVID-19 pandemic found in this study on colorectal surgical practices.
References
1. Uyan M, Özdemir A, Kalcan S, Tomas K, Demiral G, Pergel A, et al. Effects of COVID-19 pandemic on colorectal cancer surgery. Sao Paulo Med J. 2022; 140:244–249. PMID: 34586288.

2. Lui T, Leung K, Guo CG, Tsui V, Wu JT, Leung WK. Impacts of the coronavirus 2019 pandemic on gastrointestinal endoscopy volume and diagnosis of gastric and colorectal cancers: a population-based study. Gastroenterology. 2020; 159:1164–1166. PMID: 32425228.
3. D’Ovidio V, Lucidi C, Bruno G, Lisi D, Miglioresi L, Bazuro ME. Impact of COVID-19 pandemic on colorectal cancer screening program. Clin Colorectal Cancer. 2021; 20:e5–e11. PMID: 32868231.

4. Choi JY, Park IJ, Lee HG, Cho E, Kim YI, Kim CW, et al. Impact of the COVID-19 pandemic on surgical treatment patterns for colorectal cancer in a tertiary medical facility in Korea. Cancers (Basel). 2021; 13:2221. PMID: 34066390.
5. De Vincentiis L, Carr RA, Mariani MP, Ferrara G. Cancer diagnostic rates during the 2020 ‘lockdown’, due to COVID-19 pandemic, compared with the 2018-2019: an audit study from cellular pathology. J Clin Pathol. 2021; 74:187–189. PMID: 32561524.

6. Boyle JM, Kuryba A, Blake HA, Aggarwal A, van der Meulen J, Walker K, et al. The impact of the first peak of the COVID-19 pandemic on colorectal cancer services in England and Wales: a national survey. Colorectal Dis. 2021; 23:1733–1744. PMID: 33686679.

7. Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020; 21:1023–1034. PMID: 32702310.

8. Ministry of Health, Republic of Turkey (MoH-TR). COVID-19 web page of the Republic of Turkey [Internet]. Ankara: MoH-TR;2020. cited 2021 Dec 20. Available from: https://covid19.saglik.gov.tr/TR-66494/pandemi.html
.
9. Kuryba A, Boyle JM, Blake HA, Aggarwal A, van der Meulen J, Braun M, et al. Surgical treatment and outcomes of colorectal cancer patients during the COVID-19 pandemic: a national population-based study in England. Ann Surg Open. 2021; 2:e071. PMID: 34240077.

10. Xu Y, Huang ZH, Zheng CZ, Li C, Zhang YQ, Guo TA, et al. The impact of COVID-19 pandemic on colorectal cancer patients: a single-center retrospective study. BMC Gastroenterol. 2021; 21:185. PMID: 33879095.

11. Foo FJ, Ho L, Tan WJ, Koh FH, Sivarajah SS, Park SY, et al. Colorectal cancer surgery in Asia during the COVID-19 pandemic: a tale of 3 cities. Asian J Surg. 2022; 45:1095–1100. PMID: 34483046.

12. de la Portilla de Juan F, Reyes Díaz ML, Ramallo Solía I. Impact of the pandemic on surgical activity in colorectal cancer in Spain. Results of a national survey. Cir Esp (Engl Ed). 2021; 99:500–505. PMID: 34210653.

13. Shinkwin M, Silva L, Vogel I, Reeves N, Cornish J, Horwood J, et al. COVID-19 and the emergency presentation of colorectal cancer. Colorectal Dis. 2021; 23:2014–2019. PMID: 33793063.

14. World Health Organization (WHO). WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. Geneva: WHO;2020. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
.
15. Tong GJ, Zhang GY, Liu J, Zheng ZZ, Chen Y, Niu PP, et al. Comparison of the eighth version of the American Joint Committee on Cancer manual to the seventh version for colorectal cancer: a retrospective review of our data. World J Clin Oncol. 2018; 9:148–161. PMID: 30425940.

16. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.
17. Smith HG, Jensen KK, Jørgensen LN, Krarup PM. Impact of the COVID-19 pandemic on the management of colorectal cancer in Denmark. BJS Open. 2021; 5:zrab108. PMID: 34755189.

18. Polson R, Abdelqader B, Chung WY, Sangal S. Impact of the COVID-19 pandemic on early outcomes after colorectal cancer surgery. Br J Surg. 2021; 108:e398–e399. PMID: 34672322.

19. Donlon NE, Hayes C, Davern M, Bolger JC, Irwin SC, Butt WT, et al. Impact of COVID-19 on the diagnosis and surgical treatment of colorectal cancer: a national perspective. Dis Colon Rectum. 2021; 64:1305–1309. PMID: 34623346.

20. Rashid MU, Raza SS, Thomas P, Vakis S. Comparison of colorectal cancer surgery services during COVID-19 first wave with pre-COVID time. Cureus. 2021; 13:e17585. PMID: 34522556.

21. Sobrado LF, Nahas C, Marques C, Cotti G, Imperiale AR, Averbach P, et al. Is it safe to perform elective colorectal surgical procedures during the COVID-19 pandemic? A single institution experience with 103 patients. Clinics (Sao Paulo). 2021; 76:e2507. PMID: 33787677.

22. Morris E, Goldacre R, Spata E, Mafham M, Finan PJ, Shelton J, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021; 6:199–208. PMID: 33453763.

23. Manlubatan S, Lopez M, Onglao M, Monroy Iii HJ. Modifications to treatment plan of rectal cancer in response to COVID-19 at the Philippine general hospital. Ann Coloproctol. 2021; 37:225–231. PMID: 34364319.

24. Peltrini R, Imperatore N, Di Nuzzo MM, D’Ambra M, Bracale U, Corcione F. Effects of the first and second wave of the COVID-19 pandemic on patients with colorectal cancer: what has really changed in the outcomes? Br J Surg. 2021; 108:e365–e366. PMID: 34476460.

25. Lim JH, Lee WY, Yun SH, Kim HC, Cho YB, Huh JW, et al. Has the COVID-19 pandemic caused upshifting in colorectal cancer stage? Ann Coloproctol. 2021; 37:253–258. PMID: 34376026.

26. Tschann P, Girotti P, Lechner D, Adler S, Feurstein B, Szeverinski P, et al. How does the COVID-19 pandemic influence surgical case load and histological outcome for colorectal cancer? A single-centre experience. J Gastrointest Surg. 2021; 25:2957–2960. PMID: 33852126.

27. Kim CW, Lee SH. Impact of COVID-19 on the care of acute appendicitis: a single-center experience in Korea. Ann Surg Treat Res. 2021; 101:240–246. PMID: 34692596.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download