1. Central Disease Control Headquarters. COVID-19 occurence status. Updated 2022. Accessed January 10, 2022.
http://ncov.mohw.go.kr/en/
.
2. Lee JB, Jung M, Kim JH, Kim BH, Kim Y, Kim YS, et al. Guidelines for cancer care during the COVID-19 pandemic in South Korea. Cancer Res Treat. 2021; 53(2):323–329. PMID:
33721486.

3. Neal RD, Nekhlyudov L, Wheatstone P, Koczwara B. Cancer care during and after the pandemic. BMJ. 2020; 370:m2622. PMID:
32616512.

4. Carlos RC, Lowry KP, Sadigh G. The coronavirus disease 2019 (COVID-19) pandemic: a patient-centered model of systemic shock and cancer care adherence. J Am Coll Radiol. 2020; 17(7):927–930. PMID:
32631494.

5. Kim K, Kim H, Lee J, Cho IK, Ahn MH, Son KY, et al. Functional impairments in the mental health, depression and anxiety related to the viral epidemic, and disruption in healthcare service utilization among cancer patients in the COVID-19 pandemic era. Cancer Res Treat. 2022; 54(3):671–679. PMID:
34583461.

6. Chen G, Wu Q, Jiang H, Zhang H, Peng J, Hu J, et al. Fear of disease progression and psychological stress in cancer patients under the outbreak of COVID-19. Psychooncology. 2020; 29(9):1395–1398. PMID:
32596867.

7. Musche V, Bauerle A, Steinbach J, Schweda A, Hetkamp M, Weismuller B, et al. COVID-19-related fear and health-related safety behavior in oncological patients. Front Psychol. 2020; 11:1984. PMID:
32903780.

8. Gultekin M, Ak S, Ayhan A, Strojna A, Pletnev A, Fagotti A, et al. Perspectives, fears and expectations of patients with gynaecological cancers during the COVID-19 pandemic: a Pan-European study of the European Network of Gynaecological Cancer Advocacy Groups (ENGAGe). Cancer Med. 2021; 10(1):208–219. PMID:
33205595.

9. The Lancet Oncology. COVID-19: global consequences for oncology. Lancet Oncol. 2020; 21(4):467. PMID:
32240603.
10. Ciążyńska M, Pabianek M, Szczepaniak K, Ułańska M, Skibińska M, Owczarek W, et al. Quality of life of cancer patients during coronavirus disease (COVID-19) pandemic. Psychooncology. 2020; 29(9):1377–1379. PMID:
32779778.

11. Sarkar S, Scherwath A, Schirmer L, Schulz-Kindermann F, Neumann K, Kruse M, et al. Fear of recurrence and its impact on quality of life in patients with hematological cancers in the course of allogeneic hematopoietic SCT. Bone Marrow Transplant. 2014; 49(9):1217–1222. PMID:
25000458.

12. Shim EJ, Shin YW, Oh DY, Hahm BJ. Increased fear of progression in cancer patients with recurrence. Gen Hosp Psychiatry. 2010; 32(2):169–175. PMID:
20302991.

13. Feder A, Nestler EJ, Charney DS. Psychobiology and molecular genetics of resilience. Nat Rev Neurosci. 2009; 10(6):446–457. PMID:
19455174.

14. Davidson RJ, McEwen BS. Social influences on neuroplasticity: stress and interventions to promote well-being. Nat Neurosci. 2012; 15(5):689–695. PMID:
22534579.

15. Linden W, Vodermaier A, Mackenzie R, Greig D. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord. 2012; 141(2-3):343–351. PMID:
22727334.

16. Kim H, Park CH, Kim Y, Joo Y. Correlates of psychological distress in patients with cancer at a psycho-oncology clinic. J Acad Consult Liaison Psychiatry. 2021; 62(6):595–605. PMID:
34245944.

17. Mancini AD, Bonanno GA. Predictors and parameters of resilience to loss: toward an individual differences model. J Pers. 2009; 77(6):1805–1832. PMID:
19807863.

18. Somasundaram RO, Devamani KA. A comparative study on resilience, perceived social support and hopelessness among cancer patients treated with curative and palliative care. Indian J Palliat Care. 2016; 22(2):135–140. PMID:
27162423.

19. Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol. 2002; 53(1):215–243. PMID:
11752485.

20. Harvey AG, Sharpley AL, Ree MJ, Stinson K, Clark DM. An open trial of cognitive therapy for chronic insomnia. Behav Res Ther. 2007; 45(10):2491–2501. PMID:
17583673.

21. Morin CM, Vallières A, Guay B, Ivers H, Savard J, Mérette C, et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial. JAMA. 2009; 301(19):2005–2015. PMID:
19454639.

22. Janati Idrissi A, Lamkaddem A, Benouajjit A, Ben El Bouaazzaoui M, El Houari F, Alami M, et al. Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep Med. 2020; 74:248–253. PMID:
32862008.

23. Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part II: Immunologic effects. J Clin Oncol. 2005; 23(25):6097–6106. PMID:
16135476.

24. Herschbach P, Berg P, Dankert A, Duran G, Engst-Hastreiter U, Waadt S, et al. Fear of progression in chronic diseases: psychometric properties of the fear of progression questionnaire. J Psychosom Res. 2005; 58(6):505–511. PMID:
16125517.
25. Kwakkenbos L, van den Hoogen FH, Custers J, Prins J, Vonk MC, van Lankveld WG, et al. Validity of the Fear of Progression Questionnaire-Short Form in patients with systemic sclerosis. Arthritis Care Res (Hoboken). 2012; 64(6):930–934. PMID:
22262505.

26. Mehnert A, Herschbach P, Berg P, Henrich G, Koch U. Fear of progression in breast cancer patients--validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Z Psychosom Med Psychother. 2006; 52(3):274–288. PMID:
17156600.
27. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16(9):606–613. PMID:
11556941.
29. Chung S, Ahn MH, Lee S, Kang S, Suh S, Shin YW. The Stress and Anxiety to Viral Epidemics-6 Items (SAVE-6) scale: a new instrument for assessing the anxiety response of general population to the viral epidemic during the COVID-19 pandemic. Front Psychol. 2021; 12:669606. PMID:
34149565.

30. Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001; 2(4):297–307. PMID:
11438246.

31. Cho YW, Song ML, Morin CM. Validation of a Korean version of the Insomnia Severity Index. J Clin Neurol. 2014; 10(3):210–215. PMID:
25045373.

32. Temel JS, Pirl WF, Recklitis CJ, Cashavelly B, Lynch TJ. Feasibility and validity of a one-item fatigue screen in a thoracic oncology clinic. J Thorac Oncol. 2006; 1(5):454–459. PMID:
17409899.
33. Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003; 10(4):390–392. PMID:
12670856.

34. Vaishnavi S, Connor K, Davidson JR. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatry Res. 2007; 152(2-3):293–297. PMID:
17459488.

35. Chung S, Youn S, Choi B. Assessment of cancer-related dysfunctional beliefs about sleep for evaluating sleep disturbance in cancer patients. Sleep Med Rev. 2017; 8(2):98–101.

36. Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013; 7(3):300–322. PMID:
23475398.

37. Lebel S, Ozakinci G, Humphris G, Mutsaers B, Thewes B, Prins J, et al. From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support Care Cancer. 2016; 24(8):3265–3268. PMID:
27169703.

38. Kállay É, Medrea F, Dégi CL. On top of that all, now Covid-19, too. A scoping review of specificities and correlates of fear of cancer recurrence in breast cancer patients during COVID-19. Breast. 2022; 62:123–134. PMID:
35176683.

39. Simonelli LE, Siegel SD, Duffy NM. Fear of cancer recurrence: a theoretical review and its relevance for clinical presentation and management. Psychooncology. 2017; 26(10):1444–1454. PMID:
27246348.

40. Crist JV, Grunfeld EA. Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psychooncology. 2013; 22(5):978–986. PMID:
22674873.

41. van den Beuken-van Everdingen MH, Peters ML, de Rijke JM, Schouten HC, van Kleef M, Patijn J. Concerns of former breast cancer patients about disease recurrence: a validation and prevalence study. Psychooncology. 2008; 17(11):1137–1145. PMID:
18484568.

42. Pedersen AF, Rossen P, Olesen F, von der Maase H, Vedsted P. Fear of recurrence and causal attributions in long-term survivors of testicular cancer. Psychooncology. 2012; 21(11):1222–1228. PMID:
21919117.
43. Urbaniec OA, Collins K, Denson LA, Whitford HS. Gynecological cancer survivors: assessment of psychological distress and unmet supportive care needs. J Psychosoc Oncol. 2011; 29(5):534–551. PMID:
21882933.

44. Soriano EC, Perndorfer C, Otto AK, Fenech AL, Siegel SD, Dickson-Witmer D, et al. Psychosocial impact of cancer care disruptions in women with breast cancer during the COVID-19 pandemic. Front Psychol. 2021; 12:662339. PMID:
34194367.

45. Huang J, Song P, Hang K, Chen Z, Zhu Z, Zhang Y, et al. Sleep. Front Immunol. 2021; 12:727959. PMID:
34539666.
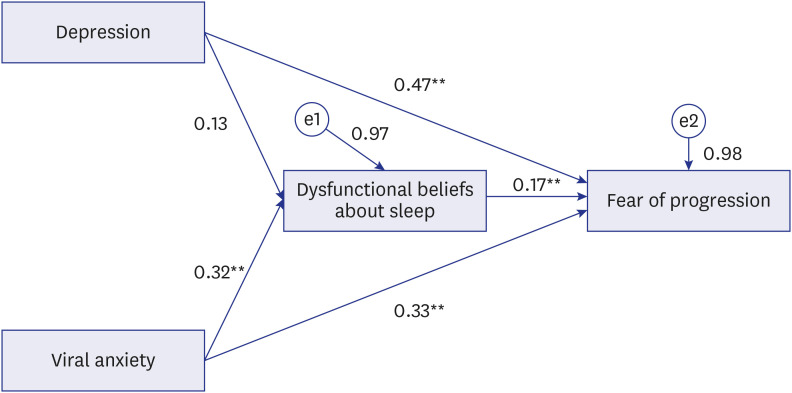
46. Kim I, Yi K, Lee J, Kim K, Youn S, Suh S, et al. Dysfunctional Beliefs about sleep in cancer patients can mediate the effect of fear of progression on insomnia. Sleep Med Rev. 2019; 10(2):83–89.

47. Youn S, Kim C, Lee J, Yeo S, Suh S, Chung S. Development of dysfunctional beliefs and attitude about sleep scale for cancer patients. Behav Sleep Med. 2020; 18(3):287–297. PMID:
30789064.

48. Lee LY, Cazier JB, Angelis V, Arnold R, Bisht V, Campton NA, et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020; 395(10241):1919–1926. PMID:
32473682.

49. Sutcuoglu O, Yazici O, Ozet A, Ozdemir N. Harmful consequences of COVID-19 fear in patients with cancer. BMJ Support Palliat Care. Forthcoming. 2020; DOI:
10.1136/bmjspcare-2020-002628.
50. Güç ZG, Alacacıoğlu A, Yazır MG, Kalender ME, Ünal S, Oflazoğlu U, et al. Being a cancer patient during the time of COVID-19: impact of the pandemic on the anxiety and the sleeping quality of oncology patients. Chemotherapy. 2022; 67(1):29–36. PMID:
34875660.

51. Yeo S, Yi K, Kim C, Lee J, Youn S, Suh S, et al. Cancer-related dysfunctional beliefs about sleep may influence insomnia of cancer patients regardless of depressive symptoms. Sleep Med Rev. 2019; 10(1):31–35.

52. Krebs J, Wasner S, Egloffstein S, Lux MP, Morawa E, Beckmann MW, et al. Resilience, fear of progression and psychosocial distress in patients with breast cancer and gynecological tumors seeking a second opinion. Psychother Psychosom Med Psychol. 2019; 69(7):293–300. PMID:
30326537.

53. Koral L, Cirak Y. The relationships between fear of cancer recurrence, spiritual well-being and psychological resilience in non-metastatic breast cancer survivors during the COVID-19 outbreak. Psychooncology. 2021; 30(10):1765–1772. PMID:
33982371.

54. Wollny AI, Jacobs I. Validity and reliability of the German versions of the CD-RISC-10 and CD-RISC-2. Curr Psychol. Forthcoming. 2021; DOI:
10.1007/s12144-021-01670-2.

55. Ahn MH, Lee J, Suh S, Lee S, Kim HJ, Shin YW, et al. Application of the Stress and Anxiety to Viral Epidemics-6 (SAVE-6) and Coronavirus Anxiety Scale (CAS) to measure anxiety in cancer patient in response to COVID-19. Front Psychol. 2020; 11:604441. PMID:
33329275.

56. Kim SY, Kim S. Do COVID-19-related treatment changes influence fear of cancer recurrence, anxiety, and depression in breast cancer patients? Cancer Nurs. 2022; 45(2):E628–E638. PMID:
33654008.

57. Latella LE, Rogers M, Leventhal H, Parker PA, Horwitz S, Matasar MJ, et al. Fear of cancer recurrence in lymphoma survivors: a descriptive study. J Psychosoc Oncol. 2020; 38(3):251–271. PMID:
31617830.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download