INTRODUCTION
Iliac artery disease affects up to half of all patients with lower extremity artery disease,
1) and revascularization is needed for symptom relief or limb salvage. Compared with surgical treatment, endovascular therapy (EVT) has the advantages of lower invasiveness and reduced periprocedural morbidity and mortality.
2) Given improved endovascular instruments and techniques, EVT is now widely adopted for iliac artery revascularization.
2)3) Iliac artery lesions are commonly classified into different extent categories according to the 2007 Trans-Atlantic Inter-Society Consensus (TASC) for the management of peripheral arterial disease II guidelines.
4) Recent studies demonstrated favorable outcomes of EVT, even for complex iliac artery lesions.
5)6) The latest guidelines recommend EVT as the first-line treatment for TASC A, B, and C lesions and as an alternative option for TASC D lesions in patients with high perioperative surgical risk.
3)7) However, there are still limited long-term data on EVT performance for the iliac artery, especially for TASC D lesions. In this study, we investigated the 5-year outcomes of EVT for iliac artery disease according to the TASC II lesion classifications.
METHODS
Ethical statement
The study protocol was approved by the Institutional Review Board (IRB) of each hospital and was conducted according to the principles of the Declaration of Helsinki as revised in 2013 (Yonsei University Health System, Severance Hospital, IRB approval number: 4-2013-0463). The IRBs of the participating hospitals waived the requirement of informed consent due to the retrospective nature of this study.
Study population
The Korean Vascular Intervention Society (K-VIS) Endovascular Therapy in Lower Limb Artery Diseases (ELLA) registry is a multicenter observational study with retrospective and prospective cohorts of patients with lower extremity artery disease treated with EVT (ClinicalTrials.gov
NCT02748226). Among patients treated with EVT in 31 hospitals in Korea between January 2006 and July 2015, a total of 3,076 patients with 3,972 limbs from the retrospective cohort of the K-VIS ELLA registry were enrolled for the analysis. The K-VIS ELLA registry study design and results have been described in detail previously.
8) Among them, 1,425 patients underwent iliac EVT in 1,766 limbs in presence of symptoms such as intermittent claudication, rest ischemic pain or tissue loss, and narrowing of a iliac artery in the symptomatic limb ≥ 50%.
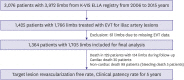
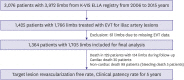
After excluding 61 limbs missing detailed EVT data, 1,364 patients with 1,705 limbs were included in the current analysis (
Figure 1). The baseline clinical and lesion characteristics, procedural data, and follow-up outcomes were collected from electronic medical records. Treatment strategies including procedural approach, wiring techniques, selection of balloons and stent types, and medications were left at the operator’s discretion.
Figure 1
Study flowchart.
EVT = endovascular therapy; K-VIS ELLA = Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases.
Endovascular therapy
Dual anti-platelet therapy (aspirin 100 mg/day and clopidogrel 75 mg/day) was commonly administered prior to the procedure. All procedures were performed under local anesthesia at the puncture site with intravenous sedation as needed. Systemic heparin (50–100 U/kg) was administered to achieve an activated clotting time up to 250 seconds. Either ipsilateral or contralateral femoral or brachial puncture was performed, depending on the target lesion location(s). The choice of intraluminal or subintimal approach was left to the operator’s wiring status. For the intraluminal approach, various 0.014-, 0.018-, and 0.035-inch guidewires were chosen according to lesion characteristics and operator preference. The 0.018–0.035-inch hydrophilic guidewires for the subintimal approach were used to create the subintimal channel with forming loop and advanced distally with support of a 4–5 Fr. Catheter or a microcatheter until the wire re-entered the true lumen at the distal stump. We considered wire passage to be subintimal when the tip of the advance wire formed a loop and when linear or spiral dissections were visible at the proximal and distal stump. After crossing the target lesion with wires, pre-dilatation was routinely performed. Lesions with residual stenosis >30% or flow-limiting dissections after pre-dilatation required stent implantation. The choice of self- or balloon-expandable stents was left to the operator’s discretion. In general, balloon-expandable stents were favored in common iliac artery (CIA) lesions, whereas self-expanding stents were chosen for long lesions involving the external iliac artery (EIA). In case of iliac rupture, a covered stent was inserted after attempting balloon tamponade.
Definitions and outcomes
Target lesions of iliac arteries were grouped using the TASC II classifications.
4) Technical success was defined as successful revascularization with residual stenosis <30% after EVT and absence of flow-limiting dissection. A major complication was defined as any clinical event that was fatal or required surgical management within 30 days of the procedure. The primary endpoint was freedom from target lesion revascularization (TLR) at 5 years stratified according to the TASC II classification. TLR was defined as any surgical or EVT at the target lesion after the index procedure. The secondary endpoint was primary clinical patency defined as freedom from symptom aggravation by at least one Rutherford category change combined with a decrease in ankle brachial index (ABI) to >0.15 or with the presence of restenosis (≥50%) on imaging studies such as duplex ultrasound, computed tomographic angiography, or intra-arterial angiography. For duplex ultrasound, peak velocity ≥180 cm/s or a lesion/adjacent-segment velocity ratio ≥2.4 was considered to indicate significant (≥50%) restenosis.
Statistical analyses
Normally distributed continuous variables are expressed as mean ± standard deviation, and categorical variables are expressed as number and percentage. The cumulative incidences of clinical events including TLR-free rates and clinical patency are presented as Kaplan-Meier estimates and were compared with log-rank tests. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using the Cox proportional hazards model to compare the risk of adverse events between TASC A, B, C, and D lesion types. The predictors for TLR were evaluated using multivariate analysis of the Cox proportional hazard regression model. All variables with p<0.20 in univariate analysis and generally known to affect TLR were included in the multivariate analysis model. Differences were considered significant at p<0.05 was considered significant. All statistical analyses were performed using the R statistical software (version 3.4.0; R Foundation for Statistical Computing, Vienna, Austria) and IBM SPSS 25.0 for Windows (IBM, Armonk, NY, USA).
DISCUSSION
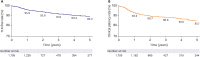
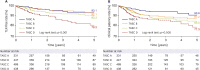
This study investigated 5-year clinical outcomes in patients treated with EVT for iliac artery disease from the multicenter retrospective cohort of the K-VIS ELLA registry according to the TASC classifications. The main findings of the study were as follows. 1) Iliac artery EVT showed 89.2% 5-year TLR-free survival and 85.1% clinical patency. 2) TASC D showed lower TLR-free survival and clinical patency compared to TASC A, B, C. However, despite lesion complexity, EVT in TASC D showed excellent procedural success (95.7%) and favorable 5-year TLR-free survival (79.3%) and clinical patency (77.3%). 3) The incidence of complications after iliac artery EVT was 6.8% including major complications in 1.0% of cases, mainly driven by bleeding complications (e.g., access site bleeding and vascular rupture). The TASC D group showed a relatively higher incidence of complications than the other TASC lesion groups, but procedure-related and in-hospital death rates were not different between TASC groups. 4) TASC D, plain old balloon angioplasty, current smoker, previous bypass surgery, combined femoropopliteal or below the knee treatment, and complications were identified as independent risk factors for TLR.
In recent guidelines, EVT was considered standard therapy for patients with TASC A, B, and C iliac artery lesions.
2)7)9) Even for TASC D lesions, EVT is suggested as an alternative treatment option in experienced centers after consideration of patient age and comorbidities.
2)3)10) Surgical bypass is still considered the standard treatment for TASC D lesions due to the excellent long term patency rate of up to 80% over 10 years. However, surgery is known to carry higher complication and mortality rates than EVT.
9) In a meta-analysis comparing surgical bypass and EVT outcomes in more than 5,000 patients with TASC C and D lesions, the 5-year primary patency rates were 82.6% and 71.4% (p<0.001), respectively. Complications occurred in 18.0% and 13.4% (p<0.001), and the 30-day mortality rates were 2.6% and 0.7% (p<0.001) for surgery and EVT, respectively. Thus, surgical bypass offered superior long-term patency, whereas EVT was safer regarding complications and procedure-related mortality.
5) In the most recent EVT studies that reflect recent advances in intervention devices and skills, the success and mid-term patency rates did not differ between TASC A/B and C/D lesions, suggesting that current EVT may yield more positive outcomes than in the past.
11)12)
Although there are still limited long-term EVT data on TASC D lesions, the primary patency rate of TASC C and D lesions after EVT ranged from 60% to 86% at 5-year follow-up in meta-analysis.
13) Suzuki et al.
14) reported a comparable 5-year patency rate of 77.1% for TASC D lesions with a relatively lower procedural success rate (91.6%) and more procedure complications (11.1%) compared with other TASC lesions. In contrast, recent single-center results from Çakmak et al.
15) showed that the lower 5-year TLR-free rates for EVT procedures from 2015–2017 were 65% for TASC D. However, they assessed a smaller study population with approximately 100 patients per TASC lesion group, and self-expandable stents were used only in up to 50% of cases. In the present study, TASC D showed lower TLR-free survival and clinical patency rates compared with other TASC lesion types. Nevertheless, TASC D lesions showed excellent procedural success (95.7%) with a low major complication (1.6%) and in-hospital mortality rates (1.4%), and favorable 5-year TLR-free survival (79.3%), and clinical patency (77.3%). It is possible that TASC D patients with relatively low morbidities may have been considered for EVT and achieved favorable immediate and late outcomes. In addition, we can also speculate that larger vessel diameter, availability of bidirectional approach, and improved intervention skills and devices may contribute to high technical success rate even for complex iliac artery lesions. The higher patency rates after EVT in iliac lesions compared with femoropopliteal lesions may be explained by larger vessel diameter, shorter lesion length, and lesser influence from leg movement.
16) Thus, we believe that EVT may be considered as the alternative treatment option for TASC D lesions in selected patients, especially those at high surgical risk.
Recently, covered stents demonstrated favorable results in iliac artery EVT, but large-scale, long-term clinical outcome data are still lacking.
17) Due to the limited availability of covered stents in Korea, only 1.2% of cases in the present study were treated with covered stents, and all cases were used emergently in cases of vascular rupture.
Previous iliac EVT studies identified age <50 years, female sex, diabetes mellitus, hyperlipidemia, smoking history, TASC C/D lesions, EIA involvement, balloon angioplasty, and smaller stent diameter as risk factors for patency loss.
4)16)18)19) Similarly, we found that TASC D, balloon angioplasty and current smoker were important predictive factors for TLR rates in our long-term data. Additional factors associated with TLR were previous bypass surgery, combined femoropopliteal and below the knee treatment, and complications. As more difficult lesions are increasingly addressed with EVT, better treatment in femoropopliteal and below the knee artery lesions, and lower procedural complications may also help increase long-term patency rates after iliac EVT.
Our results should be considered in the context of some limitations. First, this was a retrospective study with the inherent limitations of this study nature. Second, median follow-up of study was 699 days (315.5–1,097.5) and there was relatively small portion of patients followed over 3 years. However, the standard errors for clinical events in the Kaplan-Meier analysis did not exceed 10% up to 5 years. Third, primary patency based on regular imaging data could not be obtained, so TLR was chosen as the primary endpoint and explains the more favorable clinical outcomes in our study. Fourth, differences in procedural skills and strategies between operators could not be considered because of the limited study population. The procedures were performed over 10 years, and there might have been numerous changes in procedures, instruments, and stent profiles. Fifth, there was no information on target lesion calcification severity. Heavily calcified lesions are often challenging for endovascular procedures and affect the treatment strategy including stent type. Sixth, subintimal or intraluminal passage of the wires was not confirmed by intravascular ultrasound during the procedure. Thus, we used the term “subintimal approach” instead of “subintimal angioplasty.” Seventh, we did not analyze the procedure images in an independent core lab and relied on the data entered by the investigators. Thus, detailed analysis of the factors regarding procedure failure or complications was limited.
In conclusion, iliac artery EVT achieved excellent technical success and 5-year TLR-free survival. TASC D showed a favorable albeit lower 5-year TLR-free survival compared with other TASC groups. EVT may be considered for TASC D lesions as the alternative treatment option in selected patients at high surgical risk.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download