DISCUSSION
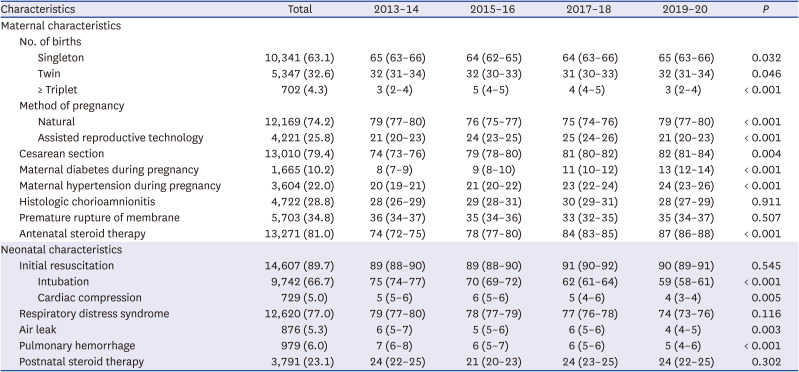
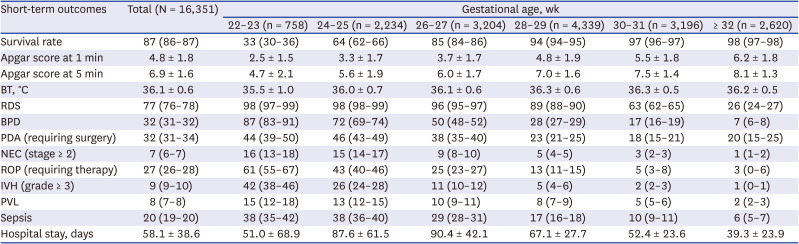
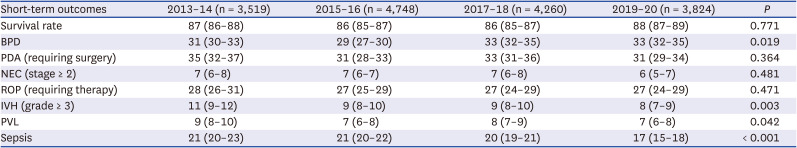
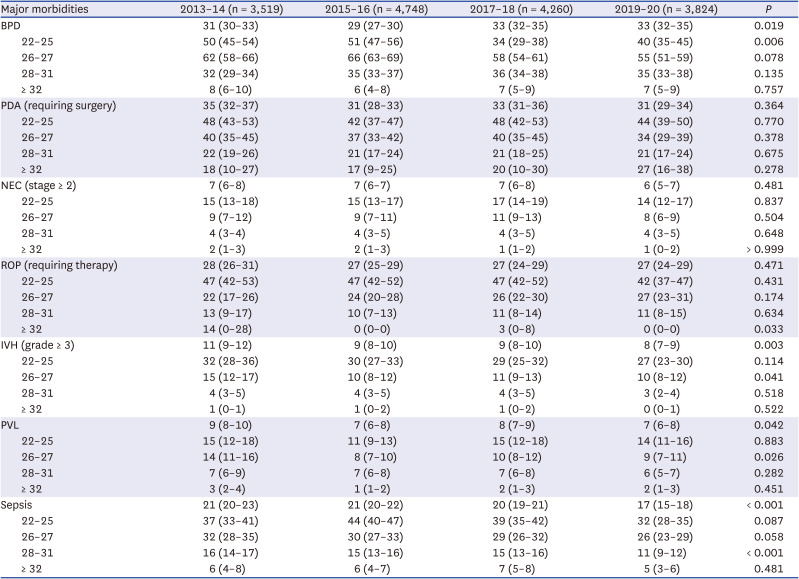
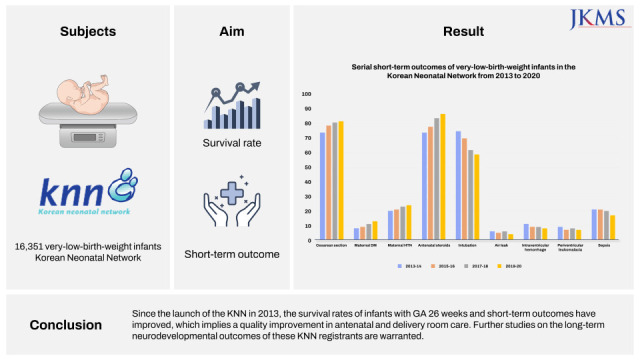
We believe that this study makes a significant contribution to the literature because, to the best of our knowledge, it is the first to evaluate the overall survival rate and major morbidities of VLBWIs in Korea born between 2013 and 2020 using a prospective nationwide large cohort registry. More mothers delivered by cesarean section, had diabetes or hypertension during their pregnancy, and received antenatal steroids when analyzed according to era. Fewer infants were intubated at birth and had air leaks when analyzed according to era. The overall survival rate of VLBWIs between 2013 and 2020 was 87% in the present study. The rates of RDS and BPD were 77% and 32%. The rates of ligation of PDA among infants with PDA, NEC (stage ≥ 2), ROP requiring therapy among infants with ROP, and IVH (grade ≥ 3) were 32%, 7%, 27%, and 9%, respectively.
A total of 79% of VLBWIs were born by cesarean section between 2013 and 2020, which increased from 74% in 2013–14 to 82% in 2019–20. Delivery by cesarean section was performed in 62%, 81%, and 78% of infants with a GA of < 24, 24–25, and 26–27 weeks, respectively, according to the data from the annual reports of the KNN. These rates were higher than those reported in the Australian and New Zealand Neonatal Network (ANZNN) report (44.8%, 56.4%, and 69.3% in infants with a GA of < 24, 24–25, and 26–27 weeks, respectively
21).
Exposure to antenatal steroids is associated with decreased mortality
22 and fewer morbidities
23 in preterm infants, especially in infants with a low GA.
24 A higher number of mothers of KNN registrants received antenatal steroids, which increased from 74% in 2013–14 to 87% in 2019–20. However, the rate of antenatal steroid therapy is still low compared with that in the Canadian Neonatal Network (CNN) or ANZNN reports. The rate of antenatal steroid administration was only 43% in infants with a GA of 22 weeks, and this increased to 79% and 83% in infants with a GA of 23 and 24 weeks, respectively, in the present study in 2020.
8 The rate of antenatal steroid administration was 87% in infants with a GA of 22–28 weeks and 92% in infants with a GA of 29–32 weeks in the present study in 2020. More than 90% of mothers of CNN registrants with a GA of < 33 weeks received antenatal steroids in 2020.
25 Only 4.5% and 5.8% of mothers of CNN registrants with a GA of 22–28 and 29–32 weeks, respectively, did not receive antenatal steroids in 2020. In addition, antenatal steroid therapy was performed in 92% of infants with a GA of < 32 weeks according to the ANZNN report,
21 a rate higher than that in the present study.
Apgar scores at 1 minute were 3, 3, and 4, which at 5 minutes were 5, 6, and 6 in the present study in infants with a GA of < 24, 24–25, and 26–27 weeks between 2013 and 2020, respectively. Apgar scores at 1 and 5 minutes according to the annual report of the KNN in 2020 were 3, 3, 4 and 5, 6, and 7 in infants with a GA of < 24, 24–25, and 26–27 weeks, values that were still lower than those reported in the ANZNN report (Apgar scores at 1 minute: 3, 5, and 5, Apgar scores at 5 minutes: 6, 7, and 8 in infants with a GA of < 24, 24–25, and 26–27 weeks, respectively
21).
Body temperature at admission was between 36.0°C and 36.3°C in infants with a GA of ≥ 24 weeks; however, it was 35.5°C in infants with a GA of < 24 weeks in the present study between 2013 and 2020. Body temperature at admission increased to 35.9°C and 36.1°C in infants with a GA of < 24 and 24–25 weeks according to the annual report of the KNN in 2020; however, this was lower than the values reported in the ANZNN report (between 36.3°C and 36.7°C
21).
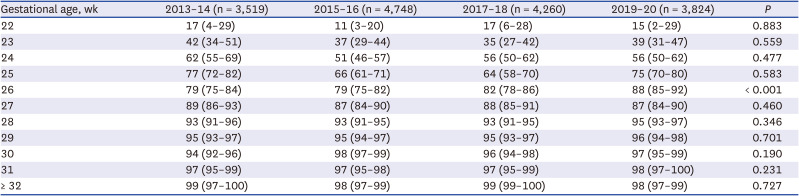
The survival rate of VLBWIs was 86% between 2013 and 2016 according to the study by Lee et al.,
6 which improved to 88% between 2019 and 2000 and finally to 89% in 2020 in the present study. The survival rates in 2020 in the present study were 29%, 44%, 60%, and 82% in infants with a GA of 22, 23, 24, and 25 weeks, respectively.
8 In the CNN report,
25 the survival rates in 2020 were 27%, 49%, 73%, and 85% in infants with a GA of 22, 23, 24, and 25 weeks, respectively. In the ANZNN report,
21 the survival rates in 2019 were 63%, 70%, and 83% in infants with a GA of < 24, 24, and 25 weeks. The survival rates of infants with a GA of 22–23 weeks in the present study are comparable to those in the CNN report, which were considerably lower than those reported in the ANZNN report. The survival rate of infants with a GA of 24 weeks was still lower than the values reported in the CNN and ANZNN reports (60% in the KNN, 73% in the CNN report, and 70% in the ANZNN report). The survival rate of infants with a GA of 25 weeks was comparable to those in the CNN and ANZNN reports (82% for the KNN, 85% for the CNN, and 83% for the ANZNN report). Finally, infants with a GA of 26 weeks in the present study in 2020 attained a survival rate of > 90%, which is comparable to the values reported in the CNN and ANZNN reports. Infants with a GA of 27 weeks within the CNN report and GA of 26 weeks within the ANZNN report attained survival rates of > 90%.
Although not statistically significant, the overall survival rate of preterm infants born in 2020 improved compared with that in the previous era. Furthermore, the survival of infants with a GA of 26 weeks markedly improved from 79% in 2013–14, 88% in 2019–20, and finally 91% in 2020. These findings should be highlighted. Improved survival in extremely preterm infants has been shown to be associated with improved survival without major morbidities in more mature preterm infants.
34 Therefore, we can expect improved intact survival without major morbidities in more mature preterm infants in the KNN in the near future.
BPD is one of the most serious complications of preterm infants, causing long-term adverse outcomes on respiratory, neurodevelopmental, and growth outcomes.
26 The rates of BPD in the present study in 2020 were 77%, 88%, and 69% in infants with a GA of < 24, 24, and 25 weeks, which is comparable to the values reported in the CNN and ANZNN reports (82%, 83%, 76% in the CNN report;
25 92%, 81%, 72% in the ANZNN report
21 in infants with a GA of < 24, 24, and 25 weeks, respectively). In particular, fewer infants with a GA of < 24 and 25 weeks had BPD than the CNN or ANZNN registrants. However, higher mortality rate among infants with smaller GA may be related to fewer rate of morbidities among survivors.
27 Further, KNN uses NICHD 2001 definition of BPD. This definition cannot diagnose preterm infants as having BPD who die of respiratory failure before 36 weeks’ postmenstrual age, the most severe form of BPD. The rate of BPD decreased to 59% and 45% in infants with a GA of 26 and 27 weeks, and this rate finally decreased to 40% in infants with a GA of 28 weeks in the annual report of the KNN in 2020. The rates of BPD in infants with a GA of 26, 27, and 28 weeks were 56%, 42%, and 37% according to the CNN report, and these were 60%, 54%, and 40% according to the ANZNN report. The incidence of BPD has not decreased or even increased despite remarkable advances in perinatal and neonatal care.
328 The improved survival of extremely preterm infants with a high risk of BPD is one of the reasons for this. In accordance with this trend, the incidence of BPD did not decrease in the present study (31% in 2013–14, 29% in 2015–16, and 33% both in 2017–18 and 2019–20).
Surgical interventions during NICU admission were associated with an increased risk of long-term neurodevelopmental impairment.
29 Ligation of the PDA is one of the most commonly performed operations in the NICU. Therefore, PDA ligation rate can be an important risk factor for long-term neurodevelopmental impairment in preterm infants, though there are still controversies whether surgical ligation or medical treatment is better for symptomatic PDA of preterm infants.
3031 Overall, 24%, 23%, and 6% of PDAs among all infants with a specific GA of < 25, 25–26, and 27–28 weeks were surgically ligated in the present study in 2020. The rate of PDA ligation was modified for comparison with those in other studies. In the original version of the annual report of the KNN, the rate of ligation of PDA was assessed among symptomatic PDA cases, not among all PDA cases or among all patients. A total 11.4%, 6.9%, and 2.7% of PDAs among total infants with a GA of < 25, 25–26, and 27–28 weeks were ligated according to the CNN report.
25 More infants among KNN registrants received PDA ligation than those among CNN registrants.
The rates of NEC (stage ≥ 2) were 19%, 11%, and 6% in infants with a GA of < 25, 25–26, and 27–28 weeks in the present study by the annual report of the KNN in 2020, which were higher than those in the CNN report (13%, 7%, and 3% in infants with a GA of < 25, 25–26, and 27–28 weeks, respectively
25). Furthermore, the rate of NEC (stage ≥ 2) in infants with a GA of < 28 weeks was 12% in the present study, which was also higher than that in the ANZNN report (7% in infants with a GA of < 28 weeks
21).
The rates of ROP requiring therapy were 21%, 23%, 24%, 23%, and 4% among all infants with a specific GA of < 24, 24, 25, 26, and 27–28 weeks, respectively, in the present study in 2020. This rate was modified for comparison with other studies. In the original version of the annual report of the KNN, the rate of ROP requiring therapy was assessed among infants with ROP, not among all infants with a specific GA. The rates of ROP (stage ≥ 3) were 48%, 35%, 21%, 14%, and 4% in all infants with a GA of < 24, 24, 25, 26, and 27–28 weeks, respectively, according to the ANZNN report.
21 In addition, the rates of severe ROP (stage ≥ 3 and/or requiring laser or intraocular injection) were 58%, 36%, 26%, 12%, and 5% in all infants with a GA of < 24, 24, 25, 26, and 27 weeks, respectively, according to the CNN report.
25
The rates of IVH (grade ≥ 3) and PVL decreased significantly according to era and advancing GA. This finding is encouraging because IVH and PVL are closely related to the long-term neurodevelopmental impairment of preterm infants and to cerebral palsy.
32 IVH (grade ≥ 3) occurred in 39%, 26%, 17%, 10%, and 8% of infants with a GA of < 24, 24, 25, 26, and 27 weeks, respectively in the annual report of the KNN in 2020. The rates of PVL were 13%, 13%, 11%, 9%, and 9% in infants with a GA of < 24, 24, 25, 26, and 27 weeks, respectively. Fewer instances of IVH (grade ≥ 3) occurred in infants with a GA of < 24, 24, 25, 26, and 27 weeks, with rates of 27%, 18%, 14%, 7%, and 3%, respectively according to the ANZNN report. In addition, the overall rate of PVL was 1–3% in infants with a GA of 25–31 weeks according to the ANZNN report.
21 IVH (grade ≥ 3) and/or PVL occurred in 30%, 26%, 17%, 10%, and 9% of infants with a GA of < 24, 24, 25, 26, and 27 weeks, respectively, according to the CNN report.
25
Sepsis is one of the major causes of mortality and morbidity in very-preterm infants.
33 The rate of sepsis has been decreased serially from 21% in 2013–14 to 17% in 2019–20, and finally to 16% in 2020, which represents improved neonatal care and infection control. Sepsis occurred in 31%, 28%, and 18% of infants with a GA of < 25, 25–26, and 27–28 weeks, respectively, in the present study in 2020. Sepsis was less prevalent in infants with a GA of < 25 weeks in the present study compared with that in the CNN report (31% in the present study vs. 39% in the CNN report
25). However, sepsis was more frequent in infants with a GA of ≥ 25 weeks than in the CNN report (28% and 18% in the present study vs. 22% and 10% among CNN infants with a GA of 25–26 and 27–28 weeks).
Increased Apgar score and body temperature at admission and decreased need for advanced resuscitation at birth, such as intubation and cardiac compression, imply improved quality in delivery room care. Furthermore, the increased rate of antenatal steroid therapy implies a quality improvement in antenatal care. Improved antenatal and delivery room care can result in decreased IVH (grade ≥ 3) and PVL, further improving long-term neurodevelopmental outcomes.
The present study has some limitations. First, as we used data from the annual report of the KNN based on the its pre-set registry data, we could not analyze all of the data in detail by GA or era. Further, in the annual report of the KNN, hospital stay was based on total registrants not survivors, therefore infants with higher morality such as 22–23 weeks presenting shorter hospital stay among survivors was inevitable. Second, in comparison with the CNN or ANZNN reports, methodological differences in statistics were inevitable. For example, the CNN and ANZNN reports assessed the incidence of ROP requiring therapy among the total number of infants with specific GAs, while this was assessed among infants with ROP by the KNN. Furthermore, the data collection methods differed among studies. Therefore, the disease categories and incidences were different. For ROP cases requiring therapy, cases of ROP (stage ≥ 3) were collected by the ANZNN, and severe ROP cases (stage ≥ 3 and/or requiring laser or intraocular injection) were collected by the CNN. Therefore, a direct comparison between international networks was impossible. The strength of this study is that it is the first to analyze the overall survival rates and major morbidities of VLBWIs in Korea born between 2013 and 2020 using a prospective nationwide large cohort registry. This study also analyzed trends in survival rates and major morbidities according to era and GA.
In conclusion, since the launch of the KNN in 2013, the survival rate of infants with GA 26 weeks has improved serially; these findings are encouraging. We have already found that improved survival was accompanied by improved intact survival without major morbidities in more mature preterm infants; therefore, we can expect improved survival without major morbidities in the near future. Furthermore, the incidence of IVH, PVL, and sepsis has decreased serially. The decreased incidence of IVH and PVL may be related to improved long-term neurodevelopmental outcomes. Further studies on the long-term neurodevelopmental outcomes of these KNN registrants are warranted. We can also expect decreased mortality and morbidities in very-preterm infants, along with decreased incidence of sepsis. Furthermore, the rates of intubation at birth, and air leaks decreased over time implying improved delivery room care. Further studies regarding the effect of the changes of maternal and neonatal basal characteristics according to the changes of perinatal care and NICU care to short-term outcomes of these infants are warranted. Also, further studies analyzing whether there are changes of long-term outcomes in accordance with the changes of short-term outcomes are needed.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download