1. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public: a systematic review and meta-analysis. Psychiatry Res. 2020; 291:113190. PMID:
32563745.
2. Prati G, Mancini AD. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol Med. 2021; 51(2):201–211. PMID:
33436130.

3. Breslau J, Roth EA, Baird MD, Carman KG, Collins RL. A longitudinal study of predictors of serious psychological distress during COVID-19 pandemic. Psychol Med. Forthcoming. 2021; DOI:
10.1017/S0033291721004293.

4. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. 2020; 383(6):510–512. PMID:
32283003.

7. Choi J, Park Y, Kim HE, Song J, Lee D, Lee E, et al. Daily life changes and life satisfaction among Korean school-aged children in the COVID-19 pandemic. Int J Environ Res Public Health. 2021; 18(6):3324. PMID:
33807042.

8. Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, Simoes-E-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct. 2020; 51:101845. PMID:
32929399.

9. Schmidt SC, Anedda B, Burchartz A, Eichsteller A, Kolb S, Nigg C, et al. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Sci Rep. 2020; 10(1):21780. PMID:
33311526.

10. Montag C, Elhai JD. Discussing digital technology overuse in children and adolescents during the COVID-19 pandemic and beyond: on the importance of considering affective neuroscience theory. Addict Behav Rep. 2020; 12:100313. PMID:
33364321.

11. Masonbrink AR, Hurley E. Advocating for children during the COVID-19 school closures. Pediatrics. 2020; 146(3):e20201440. PMID:
32554517.

12. Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020; 221:264–266.e1. PMID:
32248989.

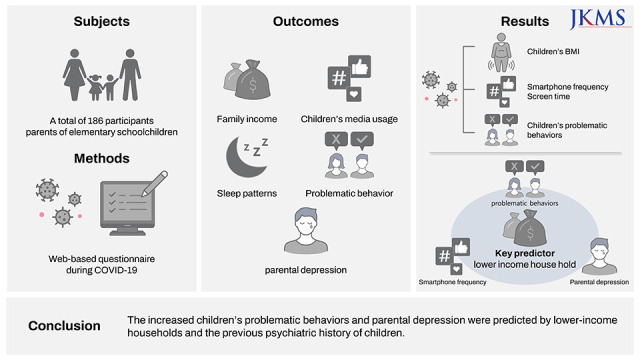
13. Kim SJ, Lee S, Han H, Jung J, Yang SJ, Shin Y. Parental mental health and children’s behaviors and media usage during COVID-19-related school closures. J Korean Med Sci. 2021; 36(25):e184. PMID:
34184439.

14. Ramiz L, Contrand B, Rojas Castro MY, Dupuy M, Lu L, Sztal-Kutas C, et al. A longitudinal study of mental health before and during COVID-19 lockdown in the French population. Global Health. 2021; 17(1):29. PMID:
33752717.

15. Poulain T, Meigen C, Sobek C, Ober P, Igel U, Körner A, et al. Loss of childcare and classroom teaching during the Covid-19-related lockdown in spring 2020: a longitudinal study on consequences on leisure behavior and schoolwork at home. PLoS One. 2021; 16(3):e0247949. PMID:
33651851.

16. Kwong AS, Pearson RM, Adams MJ, Northstone K, Tilling K, Smith D, et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br J Psychiatry. 2021; 218(6):334–343. PMID:
33228822.

17. Okely AD, Kariippanon KE, Guan H, Taylor EK, Suesse T, Cross PL, et al. Global effect of COVID-19 pandemic on physical activity, sedentary behaviour and sleep among 3- to 5-year-old children: a longitudinal study of 14 countries. BMC Public Health. 2021; 21(1):940. PMID:
34001086.

18. Daly M, Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J Psychiatr Res. 2021; 136:603–609. PMID:
33138985.

19. Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020; 7(6):547–560. PMID:
32304649.

20. Wade M, Prime H, Browne DT. Why we need longitudinal mental health research with children and youth during (and after) the COVID-19 pandemic. Psychiatry Res. 2020; 290:113143. PMID:
32502829.

21. Daly M, Sutin AR, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med. Forthcoming. 2020; DOI:
10.1017/S0033291720004432.

22. Meda N, Slongo I. Caution when linking COVID-19 to mental health consequences. Brain Behav Immun. 2020; 87:152. PMID:
32387514.

23. Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020; 7(10):883–892. PMID:
32707037.

24. Pierce M, McManus S, Jessop C, John A, Hotopf M, Ford T, et al. Says who? The significance of sampling in mental health surveys during COVID-19. Lancet Psychiatry. 2020; 7(7):567–568. PMID:
32502467.

25. Lee S, Kim S, Suh S, Han H, Jung J, Yang S, et al. Relationship between screen time among children and lower economic status during elementary school closures due to the coronavirus disease 2019 pandemic. BMC Public Health. 2022; 22(1):160. PMID:
35073908.

26. Craig BM, Brown DS, Reeve BB. Valuation of child behavioral problems from the perspective of US adults. Med Decis Making. 2016; 36(2):199–209. PMID:
26209476.

27. Zill JL. Marital disruption, parent-child relationships, and behavior problems in children. J Marriage Fam. 1986; 48(2):295–307.

28. Achenbach TM, Edelbrock CS. Behavioral problems and competencies reported by parents of normal and disturbed children aged four through sixteen. Monogr Soc Res Child Dev. 1981; 46(1):1–82.

29. Sultana S, Rahman MM, Sigel B, Hashizume M. Associations of lifestyle risk factors with overweight or obesity among adolescents: a multicountry analysis. Am J Clin Nutr. 2021; 113(3):742–750. PMID:
33381796.

30. Franckle R, Adler R, Davison K. Accelerated weight gain among children during summer versus school year and related racial/ethnic disparities: a systematic review. Prev Chronic Dis. 2014; 11:E101. PMID:
24921899.

31. Kang HM, Jeong DC, Suh BK, Ahn MB. The impact of the coronavirus disease-2019 pandemic on childhood obesity and vitamin D status. J Korean Med Sci. 2021; 36(3):e21. PMID:
33463095.

32. Limone P, Toto GA. Psychological and emotional effects of digital technology on children in COVID-19 pandemic. Brain Sci. 2021; 11(9):1126. PMID:
34573148.

33. Lee DY, Roh HW, Kim SJ, Park EJ, Yoo H, Suh S, et al. Trends in digital media use in Korean preschool children. J Korean Med Sci. 2019; 34(41):e263. PMID:
31650718.

34. Choi Y, Lee DY, Lee S, Park EJ, Yoo HJ, Shin Y. Association between screen overuse and behavioral and emotional problems in elementary school children. Soa Chongsonyon Chongsin Uihak. 2021; 32(4):154–160. PMID:
34671188.

35. Lee J, Lim H, Allen J, Choi G, Jung J. Smartphone addiction and depression among low-income boys since COVID-19: the moderating effect of being an only child. Healthcare (Basel). 2021; 9(10):1350. PMID:
34683030.

36. Chen W, Adler JL. Assessment of screen exposure in young children, 1997 to 2014. JAMA Pediatr. 2019; 173(4):391–393. PMID:
30776061.

37. Chen CYC, Byrne E, Vélez T. Impact of the 2020 pandemic of COVID-19 on families with school-aged children in the United States: roles of income level and race. J Fam Issues. 2021; 43(3):719–740.

38. Diaz A, Baweja R, Bonatakis JK, Baweja R. Global health disparities in vulnerable populations of psychiatric patients during the COVID-19 pandemic. World J Psychiatry. 2021; 11(4):94–108. PMID:
33889535.

39. McGuine TA, Biese KM, Petrovska L, Hetzel SJ, Reardon C, Kliethermes S, et al. Mental health, physical activity, and quality of life of US adolescent athletes during COVID-19-related school closures and sport cancellations: a study of 13\xe2\x80\x8a000 athletes. J Athl Train. 2021; 56(1):11–19. PMID:
33290516.

40. Newlove-Delgado T, McManus S, Sadler K, Thandi S, Vizard T, Cartwright C, et al. Child mental health in England before and during the COVID-19 lockdown. Lancet Psychiatry. 2021; 8(5):353–354. PMID:
33444548.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download