This article has been
cited by other articles in ScienceCentral.
ABSTRACT
A 16-year-old patient with pectus excavatum visited our hospital because of palpitation. He underwent first Nuss operations at the age of 3. When he was 13 years old, the slow-fast type atrioventricular nodal reentrant tachycardia was documented during electrophysiology study. However, the catheter ablation was not conducted because of recurrent atrial fibrillation during procedure. At that time, second Nuss operation was performed due to progressive chest wall deformity. And then, atrioventricular nodal reentrant tachycardia was successfully treated by radiofrequency catheter ablation at the higher position than usual slow pathway zone under the modified fluoroscopic view with the cranial angle although distorted right atrial geometry and radiographic obstacle of Nuss operation bar. The concern about abnormal cardiac and electrical anatomy, and the accurate and modified procedure technique are essential in patients with pectus excavatum. (Ewha Med J 2022;45(3):e6)
Keywords: Tachycardia, Atrioventricular nodal reentry, Catheter ablation, Pectus excavatum, Nuss operation
Introduction
Chest wall deformity such as pectus excavatum is associated with different types of cardiac arrhythmias. Supraventricular and ventricular arrhythmia often occur regardless of chest repair operation (Nuss operation), which is caused by compression of the anterior sternal wall [
1–
4]. In addition, repair operation of pectus excavatum can change thoracic cavity dimension and geometry [
5]. It might cause several challenges of catheter ablation for supraventricular tachyarrhythmias. Here, we report atrioventricular nodal reentrant tachycardia (AVNRT) with successful catheter ablation, in spite of distorted cardiac geometry and radiographic obstacle of Nuss operation bar.
Case Report
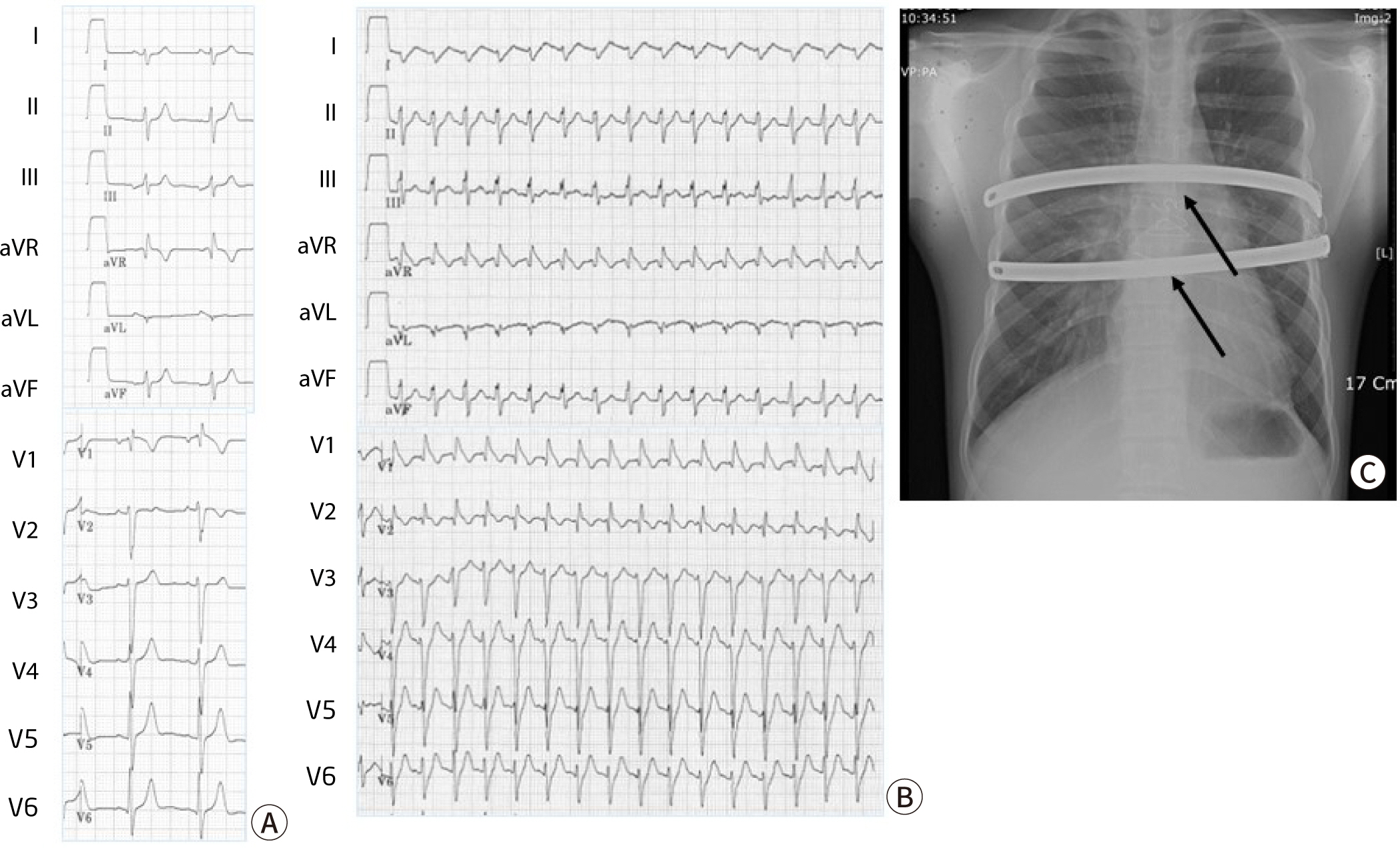
A 16-year-old patient with pectus excavatum visited our hospital because of palpitation. He had history of Nuss operations at the age of 3. With progressively worsening chest wall deformity for several years after Nuss operation, he felt frequent palpitation. The 12-leads surface ECG revealed wide QRS tachycardia with heart rate of 180 bpm, that is supraventricular tachycardia with incomplete right bundle branch block pattern (
Fig. 1A, 1B). He had taken propranolol and flecainide. When he was 13 years old, electrophysiology study was performed at other hospital. The slow-fast type AVNRT was documented during electrophysiology study. However, the catheter ablation was not conducted because atrial fibrillation (AF) was frequently induced by programmed electrical stimulation during procedure. At that time, combined severe chest wall deformity was corrected by the second Nuss operation at other hospital. In spite of antiarrhythmic medications, palpitation was not controlled well. He was referred to our hospital for radiofrequency catheter ablation.
Fig. 1.
12-lead surface electrocardiogram and Chest X-ray. (A) The baseline surface electrocardiogram showing incomplete right bundle branch block. (B) A wide QRS tachycardia with heart rate of 180 bpm suggesting supraventricular tachycardia with incomplete right bundle branch block pattern. (C) Chest X-ray showing Nuss operation bar (arrows).
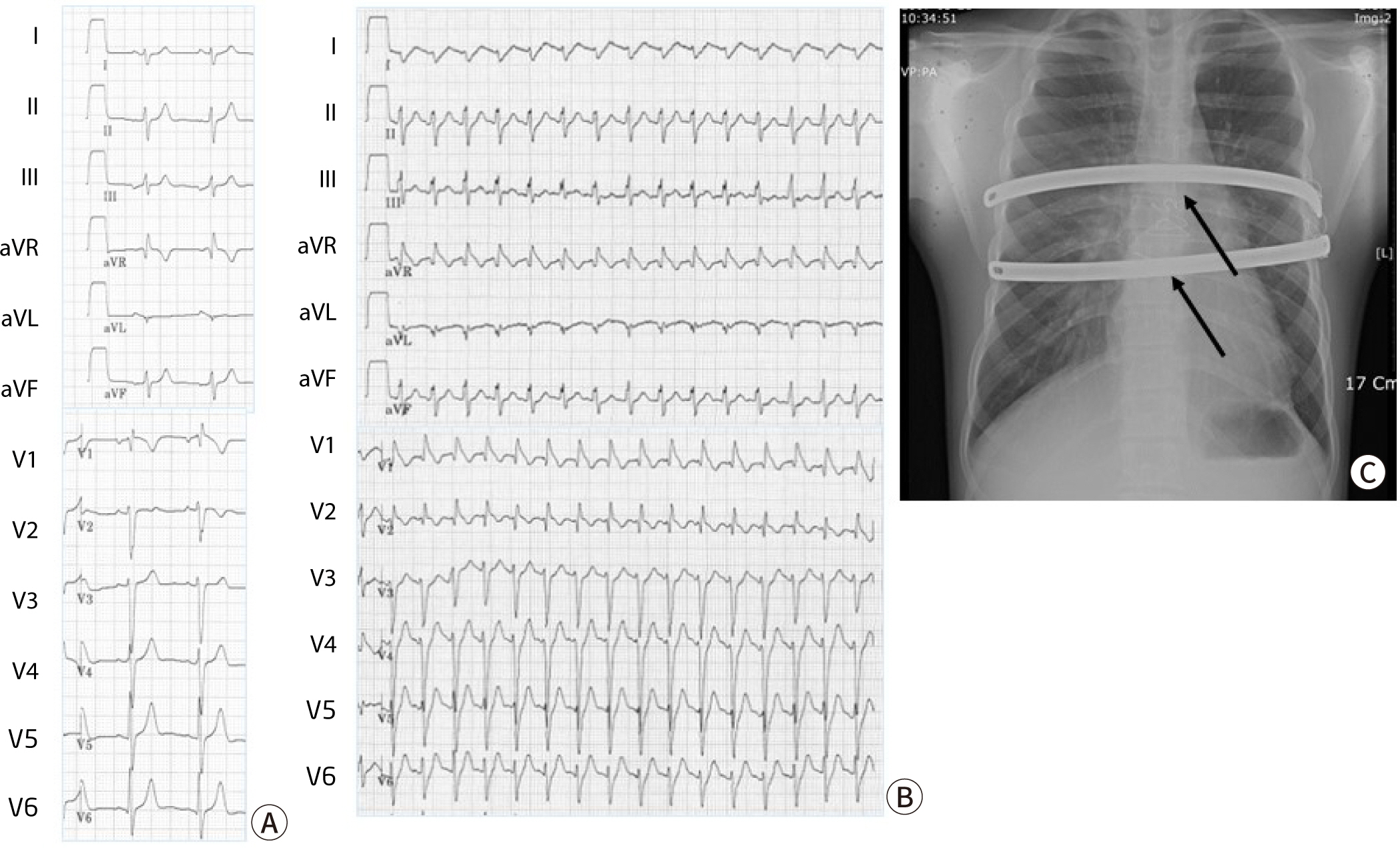
Chest X-rays revealed an enlarged cardio-thoracic ratio with two radiopaque Nuss bar (
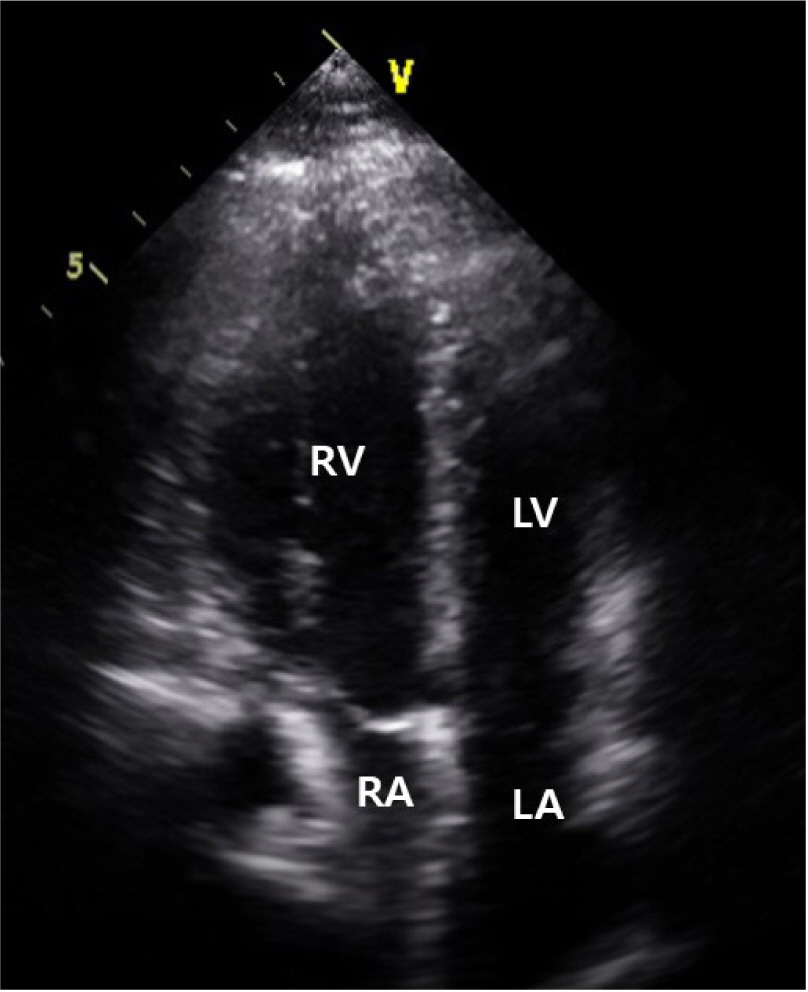
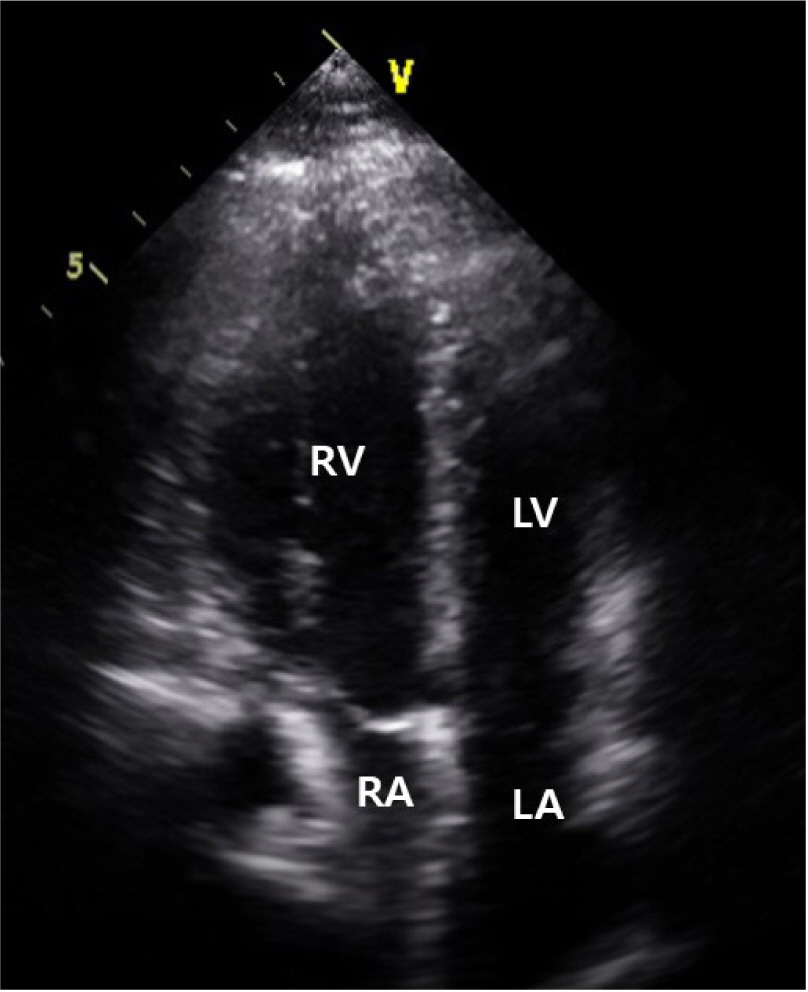
Fig. 1C), and transthoracic echocardiography revealed severely right atrial compression against the sternum (
Fig. 2).
Fig. 2.
Transthoracic echocardiography showing the compression of right atrium on apical four chamber view. RV, right ventricle; LV, left ventricle; RA, right atrium; LA, left atrium.
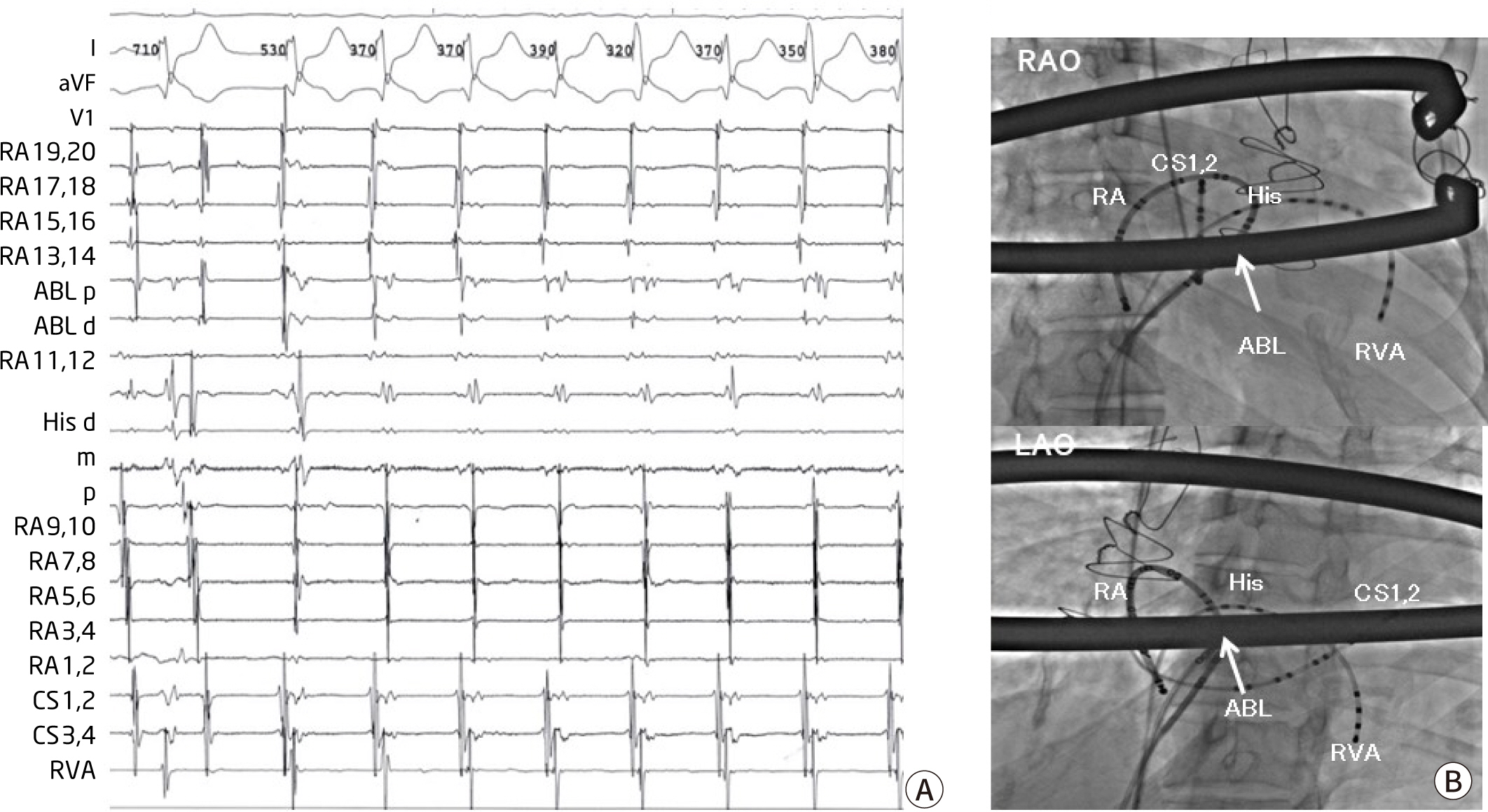
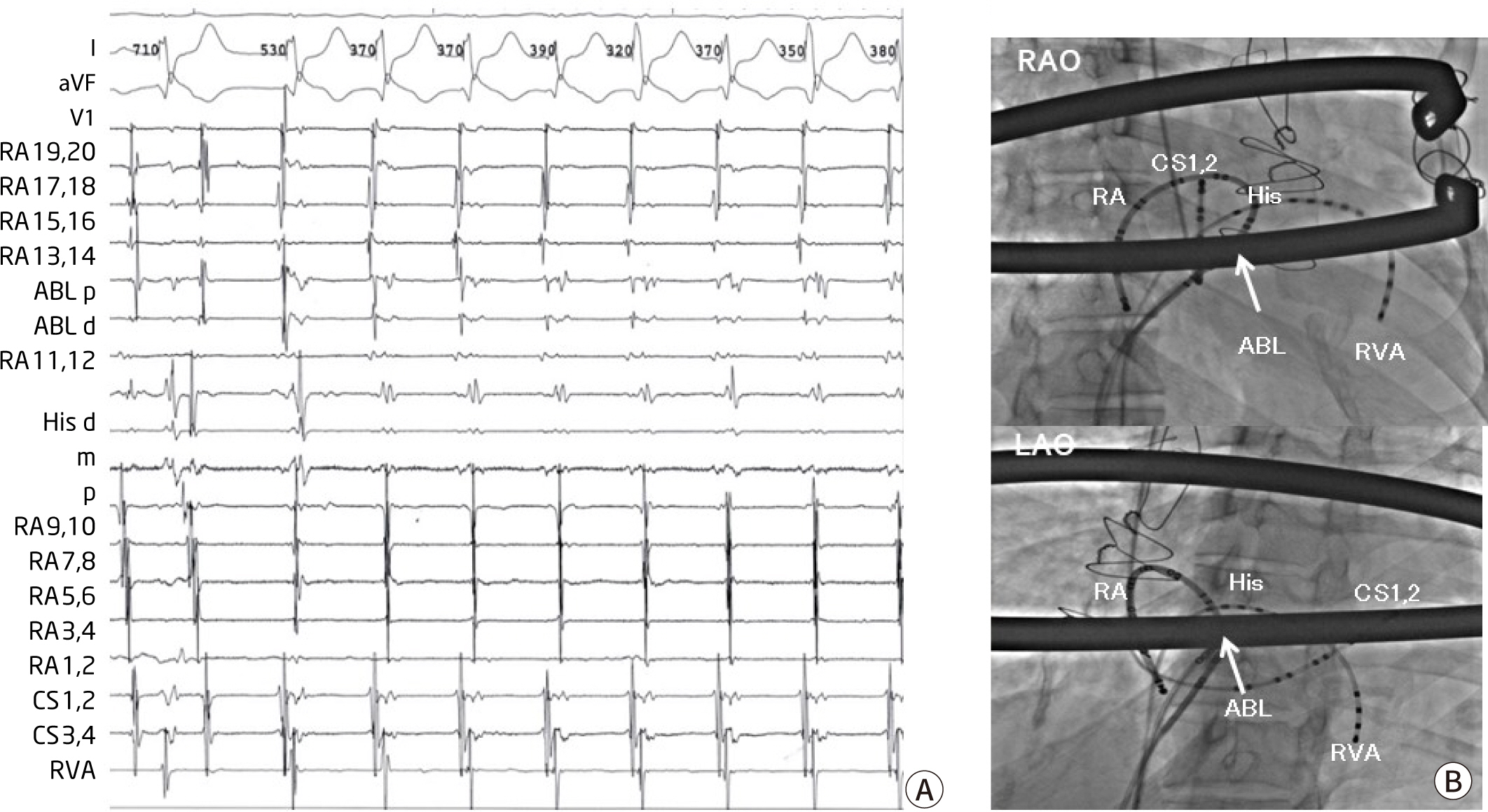
After obtaining written informed consent, the electrophysiology study was performed under local anesthesia. Multielectrode duodecapolar, decapolar and quadripolar catheters were placed in the right atrium (RA), right ventricular (RV) apex, His bundle region and coronary sinus (CS) via the right or left femoral vein and right internal jugular vein, respectively. During catheter manipulation, sustained AF was induced. Then, we terminated AF by internal cardioversion of 10 joule. Nonsustained AF was frequently induced during procedure. However, most of AF occurrence was spontaneously terminated. After confirming slow-fast type AVNRT which was reproducibly induced during electrophysiology study (
Fig. 3A), we first targeted the slow pathway zone between CS ostium and tricuspid annulus at the level of CS ostial roof. However, slow pathway was not ablated adequately because of distorted RA geometry and radiographic obstacle of Nuss operation bar. So, we repositioned the His catheter to find the location where the His signal was greatest and set the fluoroscopic view as the cranial angle to accurately see the movement of the ablation catheter. We finally gave radiofrequency energy at the higher position than usual slow pathway zone (
Fig. 3B), producing junctional rhythm with 1:1 retrograde conduction during radiofrequency delivery. After ablation, the patient remained free from the tachycardia during 3 year of follow-up.
Fig. 3.
Successful ablation site of atrioventricular nodal reentrant tachycardia. (A) Intra-cardiac electrogram showing the atrioventricular nodal reentrant tachycardia with earliest atral activation site of His area at a cycle length of 380 ms. (B) Fluoroscopic images in the left anterior oblique (LAO) and right anterior oblique (RAO) projection showing the masablation catheter positioned at the higher site than usual slow pathway zone. RA, right atrium; CS, coronary sinus; ABL, ablation catheter; RV, right ventricular catheter; His, His potential.
Discussion
Pectus excavatum is the most common congenital chest wall deformity. It causes cardiac compression and distorsion, resulting in cardiac dysfunction and arrhythmias. In patients with pectus excavatum, chest wall compression-induced arrhythmias often occur regardless of chest repair operation. Cardiac arrhythmias are caused by compression of RA and RV against the sternum, left atrium (LA) compression against the spinal column, and lateral displacement of the heart to the left. The observed arrhythmias are supraventricular tachycardia, AF, premature ventricular complex, and VT [
1–
4]. AF was documented in two thirds of the patients with mild form pectus excavatum. The possible explanation of the development of AF in pectus excavatum is that direct RA compression and LA mechanical compression could trigger the development of AF in a mechanism similar to that proposed for swallowing AF, which is thought to potentially result from the mechanical stimulation of the LA and/or the activation of vagal reflexes during swallowing [
1]. Monomorphic or polymorphic VT were caused by mechanical compression and abnormal rotation of the RV [
2,
6]. Previous studies demonstrated preoperative arrhythmia showed marked improvement after surgical repair of pectus excavatum [
6,
7]. In addition, difficult surgical and catheter ablation were demonstrated in several reports [
8,
9].
The Nuss procedure has been used as a minimally invasive repair for pectus excavatum. A convex steel bar is usually inserted under the sternum through bilateral thoracic incisions. When the steel bar is in position, the bar is turned over to the anterior chest, thereby correcting the chest wall deformity [
10]. After correction of anterior depression of the sternum, compensatory narrowing of chest width was observed. Changes in thoracic dimensions following the Nuss procedure were distinct in patients aged above 13 years [
5]. In the present case, the patient underwent Nuss operation at the age of 3. The surgery performed at that time may not have been sufficiently corrected. Furthermore, as the chest wall gradually deformed, the tachyarrhythmia seemed to be getting worse. Initially catheter ablation for AVNRT was failed because repetitive occurrence of AF during procedure. After second Nuss operation of severe chest wall deformity, nonsustained AF was frequently induced during catheter ablation. However, most of AF was spontaneously terminated. Internal cardioversion was performed only once because of sustained AF. Regarding the mechanism of AF in pectus excavatum, decreased mechanical stimulation may reduce the sustained AF after operation for pectus deformity.
In the previous report, symptomatic pediatric patients much improved 2 years postoperatively, while the bar was in place [
11]. In case of sustained tachycardia, the ablation procedure can be considered at least 2 years after surgery.
The slow pathway was unusually located owing to cardiac distorsion. So, we repositioned the His catheter to find the location where the His signal was greatest. And the location of ablation catheter was not clear due to Nuss operation bar on the fluoroscopic views. Therefore, we set the fluoroscopic views to the cranial angle of the right and left anterior oblique view to accurately confirm the movement of the ablation catheter. The 3-dimensional electroanatomic mapping system may help locate catheter position in this condition.
The cardiac and electrical geometry is influenced not only by the chest wall deformity itself but also Nuss operation. Therefore, the concern about distorted cardiac and electrical anatomy, and the accurate and modified procedure technique are essential in patients with pectus excavatum.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download