1. Dahou A, Levin D, Reisman M, Hahn RT. Anatomy and physiology of the tricuspid valve. JACC Cardiovasc Imaging. 2019; 12:458–468. PMID:
30846121.
2. Rogers JH, Bolling SF. The tricuspid valve: current perspective and evolving management of tricuspid regurgitation. Circulation. 2009; 119:2718–2725. PMID:
19470900.
3. Muraru D, Surkova E, Badano LP. Revisit of functional tricuspid regurgitation; current trends in the diagnosis and management. Korean Circ J. 2016; 46:443–455. PMID:
27482252.

4. McCartney SL, Taylor BS, Nicoara A. Functional tricuspid regurgitation in mitral valve disease. Semin Cardiothorac Vasc Anesth. 2019; 23:108–122. PMID:
30382771.

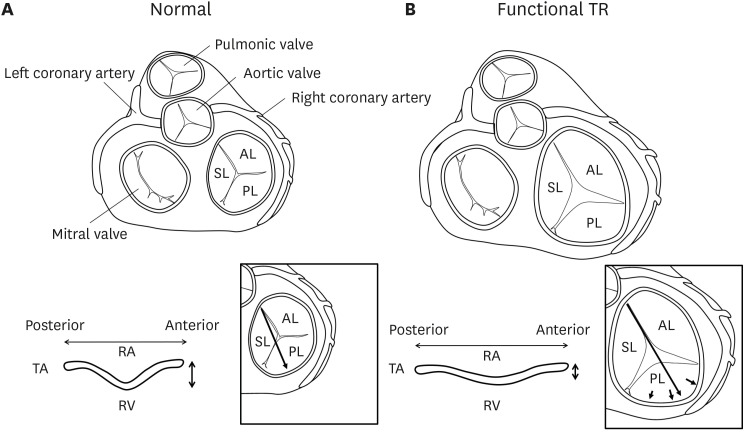
5. Fukuda S, Saracino G, Matsumura Y, et al. Three-dimensional geometry of the tricuspid annulus in healthy subjects and in patients with functional tricuspid regurgitation: a real-time, 3-dimensional echocardiographic study. Circulation. 2006; 114:I492–I498. PMID:
16820625.
6. Badano LP, Agricola E, Perez de Isla L, Gianfagna P, Zamorano JL. Evaluation of the tricuspid valve morphology and function by transthoracic real-time three-dimensional echocardiography. Eur J Echocardiogr. 2009; 10:477–484. PMID:
19482963.

7. Fender EA, Zack CJ, Nishimura RA. Isolated tricuspid regurgitation: outcomes and therapeutic interventions. Heart. 2018; 104:798–806. PMID:
29229649.

8. Topilsky Y, Maltais S, Medina Inojosa J, et al. Burden of tricuspid regurgitation in patients diagnosed in the community setting. JACC Cardiovasc Imaging. 2019; 12:433–442. PMID:
30121261.

9. Sagie A, Freitas N, Chen MH, Marshall JE, Weyman AE, Levine RA. Echocardiographic assessment of mitral stenosis and its associated valvular lesions in 205 patients and lack of association with mitral valve prolapse. J Am Soc Echocardiogr. 1997; 10:141–148. PMID:
9083969.

10. Prihadi EA, Delgado V, Leon MB, Enriquez-Sarano M, Topilsky Y, Bax JJ. Morphologic types of tricuspid regurgitation: characteristics and prognostic implications. JACC Cardiovasc Imaging. 2019; 12:491–499. PMID:
30846123.
11. Topilsky Y, Khanna A, Le Tourneau T, et al. Clinical context and mechanism of functional tricuspid regurgitation in patients with and without pulmonary hypertension. Circ Cardiovasc Imaging. 2012; 5:314–323. PMID:
22447806.

12. Park JH, Shin SH, Lee MJ, et al. Clinical and echocardiographic factors affecting tricuspid regurgitation severity in the patients with lone atrial fibrillation. J Cardiovasc Ultrasound. 2015; 23:136–142. PMID:
26446397.

13. Utsunomiya H, Itabashi Y, Mihara H, et al. Functional tricuspid regurgitation caused by chronic atrial fibrillation: a real-time 3-dimensional transesophageal echocardiography study. Circ Cardiovasc Imaging. 2017; 10:e004897. PMID:
28073806.

14. Enriquez-Sarano M, Messika-Zeitoun D, Topilsky Y, Tribouilloy C, Benfari G, Michelena H. Tricuspid regurgitation is a public health crisis. Prog Cardiovasc Dis. 2019; 62:447–451. PMID:
31707061.

15. Baek J, Lee H, Lee HH, Heo JE, Cho SM, Kim HC. Thirty-six year trends in mortality from diseases of circulatory system in Korea. Korean Circ J. 2021; 51:320–332. PMID:
33821581.

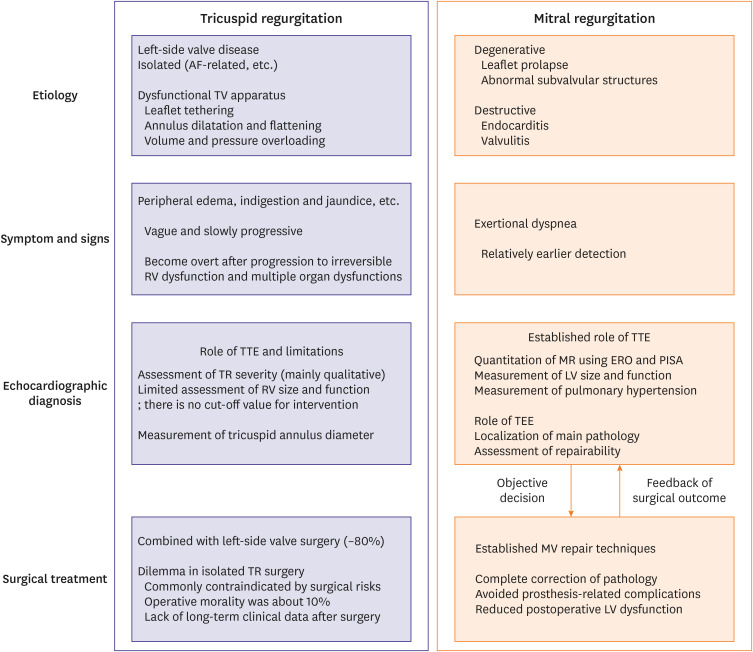
16. Arsalan M, Walther T, Smith RL 2nd, Grayburn PA. Tricuspid regurgitation diagnosis and treatment. Eur Heart J. 2017; 38:634–638. PMID:
26358570.

17. Asmarats L, Taramasso M, Rodés-Cabau J. Tricuspid valve disease: diagnosis, prognosis and management of a rapidly evolving field. Nat Rev Cardiol. 2019; 16:538–554. PMID:
30988448.

18. Taramasso M, Gavazzoni M, Pozzoli A, et al. Tricuspid regurgitation: predicting the need for intervention, procedural success, and recurrence of disease. JACC Cardiovasc Imaging. 2019; 12:605–621. PMID:
30947904.
19. Fender EA, Petrescu I, Ionescu F, et al. Prognostic importance and predictors of survival in isolated tricuspid regurgitation: a growing problem. Mayo Clin Proc. 2019; 94:2032–2039. PMID:
31279540.

20. Oh JK, Yoon YH, Roh JH, et al. Prognostic impact of left atrial strain after mitral valve repair surgery in patients with severe mitral regurgitation. Korean Circ J. 2022; 52:205–217. PMID:
35129314.

21. Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol. 2004; 43:405–409. PMID:
15013122.

22. Sadeghi HM, Kimura BJ, Raisinghani A, et al. Does lowering pulmonary arterial pressure eliminate severe functional tricuspid regurgitation? Insights from pulmonary thromboendarterectomy. J Am Coll Cardiol. 2004; 44:126–132. PMID:
15234420.

23. Benedetto U, Melina G, Angeloni E, et al. Prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing mitral valve surgery. J Thorac Cardiovasc Surg. 2012; 143:632–638. PMID:
22244561.

24. Dreyfus GD, Martin RP, Chan KM, Dulguerov F, Alexandrescu C. Functional tricuspid regurgitation: a need to revise our understanding. J Am Coll Cardiol. 2015; 65:2331–2336. PMID:
26022823.
25. Topilsky Y, Nkomo VT, Vatury O, et al. Clinical outcome of isolated tricuspid regurgitation. JACC Cardiovasc Imaging. 2014; 7:1185–1194. PMID:
25440592.
26. McCarthy FH, Vemulapalli S, Li Z, et al. Association of tricuspid regurgitation with transcatheter aortic valve replacement outcomes: a report from The Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. Ann Thorac Surg. 2018; 105:1121–1128. PMID:
29502934.

27. Pagnesi M, Montalto C, Mangieri A, et al. Tricuspid annuloplasty versus a conservative approach in patients with functional tricuspid regurgitation undergoing left-sided heart valve surgery: a study-level meta-analysis. Int J Cardiol. 2017; 240:138–144. PMID:
28499671.

28. Chikwe J, Itagaki S, Anyanwu A, Adams DH. Impact of concomitant tricuspid annuloplasty on tricuspid regurgitation, right ventricular function, and pulmonary artery hypertension after repair of mitral valve prolapse. J Am Coll Cardiol. 2015; 65:1931–1938. PMID:
25936265.

29. Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017; 30:303–371. PMID:
28314623.

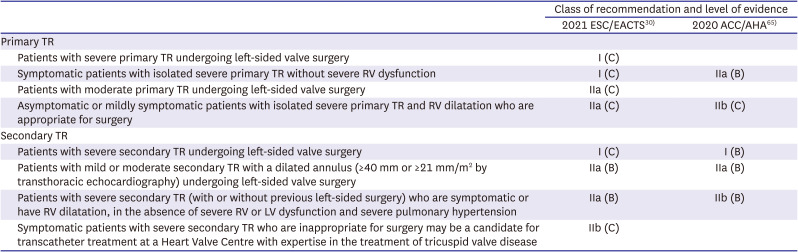
30. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022; 43:561–632. PMID:
34453165.
31. Dreyfus J, Durand-Viel G, Raffoul R, et al. Comparison of 2-dimensional, 3-dimensional, and surgical measurements of the tricuspid annulus size: clinical implications. Circ Cardiovasc Imaging. 2015; 8:e003241. PMID:
26156015.

32. Park YH, Song JM, Lee EY, Kim YJ, Kang DH, Song JK. Geometric and hemodynamic determinants of functional tricuspid regurgitation: a real-time three-dimensional echocardiography study. Int J Cardiol. 2008; 124:160–165. PMID:
17383758.

33. Fukuda S, Song JM, Gillinov AM, et al. Tricuspid valve tethering predicts residual tricuspid regurgitation after tricuspid annuloplasty. Circulation. 2005; 111:975–979. PMID:
15710756.

34. Min SY, Song JM, Kim JH, et al. Geometric changes after tricuspid annuloplasty and predictors of residual tricuspid regurgitation: a real-time three-dimensional echocardiography study. Eur Heart J. 2010; 31:2871–2880. PMID:
20601392.

35. Hahn RT, Zamorano JL. The need for a new tricuspid regurgitation grading scheme. Eur Heart J Cardiovasc Imaging. 2017; 18:1342–1343. PMID:
28977455.

36. Hahn RT, Thomas JD, Khalique OK, Cavalcante JL, Praz F, Zoghbi WA. Imaging assessment of tricuspid regurgitation severity. JACC Cardiovasc Imaging. 2019; 12:469–490. PMID:
30846122.
37. Hahn RT, Meduri CU, Davidson CJ, et al. Early feasibility study of a transcatheter tricuspid valve annuloplasty: SCOUT trial 30-day results. J Am Coll Cardiol. 2017; 69:1795–1806. PMID:
28385308.
38. Kim YJ, Kwon DA, Kim HK, et al. Determinants of surgical outcome in patients with isolated tricuspid regurgitation. Circulation. 2009; 120:1672–1678. PMID:
19822809.

39. Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713. PMID:
20620859.

40. Khalique OK, Cavalcante JL, Shah D, et al. Multimodality imaging of the tricuspid valve and right heart anatomy. JACC Cardiovasc Imaging. 2019; 12:516–531. PMID:
30846125.

41. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14. PMID:
25559473.

42. Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson. 2020; 22:17. PMID:
32089132.

43. Zhan Y, Senapati A, Vejpongsa P, Xu J, Shah DJ, Nagueh SF. Comparison of echocardiographic assessment of tricuspid regurgitation against cardiovascular magnetic resonance. JACC Cardiovasc Imaging. 2020; 13:1461–1471. PMID:
32199838.

44. Everett RJ, Treibel TA, Fukui M, et al. Extracellular myocardial volume in patients with aortic stenosis. J Am Coll Cardiol. 2020; 75:304–316. PMID:
31976869.

45. Kwak S, Everett RJ, Treibel TA, et al. Markers of myocardial damage predict mortality in patients with aortic stenosis. J Am Coll Cardiol. 2021; 78:545–558. PMID:
34353531.

46. Constant Dit Beaufils AL, Huttin O, Jobbe-Duval A, et al. Replacement myocardial fibrosis in patients with mitral valve prolapse: relation to mitral regurgitation, ventricular remodeling, and arrhythmia. Circulation. 2021; 143:1763–1774. PMID:
33706538.
47. Grosse-Wortmann L, Macgowan CK, Vidarsson L, Yoo SJ. Late gadolinium enhancement of the right ventricular myocardium: Is it really different from the left? J Cardiovasc Magn Reson. 2008; 10:20. PMID:
18466606.
48. Wang TK, Akyuz K, Reyaldeen R, et al. Prognostic value of complementary echocardiography and magnetic resonance imaging quantitative evaluation for isolated tricuspid regurgitation. Circ Cardiovasc Imaging. 2021; 14:e012211. PMID:
34521215.

49. Asmarats L, Puri R, Latib A, Navia JL, Rodés-Cabau J. Transcatheter tricuspid valve interventions: landscape, challenges, and future directions. J Am Coll Cardiol. 2018; 71:2935–2956. PMID:
29929618.
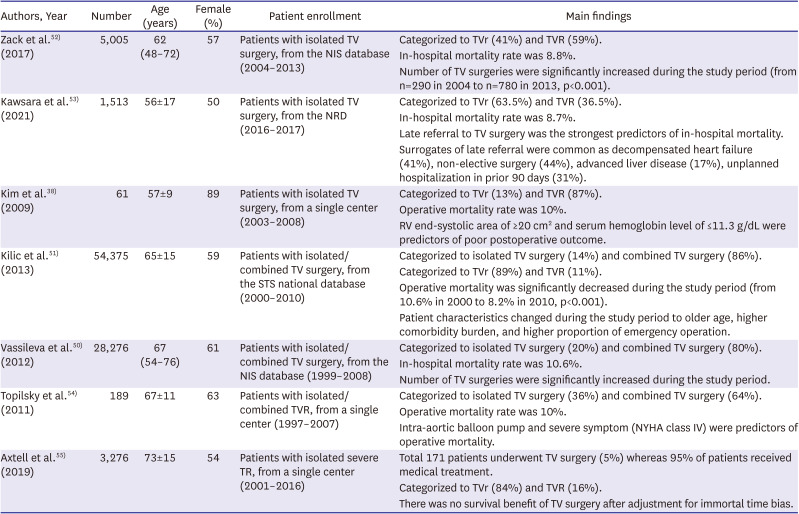
50. Vassileva CM, Shabosky J, Boley T, Markwell S, Hazelrigg S. Tricuspid valve surgery: the past 10 years from the Nationwide Inpatient Sample (NIS) database. J Thorac Cardiovasc Surg. 2012; 143:1043–1049. PMID:
21872283.

51. Kilic A, Saha-Chaudhuri P, Rankin JS, Conte JV. Trends and outcomes of tricuspid valve surgery in North America: an analysis of more than 50,000 patients from the Society of Thoracic Surgeons database. Ann Thorac Surg. 2013; 96:1546–1552. PMID:
24070702.

52. Zack CJ, Fender EA, Chandrashekar P, et al. National trends and outcomes in isolated tricuspid valve surgery. J Am Coll Cardiol. 2017; 70:2953–2960. PMID:
29241483.

53. Kawsara A, Alqahtani F, Nkomo VT, et al. Determinants of morbidity and mortality associated with isolated tricuspid valve surgery. J Am Heart Assoc. 2021; 10:e018417. PMID:
33399012.

54. Topilsky Y, Khanna AD, Oh JK, et al. Preoperative factors associated with adverse outcome after tricuspid valve replacement. Circulation. 2011; 123:1929–1939. PMID:
21518976.

55. Axtell AL, Bhambhani V, Moonsamy P, et al. Surgery does not improve survival in patients with isolated severe tricuspid regurgitation. J Am Coll Cardiol. 2019; 74:715–725. PMID:
31071413.

56. Ullah W, Sattar Y, Mukhtar M, et al. Outcomes of open mitral valve replacement versus transcatheter mitral valve repair; insight from the National Inpatient Sample database. Int J Cardiol Heart Vasc. 2020; 28:100540. PMID:
32490147.

57. Carroll JD, Mack MJ, Vemulapalli S, et al. STS-ACC TVT registry of transcatheter aortic valve replacement. J Am Coll Cardiol. 2020; 76:2492–2516. PMID:
33213729.

58. Suissa S. Immortal time bias in pharmaco-epidemiology. Am J Epidemiol. 2008; 167:492–499. PMID:
18056625.

59. von Ballmoos MC, Reardon MJ. Surgical treatment of severe tricuspid regurgitation. Curr Opin Cardiol. 2021; 36:538–541. PMID:
34397460.

60. McCarthy PM, Bhudia SK, Rajeswaran J, et al. Tricuspid valve repair: durability and risk factors for failure. J Thorac Cardiovasc Surg. 2004; 127:674–685. PMID:
15001895.

61. Van de Veire NR, Braun J, Delgado V, et al. Tricuspid annuloplasty prevents right ventricular dilatation and progression of tricuspid regurgitation in patients with tricuspid annular dilatation undergoing mitral valve repair. J Thorac Cardiovasc Surg. 2011; 141:1431–1439. PMID:
20832082.

62. Parolari A, Barili F, Pilozzi A, Pacini D. Ring or suture annuloplasty for tricuspid regurgitation? A meta-analysis review. Ann Thorac Surg. 2014; 98:2255–2263. PMID:
25443026.

63. Navia JL, Nowicki ER, Blackstone EH, et al. Surgical management of secondary tricuspid valve regurgitation: annulus, commissure, or leaflet procedure? J Thorac Cardiovasc Surg. 2010; 139:1473–1482.e5. PMID:
20394950.

64. Park SJ, Oh JK, Kim SO, et al. Determinants of clinical outcomes of surgery for isolated severe tricuspid regurgitation. Heart. 2021; 107:403–410. PMID:
33139325.

65. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021; 143:e35–e71. PMID:
33332149.
66. LaPar DJ, Likosky DS, Zhang M, et al. Development of a risk prediction model and clinical risk score for isolated tricuspid valve surgery. Ann Thorac Surg. 2018; 106:129–136. PMID:
29410187.

67. Glower DD. Surgical approaches to mitral regurgitation. J Am Coll Cardiol. 2012; 60:1315–1322. PMID:
22939558.

68. Suri RM, Clavel MA, Schaff HV, et al. Effect of recurrent mitral regurgitation following degenerative mitral valve repair: long-term analysis of competing outcomes. J Am Coll Cardiol. 2016; 67:488–498. PMID:
26846946.

69. Carpentier A. Cardiac valve surgery--the “French correction”. J Thorac Cardiovasc Surg. 1983; 86:323–337. PMID:
6887954.

70. Enriquez-Sarano M, Tajik AJ, Schaff HV, Orszulak TA, Bailey KR, Frye RL. Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation. Circulation. 1994; 90:830–837. PMID:
8044955.

71. Enriquez-Sarano M, Tajik AJ, Schaff HV, et al. Echocardiographic prediction of left ventricular function after correction of mitral regurgitation: results and clinical implications. J Am Coll Cardiol. 1994; 24:1536–1543. PMID:
7930287.

72. Grigioni F, Clavel MA, Vanoverschelde JL, et al. The MIDA Mortality Risk Score: development and external validation of a prognostic model for early and late death in degenerative mitral regurgitation. Eur Heart J. 2018; 39:1281–1291. PMID:
29020352.

73. Acker MA, Parides MK, Perrault LP, et al. Mitral-valve repair versus replacement for severe ischemic mitral regurgitation. N Engl J Med. 2014; 370:23–32. PMID:
24245543.
74. Asgar AW, Mack MJ, Stone GW. Secondary mitral regurgitation in heart failure: pathophysiology, prognosis, and therapeutic considerations. J Am Coll Cardiol. 2015; 65:1231–1248. PMID:
25814231.
75. Suri RM, Vanoverschelde JL, Grigioni F, et al. Association between early surgical intervention vs watchful waiting and outcomes for mitral regurgitation due to flail mitral valve leaflets. JAMA. 2013; 310:609–616. PMID:
23942679.

76. Kang DH, Park SJ, Lee SA, et al. Early surgery or conservative care for asymptomatic aortic stenosis. N Engl J Med. 2020; 382:111–119. PMID:
31733181.

77. Lee SW, Lee PH, Kim DH, et al. TCT-140 A novel device for TR reduction with a feature of “3D leaflet” hanging in the center of the tricuspid valve with an atraumatic anchoring mechanism: the Pivot-TR system. J Am Coll Cardiol. 2021; 78:B57.
78. Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012; 41:734–745. PMID:
22378855.

79. Shahian DM, He X, Jacobs JP, et al. The Society of Thoracic Surgeons isolated aortic valve replacement (AVR) composite score: a report of the STS Quality Measurement Task Force. Ann Thorac Surg. 2012; 94:2166–2171. PMID:
23127768.

80. Lee JH, Ko RE, Park TK, Cho YH, Suh GY, Yang JH. Association between a multidisciplinary team approach and clinical outcomes in patients undergoing extracorporeal cardiopulmonary resuscitation in the emergency department. Korean Circ J. 2021; 51:908–918. PMID:
34595885.

81. Taramasso M, Benfari G, van der Bijl P, et al. Transcatheter versus medical treatment of patients with symptomatic severe tricuspid regurgitation. J Am Coll Cardiol. 2019; 74:2998–3008. PMID:
31568868.

82. Nickenig G, Weber M, Lurz P, et al. Transcatheter edge-to-edge repair for reduction of tricuspid regurgitation: 6-month outcomes of the TRILUMINATE single-arm study. Lancet. 2019; 394:2002–2011. PMID:
31708188.

83. Taramasso M, Alessandrini H, Latib A, et al. Outcomes after current transcatheter tricuspid valve intervention: mid-term results from the International TriValve Registry. JACC Cardiovasc Interv. 2019; 12:155–165. PMID:
30594510.
84. Blanke P, Weir-McCall JR, Achenbach S, et al. Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR): an expert consensus document of the Society of Cardiovascular Computed Tomography. JACC Cardiovasc Imaging. 2019; 12:1–24. PMID:
30621986.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download