1. Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001; 285:2370–2375. PMID:
11343485.

2. Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006; 114:119–125. PMID:
16818816.

3. Corley SD, Epstein AE, DiMarco JP, et al. Relationships between sinus rhythm, treatment, and survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) Study. Circulation. 2004; 109:1509–1513. PMID:
15007003.

4. Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002; 347:1825–1833. PMID:
12466506.

5. Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010; 303:333–340. PMID:
20103757.

6. Packer DL, Mark DB, Robb RA, et al. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the cabana randomized clinical trial. JAMA. 2019; 321:1261–1274. PMID:
30874766.
7. Pappone C, Augello G, Sala S, et al. A randomized trial of circumferential pulmonary vein ablation versus antiarrhythmic drug therapy in paroxysmal atrial fibrillation: the APAF Study. J Am Coll Cardiol. 2006; 48:2340–2347. PMID:
17161267.

8. Marrouche NF, Brachmann J, Andresen D, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. 2018; 378:417–427. PMID:
29385358.

9. Verma A, Jiang CY, Betts TR, et al. Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med. 2015; 372:1812–1822. PMID:
25946280.

10. Kim YG, Choi JI, Boo KY, et al. Clinical and echocardiographic risk factors predict late recurrence after radiofrequency catheter ablation of atrial fibrillation. Sci Rep. 2019; 9:6890. PMID:
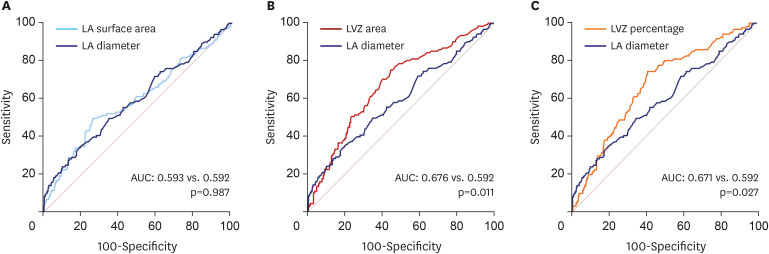
31053744.

11. Yamaguchi T, Tsuchiya T, Fukui A, et al. Impact of the extent of low-voltage zone on outcomes after voltage-based catheter ablation for persistent atrial fibrillation. J Cardiol. 2018; 72:427–433. PMID:
29807864.

12. Rolf S, Kircher S, Arya A, et al. Tailored atrial substrate modification based on low-voltage areas in catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 2014; 7:825–833. PMID:
25151631.

13. Marrouche NF, Wilber D, Hindricks G, et al. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA. 2014; 311:498–506. PMID:
24496537.

14. Kircher S, Arya A, Altmann D, et al. Individually tailored vs. standardized substrate modification during radiofrequency catheter ablation for atrial fibrillation: a randomized study. Europace. 2018; 20:1766–1775. PMID:
29177475.

15. Verma A, Wazni OM, Marrouche NF, et al. Pre-existent left atrial scarring in patients undergoing pulmonary vein antrum isolation: an independent predictor of procedural failure. J Am Coll Cardiol. 2005; 45:285–292. PMID:
15653029.

16. Kim YG, Shim J, Kim DH, et al. Characteristics of atrial fibrillation patients suffering atrioesophageal fistula after radiofrequency catheter ablation. J Cardiovasc Electrophysiol. 2018; 29:1343–1351. PMID:
29927012.

17. Kim YG, Han S, Choi JI, et al. Impact of persistent left superior vena cava on radiofrequency catheter ablation in patients with atrial fibrillation. Europace. 2019; 21:1824–1832. PMID:
31578551.

18. Kim YG, Han KD, Choi JI, et al. Non-genetic risk factors for atrial fibrillation are equally important in both young and old age: a nationwide population-based study. Eur J Prev Cardiol. 2021; 28:666–676. PMID:
34021574.

19. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983; 148:839–843. PMID:
6878708.

20. Kim YG, Shim J, Oh SK, Lee KN, Choi JI, Kim YH. Risk factors for ischemic stroke in atrial fibrillation patients undergoing radiofrequency catheter ablation. Sci Rep. 2019; 9:7051. PMID:
31065030.

21. Lee KN, Roh SY, Baek YS, et al. Long-term clinical comparison of procedural end points after pulmonary vein isolation in paroxysmal atrial fibrillation: Elimination of nonpulmonary vein triggers versus noninducibility. Circ Arrhythm Electrophysiol. 2018; 11:e005019. PMID:
29431632.

22. Haldar S, Khan HR, Boyalla V, et al. Catheter ablation vs. thoracoscopic surgical ablation in long-standing persistent atrial fibrillation: CASA-AF randomized controlled trial. Eur Heart J. 2020; 41:4471–4480. PMID:
32860414.

23. Corradi D, Callegari S, Maestri R, Benussi S, Alfieri O. Structural remodeling in atrial fibrillation. Nat Clin Pract Cardiovasc Med. 2008; 5:782–796. PMID:
18852714.

24. Corradi D. Atrial fibrillation from the pathologist’s perspective. Cardiovasc Pathol. 2014; 23:71–84. PMID:
24462196.

25. Allessie MA, de Groot NM, Houben RP, et al. Electropathological substrate of long-standing persistent atrial fibrillation in patients with structural heart disease: longitudinal dissociation. Circ Arrhythm Electrophysiol. 2010; 3:606–615. PMID:
20719881.

26. Myerburg RJ, Nilsson K, Befeler B, Castellanos A Jr, Gelband H. Transverse spread and longitudinal dissociation in the distal A-V conducting system. J Clin Invest. 1973; 52:885–895. PMID:
4693653.

27. Masuda M, Fujita M, Iida O, et al. Influence of underlying substrate on atrial tachyarrhythmias after pulmonary vein isolation. Heart Rhythm. 2016; 13:870–878. PMID:
26711800.

28. Matsuda Y, Masuda M, Asai M, et al. A new clinical risk score for predicting the prevalence of low-voltage areas in patients undergoing atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2020; 31:3150–3158. PMID:
32966648.

29. Sanders P, Morton JB, Davidson NC, et al. Electrical remodeling of the atria in congestive heart failure: electrophysiological and electroanatomic mapping in humans. Circulation. 2003; 108:1461–1468. PMID:
12952837.

30. Yang B, Jiang C, Lin Y, et al. STABLE-SR (electrophysiological substrate ablation in the left atrium during sinus rhythm) for the treatment of nonparoxysmal atrial fibrillation: a prospective, multicenter randomized clinical trial. Circ Arrhythm Electrophysiol. 2017; 10:e005405. PMID:
29141843.







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download