INTRODUCTION
Hypertension is the most common modifiable risk factor for cardiovascular disease, the leading cause of death worldwide.
1) In 2015, the estimated number of deaths that were associated with hypertension was 7.8 million, accounting for 14% of all deaths.
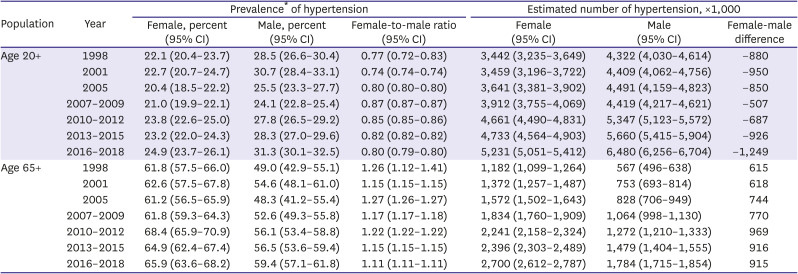
2) As of 2018, the prevalence of hypertension in Korea was estimated to be 29% in people aged 20 or older and 33% in people aged 30 or older.
3) According to the National Health Insurance Service database of Korea, the number of patients using medical service with diagnosis of hypertension increased from 3 million in 2002 to over 9 million in 2018. The estimated medical cost of treating hypertension was 3,830 billion Korean Won, accounting for 4% of all medical expenses or 16% of medical expenses for chronic diseases in 2019.
3)
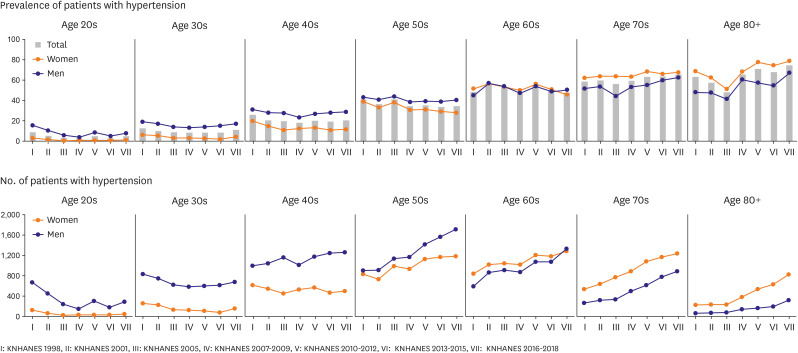
The prevalence of hypertension is known to be higher in men than in women, but not in all age groups. Blood pressure (BP) above normal range is highly common among elderly women, so the disease burden of hypertension is not less for women than men. Hypertension accounts for about 1 in 5 deaths of United States women and is a greater burden for women than men.
4) Among adult Americans, men present higher prevalence of hypertension and lower control rate compared to women. However, after age 60, women suffer from higher prevalence, lower control rate, and more complications of hypertension, compared to their male counterparts.
5) Despite these age- and sex- related differences in prevalence of hypertension, women are under-represented in many clinical studies.
6)
Korea is the world's fastest aging country, and the average life span difference between men and women is wide, resulting in a rapid increase in the elderly female population. However, there is only limited data on the prevalence and absolute number of hypertension in women compared to those in men.
7) Thus we analyzed national representative survey data to compare the prevalence of hypertension, the number of people with hypertension and their trends, between men and women.
DISCUSSION
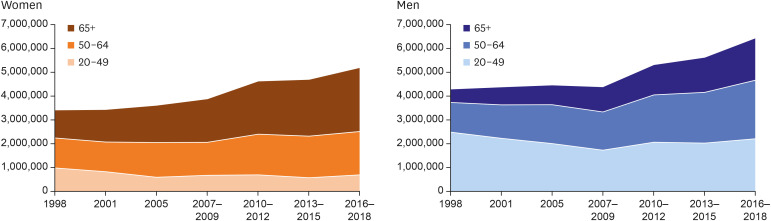
Over the last two decades, the estimated number of hypertension in men and women has steadily increased. In most parts of the world, including the United States, epidemic of obesity and the increasing detection rate of hypertension was the main contributing factors to the increasing number of people with hypertension. Between 1999 and 2014, the prevalence of obesity in adults in the United States increased significantly from 30.5% to 37.7%.
5) There was a significant linear increase in obesity from 2005 to 2014, especially in women. However, it is unlikely that the increase in the number of hypertensive patients in Korea is caused by changes in obesity or hypertension detection rate. In Korea, increase of obesity was observed in men but not in women.
8) In addition, national and private health checkups are very common in Korea, and the awareness rate of hypertension has not increased any more in recent years.
3) Therefore, the main factor that increase the number of hypertensive patients in Korea would be the increase in the elderly population. Since the prevalence of hypertension is higher among women in the elderly population,
2) it seems that the number of women with hypertension increases with the aging of society. The proportion of the of the population aged 65 and over in South Korea increased from 10.2% in 2008 to 16.4% in 2020, which corresponds to an aged society.
13)
In our study, the prevalence and the number of hypertension are lower in women than in men until age 60s and 50s, respectively, but increase later in life. The increasing prevalence of hypertension in older women was often explained by hormonal changes after menopause. Estrogen causes endothelial vasodilation via upregulation of the nitric oxide pathway and inhibition or down regulation of sympathetic and renin angiotensin system activity, as well as endothelin production.
14)15)16) Therefore, low postmenopausal estrogen levels may decrease arterial compliance and increase the risk of hypertension
17)18) and cardiovascular disease
6)18) in elderly women. Androgen deficiency after menopause also increases the risk of hypertension by increasing visceral obesity and contributing to adipocyte and endothelial dysfunction.
6) In addition to hormonal changes, anatomical and physiological sex differences may contribute to sex differences in hypertension prevalence in old age.
19)20) In association with the anatomical and physiological and sex differences of the heart and blood vessels, mean arterial pressure and pulse pressure increased faster in women than in men with aging.
21) Hypertension in women can be particularly harmful. Several studies found stronger association of hypertension with ischemic heart disease mortality and myocardial infarction in women than in men.
19) Pathological changes in blood vessels and heart in women with aging progress faster than in men, which is associated to the risk of coronary microvascular insufficiency and heart failure with preserved ejection,
21) which is primarily associated with arterial stiffness and hypertension.
22) Recently, hospitalization and mortality rates from heart failure have increased rapidly in Korea, and the rate of increase is much faster in women than in men.
23)
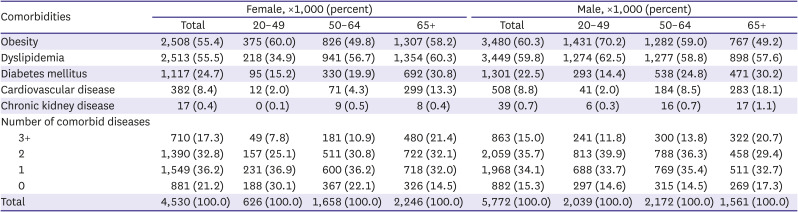
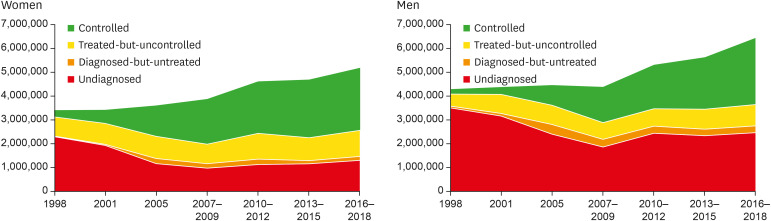
The proportion of treated-but-uncontrolled hypertension is higher in women than in men. In addition, stage 2 hypertension is more prevalent in elderly women than in elderly men, and the estimated number of elderly women with stage 2 hypertension is more than twice that of men. Hypertension accompanied by multiple chronic diseases is also more common in elderly women than in elderly men. Taken together, it can be interpreted that the number of hypertensive patients with difficulty in controlling BP and a high risk of cardiovascular disease is increasing rapidly, especially in elderly women.
A study of the United States primary care clinics reported that women aged 65 to 80 were less likely to control their BP than men of same age, even after adjusting for multiple factors.
24) Although biological aging related to endogenous stimulation seems to be a significant factor in the poor control of hypertension in women compared to men, the reasons for this sex difference are not clear.
6) In addition to biological aging, the possible explanations for this age-related decline in BP control among women may include poor lifestyle modification including lower physical activity, inadequate treatment in women and non-adherence to antihypertensive in elderly women.
4) In a nationally representative samples of adults in the United States, only 20.1% women reported participating in adequate physical activity that meets guidelines, and compared to 28.8% of men.
25) Co-existing risk factors or clinical sequelae in elderly women may cause difficulty in controlling BP despite treatment. Hypertension frequently occurs with multiple comorbidities that may amplify the cardiovascular risk of an affected individual or a specific population.
20) However, the factors lowering hypertension control rate in elderly women in Korea may be different from those in the Western population. Since Korean society has experienced huge changes over the past decades, there is a significant inter-generational difference also in gender inequality. Older women tend to be even more disadvantaged in education, occupation, and social networks than younger women. To improve BP control in elderly Korean women, further research is needed to evaluate the impact of biological, socioeconomic, behavioral factors as well as comorbidities on BP control.
This study has several limitations to be addressed. First, we cannot exclude the possibility of misclassification of hypertension. The KNHANES has measured BP values using a standard mercury sphygmomanometer, and employed quality control program of BP measurement. Nevertheless, changes in the screening environment and the BP measurement values may differ depending on the investigators. In addition, the BP readings were obtained on a single visit, so any variability in BP was not documented. Second, out-of-office BP measurement was not available. Therefore, we could not exclude white coat hypertension and could not include masked hypertension. Third, the KNHANES was designed to recruit representative sample of the Korean population, but institutionalized people were excluded from the sample. Thus, people with severe or complicated hypertension were less likely to be included. This might underestimate the prevalence and absolute number of hypertension.
In the younger and middle-aged adults, women tend to have lower prevalence and better management of hypertension than men, but in older women, the prevalence of hypertension increases rapidly, other comorbidities become frequent, and the BP control worsens. With the rapid aging, especially the surge in the elderly female population in Korea, the number of elderly women with hypertension and multi-comorbidities is rapidly increasing, which will be a serious public health challenge. A multi-pronged approach is needed to reduce the public health burden of hypertension in women. It is required to develop guidelines for the prevention and management of hypertension, which are tailored for different demographic groups. A population approach is also needed to increase awareness on the hypertension in women, and to achieve more thorough BP control especially for postmenopausal women.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download