Abstract
Purpose
As pancreaticojejunostomy (PJ) is a challenging anastomosis, an education program is needed to train young surgeons to perform PJ. This study evaluated the effects of simulation-based training of open PJ using pancreas and intestine silicone models.
Methods
Five videos pancreatobiliary clinical fellows who did not perform PJ participated in this study. After watching the master video created by a senior pancreatobiliary surgeon, each trainee performed the PJ using silicone models and recorded them 10 times using a video camera. Of these videos, 5 were randomly duplicated due to the validation of the scoring system. The scoring system developed consisted of 20 scores. Three pancreatobiliary professors scored their performance by watching videos.
Results
The mean procedure time of the 5 trainees was 25.4 minutes (range, 23.5–27.3 minutes) in the first video and 15.8 minutes (range, 13.8–19.1 minutes) in the 10th video. The mean score was 12.6 (range, 5–19) and 18.3 (range, 15–20) in the first and 10th videos, respectively. The scores were similar among the duplicated videos for each supervisor.
The surgical residents and clinical fellows learned surgical skills through apprenticeship, that is, by watching their supervisor’s operation and performing specific procedures directly in the operating room. However, owing to the complexity of recent surgery and shortage of education time [1], training in the operating room alone was insufficient to achieve skillful surgical techniques. Additionally, the surgical trainees should learn not only open but also laparoscopic or robotic surgical skills in the 21st century [2]. As the incapacity in the operating room may compromise patient safety and efficacy regarding the time use, it is important to become better-prepared surgical trainees with fundamental surgical techniques before real surgery [1]. Although learning during the actual operation would be ideal, it is unfeasible and unethical to the patients. Therefore, education programs using in vitro, in vivo, or virtual models are required to fulfill the needs of surgical trainees and achieve fundamental surgical techniques.
For intestinal anastomosis, which is a relatively simple and frequent procedure compared with other procedures, surgical residents of 3rd or 4th-year grade could perform it in the real operation under the supervision of a senior surgeon. However, in terms of pancreaticojejunostomy (PJ) anastomoses, surgical trainees rarely performed or even experienced them during the training period, particularly those in the low-volume center. As PJ is relatively rare compared with intestinal or vascular anastomosis and is related to life-threatening complications [3], the opportunity of performing the PJ by the trainees in the operating room is rare. Therefore, a training model for the PJ outside the operating room is necessary.
Several education models, such as simulation (dry-laboratory) models, or animal models, for intestinal or vascular anastomosis have already been developed [1456]. Recently, several education models for PJ anastomosis using biotissue models or animal models have been introduced and reported [7891011]. Although the animal model is more realistic than any other model, it has ethical issues and is expensive. Moreover, previous studies utilized the general objective structured assessment of technical skills (OSATS) for grading PJ performance [12], not the PJ-specific grading system, or introduced only their models and procedures. In this study, the silicone models which were similar to real intestine and pancreas were utilized, and the trainee’s surgical procedures were assessed by the PJ anastomosis-specific scoring system which was developed in our department. Therefore, this study aimed to evaluate the effectiveness of our PJ training model by observing the development of a trainee’s performance using a scoring system and to validate our scoring system.
This study protocol was approved by the Institutional Review Board in Seoul National University Hospital (No. H-2201-022-1286).
This was an uncontrolled, observational, prospective study. Five pancreatobiliary clinical fellows (3 sophomores and 2 juniors) performed the modified Blumgart open duct-to-mucosa PJ with a double-layer intestine and pancreas silicone model (SINI Inc., Uiwang, Korea) (Fig. 1). They participated in the surgery as the first assistant many times; however, never performed the open PJ themselves in the real surgical field before the simulation. The fellows performed the PJ simulation by following the master video. Fig. 2 shows the overall study design of this study. Each fellow performed 10 simulations and recorded them using a video camera. There was no supervisors’ feedback until the end of the 10 simulations. For the validation of the scoring system developed by our department, 5 video files from the original 10 files were randomly selected and duplicated. All 15 video files were randomly rearranged to eliminate bias derived from the drill order. Three pancreatobiliary professors assessed the trainees’ surgical skills by watching videos with the scoring system.
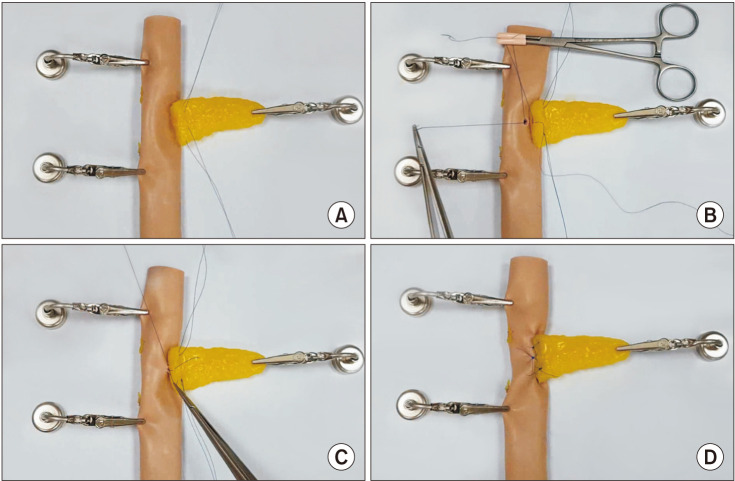
One pancreatobiliary professor (JYJ), who had performed over 1,000 pancreatoduodenectomies (PDs), demonstrated modified Blumgart PJ as he did in the real surgical field using the intestine and pancreas models and recorded the whole procedure [13]. Two transpancreatic U-shaped sutures were performed a few millimeters distal from the cut surface of the pancreatic stump, penetrating from the ventral to the dorsal side in full-thickness of the pancreas using 4-0 polypropylene (Surgipro, Covidien, Mansfield, MA, USA). Then, the seromuscular layer of the jejunal loop was sutured using the same stitch, and the stitch penetrated the pancreatic stump back from the dorsal to the ventral side (Fig. 3A). Avoiding the pancreatic duct, each transpancreatic U-suture was positioned on the superior and inferior border of the pancreatic duct, tied down but left uncut. Duct-to-mucosa anastomosis was performed using 5-0 polydioxanone (PDS II, Ethicon, Somerville, NJ, USA) in 5 to 6 different directions (Fig. 3B, C). With the uncut transpancreatic U-sutures, the ventral side of the jejunal loop was sutured in the seromuscular layer to conceal the resection surface of the pancreatic stump. Finally, an interrupted suture reinforcing PJ was performed between the 2 transpancreatic U-sutures in the central and ventral parts of the PJ (Fig. 3D).
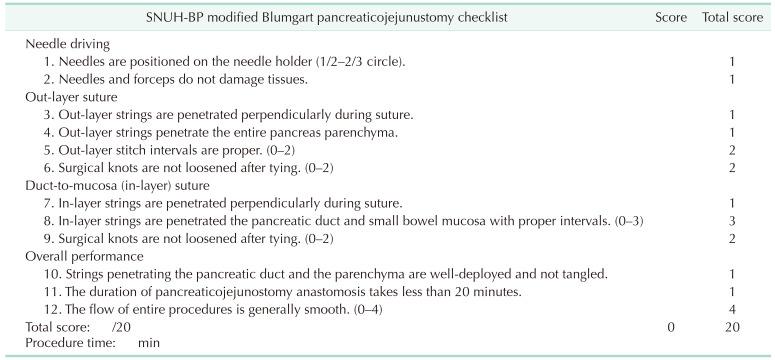
The OSATS-PJ was developed in the Department of Surgery, Seoul National University Hospital, based on the OSATS for surgical residents [12]. The original version of OSATS was modified to the specific surgical skills, such as vascular anastomosis, or intestinal anastomosis [114]. In this study, the OSATS-PJ was modified for modified Blumgart duct-to-mucosa PJ anastomosis. The detailed checklists are described in Table 1. There were 4 major categories: (1) needle driving, (2) out-layer transpancreatic U-shaped suture, (3) duct-to-mucosa suture, and (4) overall performance. Each category had 2–4 checklists (a total of 12 checklists), and the total score was 20. Additionally, the total procedure time was evaluated.
As a total of 15 videos of each participant were randomly rearranged, the supervisors did not notice duplicated video files or the order of procedures. After the acquisition of the total scores and total procedure times of each participant, these results were rearranged to the original order and analyzed. Means and ranges were employed for the numerical variables. For the reproducibility of OSATS-PJ, the scores of 5 duplicated videos were compared with those of 5 original videos among the 3 supervisors. Statistical analysis was conducted using R software version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria).
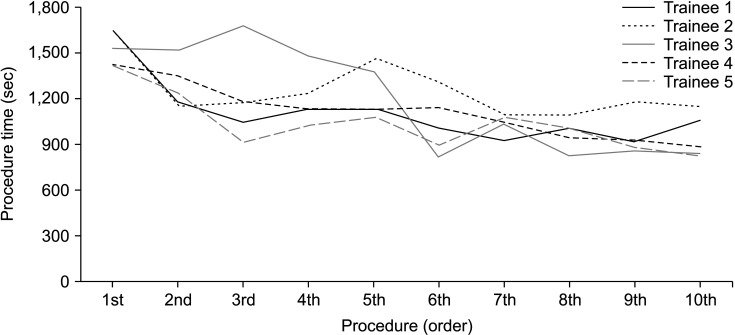
The mean procedure time of the 5 trainees was 25.4 minutes (range, 23.5–27.3 minutes) in the first video and 15.8 minutes (range, 13.8–19.1 minutes) in the 10th video. The procedure times of all 5 trainees showed a decreasing tendency as in the latter procedure (Fig. 4). From the 7th procedure, the total procedure time converged between 15 and 20 minutes.
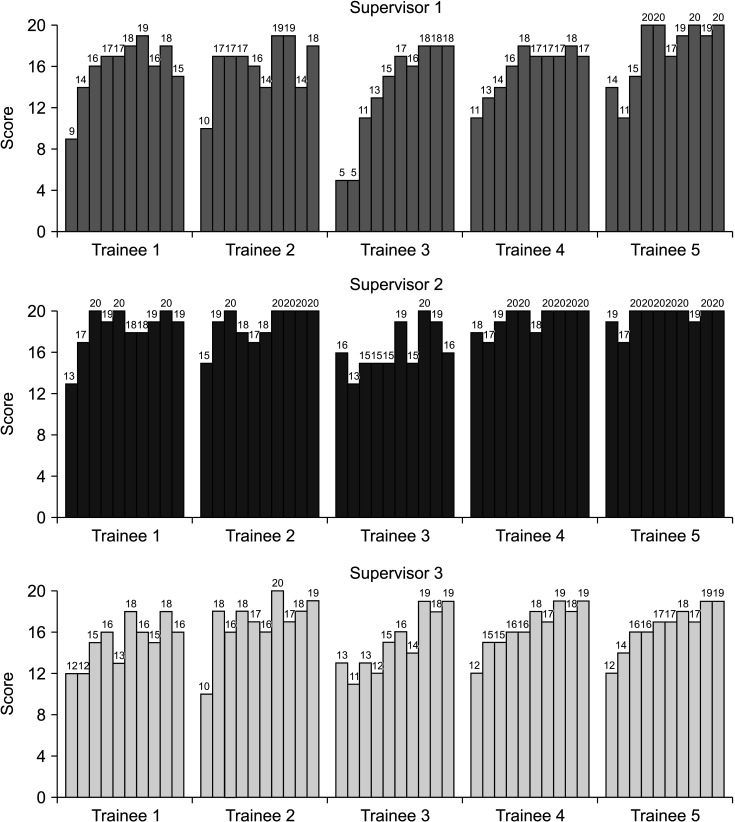
The mean score of the 5 trainees was 12.6 (range, 5–19) in the first videos, and 18.3 (range, 15–20) in the 10th video. Fig. 5 shows the histogram of the total score of the 5 trainees according to each supervisor. The total score demonstrated an increasing tendency as in the latter procedures. Most of the 7th and later procedures obtained a total score of 16 or above, that is, at least 7 practice sessions would be minimal for a stable PJ anastomosis.
Since 5 original video files were randomly selected and duplicated, each supervisor judged an additional 25 video files. Then, the difference in scores between the original and duplicated video files was evaluated. Table 2 shows that the scores were identical, or a difference of 1 point in 71 drills (94.7%).
PD is one of the most complex procedures in abdominal surgery, and its complication rate is still high. In particular, postoperative pancreatic fistula (POPF), which can cause life-threatening complications, is inevitable. One study reported that the surgeon’s performance was correlated with the development of POPF [3]. For the quality of surgery and patient’ safety, sufficient practice is needed. Several studies have reported that more than 60 cases of standard PD are needed to overcome the learning curve [1516]. However, all pancreatobiliary surgical fellows cannot perform more than 60 cases in the training period, even in large-volume centers. Furthermore, it is unethical for unprepared trainees to perform the surgical procedures directly on patients [17]. Therefore, simulation-based training for repetitive practices is essential to improve surgical skills before actual practice.
There were 3 categories of education models: (1) animal, (2) simulation, and (3) virtual reality. Regarding PJ, 1 institution developed a porcine model for open and laparoscopic PJ [7]. The porcine model has an advantage in that the trainees can train their surgical techniques in live animals with similar intraabdominal organs to those of humans. This model is the most realistic. However, the cost is much more expensive than the other 2 models, the preparation before and after the training requires time and effort, and ethical issues exist. The simulation model is the most popular method as it is relatively inexpensive and requires no special space or preparation procedure. It can be divided into 2 subcategories; biotissue model and silicone model. Although the biotissue model is more delicate and realistic than the silicone model and has already been utilized in another study [9], it needs special 3-dimensional bioprinting techniques and special materials, is more expensive than the silicone model, and mass production is difficult. Virtual-reality models are appropriate for laparoscopic or robotic surgery and have become popular [18]. However, considering that these models are expensive and require special equipment, it is only possible to install them in highly selective educational institutions. We selected the silicone model as the appropriate open PJ training model considering the lowest cost and no requirement for animal and expensive equipment.
In the present study, a double-layered intestine model and pancreatic model with a 3-mm small pancreatic duct manufactured by a Korean company (SINI Inc.) were utilized (Fig. 1). The size, texture, and strength were similar to those of humans. Furthermore, the repetition of 5–10 PJ was possible with 1 intestine and pancreas model. Considering that the cost of 1 intestine and 1 pancreas model was 400 US dollars, it is efficient and economical.
Several studies revealed that the trainee’s performance improved after the simulation training of PJ anastomosis using a simulation model [811]. In this study, the total procedure time and total score of OSATS-PJ were evaluated. The total procedure times were stabilized after the 7th drill and converged to 15–20 minutes (Fig. 4). The total scores increased, and in most cases of the 7th drill and after 16 or more scores were obtained (Fig. 5). Alternatively, at least 7 practices would be minimal for performing stable PJ anastomosis. After 10 simulations, our clinical fellows could similarly perform the real open PJ anastomosis. The total procedure time was 21 minutes, and the total score was 17. Although the operation time was slightly longer in the real PJ, they performed exactly step-by-step and did not hesitate in the next step. Additionally, the trainees repeated the PJ anastomoses themselves without feedback from supervisors. Therefore, the present training system would be effective for improving PJ anastomosis skills by self-training and able to achieve the fundamental level of performing PJ anastomosis in the real surgical field. Currently, clinical fellows train their robotic PJ techniques similar to the real robotic PJ with the same PJ training model [19], and research on robotic PJ training is now in progress. We anticipate that the present PJ training model would be effective in robotic PJ training, similar to open PJ training.
In this study, the OSATS-PJ was derived from the original OSATS and focused on the modified Blumgart duct-to-mucosa PJ anastomosis. It consisted of 12 definite checklists that indicated specific procedures sequentially (Table 1). Therefore, supervisors can easily assess each procedure individually and objectively grade the entire performance. Additionally, this scoring system was modifiable so that the supervisors could revise the specific steps tailored to the surgical procedures of their institution. To investigate the reproducibility of the scoring system, 5 videos were randomly selected and duplicated. When comparing the scores between the original and duplicated videos for each supervisor, the proportion of cases with identical scores or a difference of 1 was 88.0%, 96.0%, and 100.0%, respectively (Table 2). Therefore, the proposed scoring system has objectivity and reproducibility. Furthermore, this scoring system can be applied not only to open PJ anastomosis but also to laparoscopic or robotic PJ anastomosis during real operation.
In conclusion, the present open PJ training model with silicone models was effective in improving trainees’ surgical skills. Since this model does not have ethical issues nor requires expensive equipment, it can be introduced easily and practically to the field of surgical education.
References
1. Egle JP, Malladi SV, Gopinath N, Mittal VK. Simulation training improves resident performance in hand-sewn vascular and bowel anastomoses. J Surg Educ. 2015; 72:291–296. PMID: 25481803.

2. Fonseca AL, Evans LV, Gusberg RJ. Open surgical simulation in residency training: a review of its status and a case for its incorporation. J Surg Educ. 2013; 70:129–137. PMID: 23337682.

3. Hogg ME, Zenati M, Novak S, Chen Y, Jun Y, Steve J, et al. Grading of surgeon technical performance predicts postoperative pancreatic fistula for pancreaticoduodenectomy independent of patient-related variables. Ann Surg. 2016; 264:482–491. PMID: 27433897.

4. Davies J, Khatib M, Bello F. Open surgical simulation: a review. J Surg Educ. 2013; 70:618–627. PMID: 24016373.
5. Santos DR, Calvo FC, Feijó DH, Araújo NP, Teixeira RK, Yasojima EY. New training model using chickens intestine for pediatric intestinal anastomosis. Acta Cir Bras. 2019; 34:e201900709. PMID: 31531529.

6. Uemura M, Yamashita M, Tomikawa M, Obata S, Souzaki R, Ieiri S, et al. Objective assessment of the suture ligature method for the laparoscopic intestinal anastomosis model using a new computerized system. Surg Endosc. 2015; 29:444–452. PMID: 25005015.

7. Choi M, Kang CM. Developing an in vivo porcine model of duct-to-mucosa pancreaticojejunostomy (Yonsei-PJDTM). Ann Gastroenterol Surg. 2020; 4:180–184. PMID: 32258985.

8. Tam V, Zenati M, Novak S, Chen Y, Zureikat AH, Zeh HJ 3rd, et al. Robotic pancreatoduodenectomy biotissue curriculum has validity and improves technical performance for surgical oncology fellows. J Surg Educ. 2017; 74:1057–1065. PMID: 28578981.

9. Wei F, Xu M, Lai X, Zhang J, Yiengpruksawan A, Lu Y, et al. Three-dimensional printed dry lab training models to simulate robotic-assisted pancreaticojejunostomy. ANZ J Surg. 2019; 89:1631–1635. PMID: 31692187.

10. Yang JR, Xiao R, Zhou J, Wang L, Wang JX, Zhang Q, et al. Establishment of a canine training model for digestive tract reconstruction after pancreaticoduodenectomy. J Invest Surg. 2021; 34:561–567. PMID: 31588822.

11. Yoshioka R, Imamura H, Ichida H, Gyoda Y, Mizuno T, Mise Y, et al. Simulation training in pancreatico-jejunostomy using an inanimate biotissue model improves the technical skills of hepatobiliary-pancreatic surgical fellows. PLoS One. 2021; 16:e0244915. PMID: 33439895.

12. Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997; 84:273–278. PMID: 9052454.

13. Byun Y, Choi YJ, Han Y, Kang JS, Kim H, Kwon W, et al. Outcomes of 5000 pancreatectomies in Korean single referral center and literature reviews. J Hepatobiliary Pancreat Sci. 2021; 02. 26. DOI: 10.1002/jhbp.933. [Epub].

14. Malas T, Al-Atassi T, Brandys T, Naik V, Lapierre H, Lam BK. Impact of visualization on simulation training for vascular anastomosis. J Thorac Cardiovasc Surg. 2018; 155:1686–1693. PMID: 29554789.

15. Fisher WE, Hodges SE, Wu MF, Hilsenbeck SG, Brunicardi FC. Assessment of the learning curve for pancreaticoduodenectomy. Am J Surg. 2012; 203:684–690. PMID: 22079032.

16. Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010; 145:634–640. PMID: 20644125.

17. Ziv A, Wolpe PR, Small SD, Glick S. Simulation-based medical education: an ethical imperative. Simul Healthc. 2006; 1:252–256. PMID: 19088599.

18. Alaker M, Wynn GR, Arulampalam T. Virtual reality training in laparoscopic surgery: a systematic review & meta-analysis. Int J Surg. 2016; 29:85–94. PMID: 26992652.

19. Kim HS, Han Y, Kang JS, Kim H, Kim JR, Kwon W, et al. Comparison of surgical outcomes between open and robot-assisted minimally invasive pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2018; 25:142–149. PMID: 29117639.

Fig. 1
Pancreas and intestine models used in this study. They are made of silicone and the cost of 1 pancreas and 1 intestine is 400 US dollars.
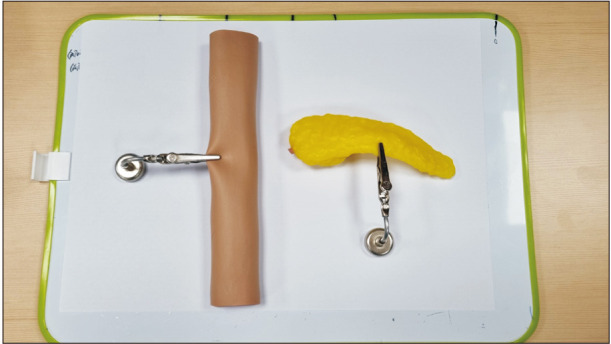
Fig. 2
Overall flowchart of study design. Ten original video files were recorded and 5 video files were randomly selected and duplicated. After the rearrangement of total 15 video files, they were sent to each supervisor.
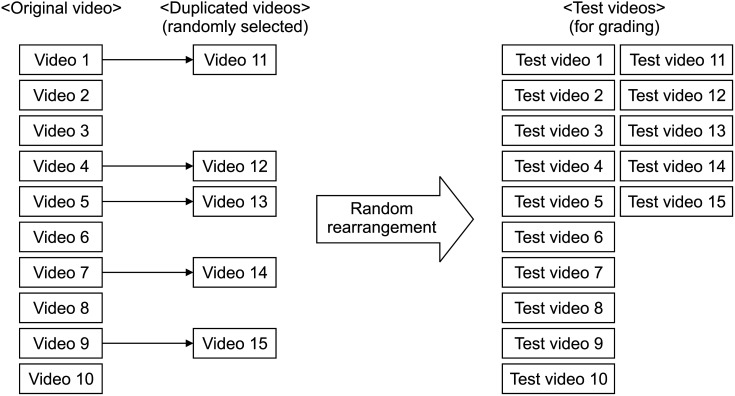
Fig. 3
The still-cut images of the master video. (A) Two transpancreatic U-shaped sutures were established. Duct-to-mucosa sutures were performed in the dorsal side (B) and in the ventral side (C). (D) The uncut transpancreatic U-sutures and the interrupted sutures were performed in the ventral and central part of the pancreaticojejunostomy.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download