Abstract
Purpose
The incidence of patients requiring pancreaticoduodenectomy (PD) following any type of gastrectomy is increasing as the population of elderly patients is increasing, especially in endemic areas of gastric cancer such as Korea. All types of gastrectomy can be categorized as subtotal gastrectomy with Billroth I (BI), Billroth II (BII), and total gastrectomy with Roux-en-Y anastomosis. In this paper, we reviewed our experiences of PD for patients who previously underwent gastrectomy.
Methods
We reviewed the medical records of the patients who underwent PD following any type of gastrectomy among 505 consecutive patients who underwent PD in a single institution between 2011 and 2020 retrospectively.
Results
There were 13 patients who had undergone gastrectomy including 7 patients of BI, 1 patient of BII, and 5 patients of total gastrectomy. For all 7 patients of BI, the reconstruction was not different from conventional PD. For the 1 patient of BII, previous gastrojejunal anastomosis was preserved and reconstruction was performed in Roux-en-Y method. For the 5 patients with total gastrectomy, 2 different types of reconstruction were performed. In one patient, we removed the remaining jejunum with the specimen, and reconstruction was performed. For the other 4 patients, the remaining jejunum, distal to the Treitz ligament, was preserved and was utilized for anastomosis. Surgeries for all patients were uneventful.
Due to the rapid rate of prolonged life expectancy and improvement of medical technology, the incidence of elderly patients is increasing. Accordingly, the incidence of patients diagnosed with secondary cancer has also increased. It was reported that the occurrence of secondary cancer has risen to approximately 19% [1]. In accordance with this global trend, it is expected that the incidence of patients requiring pancreaticoduodenectomy (PD) for periampullary cancer following any type of gastrectomy would be increasing, especially in endemic areas of gastric cancer such as Korea. Gastric cancers can be divided into non-cardia types which are related to Helicobacter pylori infection and cardia type. The treatment and prevention of H. pylori increased the proportion of cardia type among all gastric cancers [2]. As a result, it was anticipated that the proportion of patients who underwent total gastrectomy will be increased in clinical practice.
PD is a major abdominal surgery demanding cautious dissection along critical vascular structures and 3 complex anastomoses of the jejunum to pancreatic duct, bile duct, and gastric outlet. For this reason, when surgeons perform PD for a patient who previously underwent gastrectomy, they must overcome hurdles during resection due to severe adhesion and must select the proper types of reconstruction. The proper types of reconstruction can vary depending on the type of gastrectomy and the status, especially the length of the jejunum distal to the Treitz ligament.
All types of gastrectomy can be categorized as subtotal gastrectomy with Billroth I (BI), Billroth II (BII), and total gastrectomy with Roux-en-Y anastomosis. For the BI patient, resection and reconstruction are not different from conventional PD. However, for the BII patient or total gastrectomy with Roux-en-Y loop, reconstruction can vary according to the status of the remaining jejunum distal to the Treitz ligament.
In this paper, we reviewed our experiences of PD for patients who previously underwent all types of gastrectomy.
This study has been approved by the Research Ethics Committee of Kyungpook National University Chilgok Hospital (No. KNUCH 2022-01-032). This study was performed in accordance with the Declaration of Helsinki and written informed consent was waived due to its retrospective nature.
We reviewed the medical records of patients who underwent PD following any type of gastrectomy among 505 consecutive patients who underwent PD in a single institution between 2011 and 2020 retrospectively. There were 13 patients (2.6%) who had undergone gastrectomy including 7 patients of BI, 1 patient of BII, and 5 patients of total gastrectomy with Roux-en-Y. We collected the data of patient demographics including age, sex, body mass index, and comorbidities. Operative parameters are the methods of reconstruction, operative time, hospitalization day, and postoperative complications.
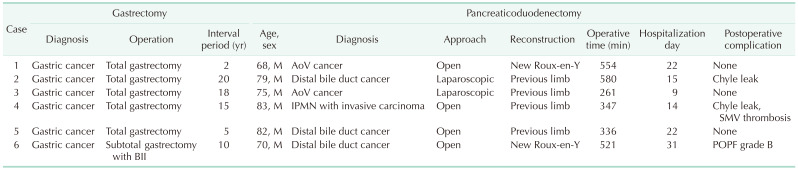
For all 7 patients of BI, resection and reconstruction were not different from conventional PD (Fig. 1). The other characteristics, such as classification of precedent gastrectomy and perioperative parameters for PD, are summarized in Table 1.
All of the previous gastrectomies were open surgery. Four patients underwent open PD and 2 patients underwent laparoscopic PD. The median operative time for PD was 433 minutes (range, 261–580 minutes) and median hospital days were 19 days (range, 9–31 days).
One patient (No. 6) previously underwent subtotal gastrectomy with BII anastomosis. The resection was performed dividing the afferent jejunum near the left corner of the gastrojejunostomy. New Roux-en-Y reconstruction was performed using a distal jejunum (Fig. 2). This patient suffered grade B postoperative pancreatic fistula by the definition of the international study group pancreatic surgery [3]. The patient recovered without reoperation or intervention procedure.
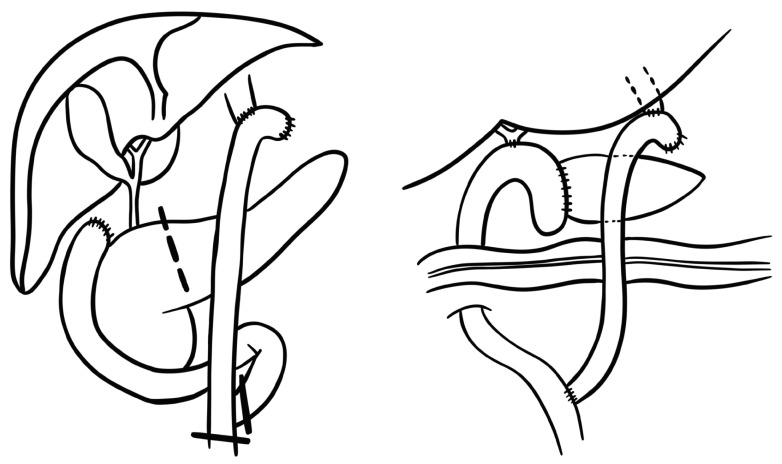
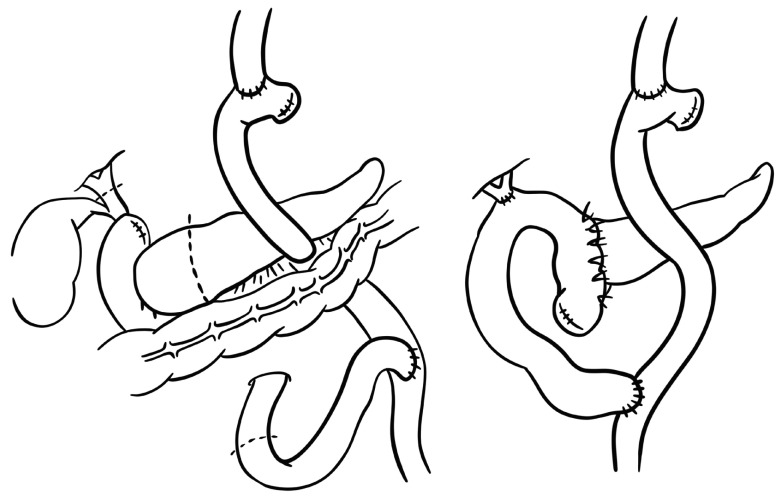
For the 5 patients with total gastrectomy with Roux-en-Y reconstruction, 2 different types of reconstruction were performed. For one patient, we removed the remaining jejunum distal to the Treitz ligament combined with the specimen leaving a 2-cm stump from the previous jejunojejunostomy, and new Roux-en-Y reconstruction was performed (Fig. 3). For the other 4 patients, the remaining jejunum distal to the Treitz ligament was preserved during the resection and it was utilized for the pancreaticojejunostomy and hepaticojejunostomy because the length of jejunum was long enough to avoid tension (Fig. 4). Among these 4 patients, 2 patients underwent laparoscopic PD, and the other 2 patients underwent open surgery. Chyle leakage occurred in 2 patients and was treated with low-fat diet. Superior mesenteric vein thrombosis occurred in 1 patient and was treated with an anticoagulant.
Gastric cancer is the fifth most commonly diagnosed cancer in the world. The Republic of Korea is one of the countries with the highest national incidence in the world [2]. The survival of gastric cancer has dramatically improved. A recent study showed that the 5-year survival rate of the period from 2013 to 2017 was higher (76.5%) compared to that of the period from 1993 to 1995 (43.9%) [4]. Similar to gastric cancer, the tendency of increasing survival from other primary cancers is also reported due to early detection and improvement of medical technology, which lead to an increase of second primary cancer [15].
In accordance with the global trend of prolonged life expectancy and high prevalence of gastric cancer in Korea, it is expected that the demand of PD for periampullary cancer following gastrectomy would increase further in the future.
There would be many challenges for surgeons to reoperate on patients who had previously received other abdominal surgeries due to normal anatomical structures being altered and the healing process accompanied by natural adhesion. The clinical implications are more significant when secondary tumors occur in the periampullary region and precedent surgery is performed for gastric cancer. Surgery for gastric cancer alters the gastrointestinal tract significantly and extensive lymph node dissection leads to severe adhesion after surgery. In addition, the proportion of cardia-type gastric cancer requiring total gastrectomy is increasing. In this situation, the demand for PD for periampullary tumors is accompanied by hurdles difficult to overcome. In this report, we shared our experience of PD after gastrectomy.
In our results, the median interval time from the first gastrectomy to secondary PD was quite long; 11 years and 6 months (range, 2–20 years).
For patients with BI reconstruction after gastrectomy, the process of resection is the same as conventional PD, even though it requires meticulous dissection due to severe adhesion.
In most of our cases, adhesion was not an interrupting factor, even though it required great caution. The division line of the duodenum was just 1 to 2 cm distal to the previous gastroduodenostomy. Although the color of the duodenum was different from those of conventional PD, we experienced no complication of duodenojejunostomy. We concluded that the blood supply to the duodenum is well maintained even though the duodenum looked pale.
For the patients of total gastrectomy with Roux-en-Y reconstruction, 2 different methods were applied depending on the status of remaining jejunum distal to the Treitz ligament. For 2 patients, we utilized the remaining jejunum for pancreaticojejunostomy and hepaticojejunostomy; and for the other 2 patients, we utilized Roux-en-Y method sacrificing the remaining jejunum distal to the Treitz ligament.
For experienced surgeons, it is known that the history of previous gastrectomy is not associated with clinical outcomes of PD [6], yet there is no guideline or consensus on methods of reconstruction after previous total gastrectomy with Roux-en-Y reconstruction.
In this paper, we utilized Roux-en-Y reconstruction in 1 patient and we used the previous remaining jejunum for reconstruction in 4 cases. Some authors utilized the previous remaining jejunum for reconstruction as we did. However, they reported that afferent loop syndrome (ALS) was observed in 2 of 3 cases when they used the remaining jejunum for pancreatic and biliary reconstruction. They reported that surgical correction making a new Y-limb resolved the symptom immediately, and the reason for the ALS was the short length of the remaining jejunum utilized for the reconstruction [7]. Based on their experience, they recommended that the previously remaining jejunum distal to the Treitz ligament may not be used for anastomosis [89]. ALS is usually caused by mechanical obstruction due to internal hernia, recurrence, adhesion, or torsion of the afferent limb. Decreased jejunal motility caused by inappropriate length of an afferent limb can lead to biliary stasis and nonobstructive ALS [10]. It was considered that short length of a remaining jejunum distal to the Treitz ligament used in reconstruction is the cause of ALS.
However, according to our experience, if the length of the jejunum is long enough to avoid tension, utilization of remaining jejunum distal to the Treitz ligament for reconstruction has advantage in the aspect of shortening operative time and avoiding new anastomosis of the jejunum.
In conclusion, PD following any type of gastrectomy can be safely performed and, if possible, utilization of the remaining jejunum distal to the Treitz ligament can be an appropriate option.
References
1. Morton LM, Onel K, Curtis RE, Hungate EA, Armstrong GT. The rising incidence of second cancers: patterns of occurrence and identification of risk factors for children and adults. Am Soc Clin Oncol Educ Book. 2014; e57–e67. PMID: 24857148.

2. Rawla P, Barsouk A. Epidemiology of gastric cancer: global trends, risk factors and prevention. Prz Gastroenterol. 2019; 14:26–38. PMID: 30944675.

3. Pulvirenti A, Ramera M, Bassi C. Modifications in the International Study Group for Pancreatic Surgery (ISGPS) definition of postoperative pancreatic fistula. Transl Gastroenterol Hepatol. 2017; 2:107. PMID: 29354764.

4. Hong S, Won YJ, Park YR, Jung KW, Kong HJ, Lee ES, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2017. Cancer Res Treat. 2020; 52:335–350. PMID: 32178489.

5. Kanninen TT, Nasioudis D, Sisti G, Holcomb K, Di Tommaso M, Khalil S, et al. Epidemiology of second primary tumors in women with ovarian cancer. Int J Gynecol Cancer. 2017; 27:659–667. PMID: 28441249.

6. Kim JR, Kwon W, Chang J, Jang JY, Kim SW. Comparison of clinical outcomes according to the history of previous gastrectomy in patients undergoing pancreatoduodenectomy: a propensity score matching analysis. Ann Surg Treat Res. 2020; 98:177–183. PMID: 32274365.

7. Yokoyama S, Sekioka A, Ueno K, Higashide Y, Okishio Y, Kawaguchi N, et al. Pancreaticoduodenectomy following total gastrectomy: a case report and literature review. World J Gastroenterol. 2014; 20:2721–2724. PMID: 24627609.

8. Yokoyama S, Ueno K, Higashide Y, Noma A, Okishio Y, Masuda M, et al. Short- and long-term outcomes after pancreaticoduodenectomy following total gastorectomy: report of case series and literature review. Int J Surg Case Rep. 2017; 30:118–121. PMID: 28012325.

9. Kawamoto Y, Ome Y, Kouda Y, Saga K, Park T, Kawamoto K. Pancreaticoduodenectomy following gastrectomy reconstructed with Billroth II or Roux-en-Y method: case series and literature review. Int J Surg Case Rep. 2017; 35:106–109. PMID: 28477562.

10. Sanada Y, Yamada N, Taguchi M, Morishima K, Kasahara N, Kaneda Y, et al. Recurrent cholangitis by biliary stasis due to non-obstructive afferent loop syndrome after pylorus-preserving pancreatoduodenectomy: report of a case. Int Surg. 2014; 99:426–431. PMID: 25058778.

Fig. 1
Reconstruction of pancreaticoduodenectomy (PD) following subtotal gastrectomy with a Billroth I. The surgery was not different from conventional PD.
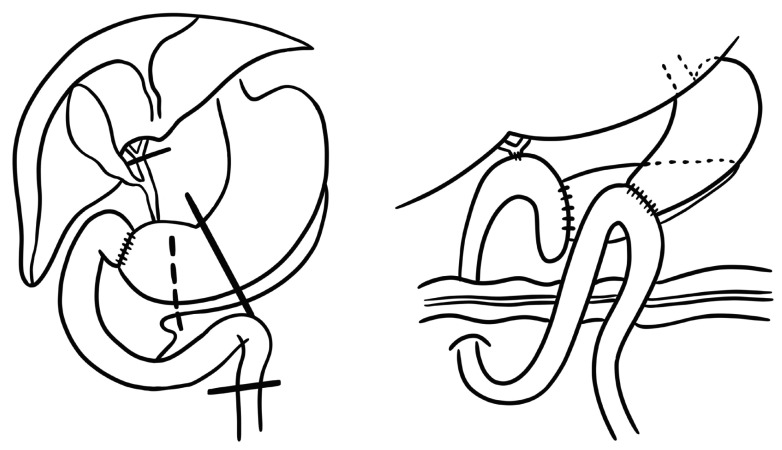
Fig. 2
Reconstruction of pancreaticoduodenectomy following subtotal gastrectomy with a Billroth II. Previous gastrojejunal anastomosis was preserved.
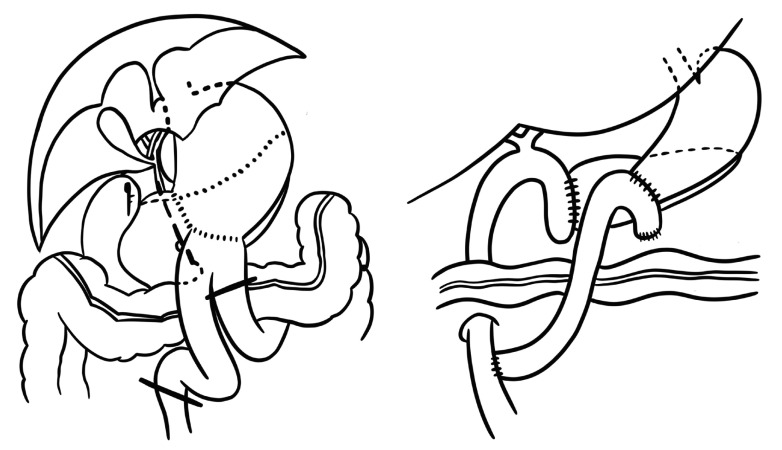
Fig. 3
Reconstruction of pancreaticoduodenectomy following total gastrectomy with Roux-en-Y method. We removed the remained jejunum distal to Treitz ligament with the specimen and new reconstruction was performed in Roux-en-Y method.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download