1. Mahase E. Covid-19: England’s obesity strategy will fail without tackling social factors, warn doctors. BMJ. 2020; 370:m2994. PMID:
32718928.
2. Kim M, Khang YH. Inequalities in longitudinal health trajectories in middle to later life: a comparison of European countries and Korea. J Korean Med Sci. 2020; 35(21):e141. PMID:
32476301.
3. Gubrium A, Gubrium E. Narrative complexity in the time of COVID-19. Lancet. 2021; 397(10291):2244–2245. PMID:
34119055.
4. Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, et al. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet. 2015; 386(10007):1973–2028. PMID:
26188744.
5. Worsley-Tonks KE, Bender JB, Deem SL, Ferguson AW, Fèvre EM, Martins DJ, et al. Strengthening global health security by improving disease surveillance in remote rural areas of low-income and middle-income countries. Lancet Glob Health. 2022; 10(4):e579–e584. PMID:
35303467.
6. Declaration of ALMA-ATA. Am J Public Health. 2015; 105(6):1094–1095. PMID:
25970470.
7. Walsh JA, Warren KS. Selective primary health care: an interim strategy for disease control in developing countries. N Engl J Med. 1979; 301(18):967–974. PMID:
114830.
10. Al Knawy B, Adil M, Crooks G, Rhee K, Bates D, Jokhdar H, et al. The Riyadh Declaration: the role of digital health in fighting pandemics. Lancet. 2020; 396(10262):1537–1539. PMID:
32976771.
11. Myers SS, Pivor JI, Saraiva AM. The São Paulo Declaration on planetary health. Lancet. 2021; 398(10308):1299.
12. Fee E, Brown TM. A return to the social justice spirit of Alma-Ata. Am J Public Health. 2015; 105(6):1096–1097. PMID:
25880948.
13. Walker R, Hassall J, Chaplin S, Congues J, Bajayo R, Mason W. Health promotion interventions to address climate change using a primary health care approach: a literature review. Health Promot J Austr. 2011; 22(Spec No):S6–12. PMID:
22518912.
14. Ruano AL. The role of social participation in municipal-level health systems: the case of Palencia, Guatemala. Glob Health Action. 2013; 6(1):20786. PMID:
24028936.
15. Gorry C. Six decades of Cuban Global Health Cooperation. MEDICC Rev. 2019; 21(4):83–92. PMID:
32335576.
17. Brolan CE, Te V, Floden N, Hill PS, Forman L. Did the right to health get across the line? Examining the United Nations resolution on the Sustainable Development Goals. BMJ Glob Health. 2017; 2(3):e000353.
18. Asma S, Lozano R, Chatterji S, Swaminathan S, de Fátima Marinho M, Yamamoto N, et al. Monitoring the health-related Sustainable Development Goals: lessons learned and recommendations for improved measurement. Lancet. 2020; 395(10219):240–246. PMID:
31767190.
19. Jungo KT, Anker D, Wildisen L. Astana declaration: a new pathway for primary health care. Int J Public Health. 2020; 65(5):511–512. PMID:
32318780.
20. The Lancet. The Astana Declaration: the future of primary health care? Lancet. 2018; 392(10156):1369. PMID:
30343840.
21. Davletov K, Nurgozhin T, McKee M. Reflecting on Alma Ata 1978: forty years on. Eur J Public Health. 2018; 28(4):587. PMID:
30020518.
22. The Lancet Infectious Diseases. The Astana Declaration: time to focus on primary health care. Lancet Infect Dis. 2018; 18(12):1289. PMID:
30507443.
23. Kraef C, Kallestrup P. After the Astana declaration: is comprehensive primary health care set for success this time? BMJ Glob Health. 2019; 4(6):e001871.
24. The Lancet Global Health. The price of primary care: from evidence to action. Lancet Glob Health. 2022; 10(5):e585. PMID:
35427501.
25. Rasanathan K, Evans TG. Primary health care, the Declaration of Astana and COVID-19. Bull World Health Organ. 2020; 98(11):801–808. PMID:
33177777.
26. Edelman A, Marten R, Montenegro H, Sheikh K, Barkley S, Ghaffar A, et al. Modified scoping review of the enablers and barriers to implementing primary health care in the COVID-19 context. Health Policy Plan. 2021; 36(7):1163–1186. PMID:
34185844.
27. Mahler H. The Meaning of “Health for All by the Year 2000”. Am J Public Health. 2016; 106(1):36–38. PMID:
26696287.
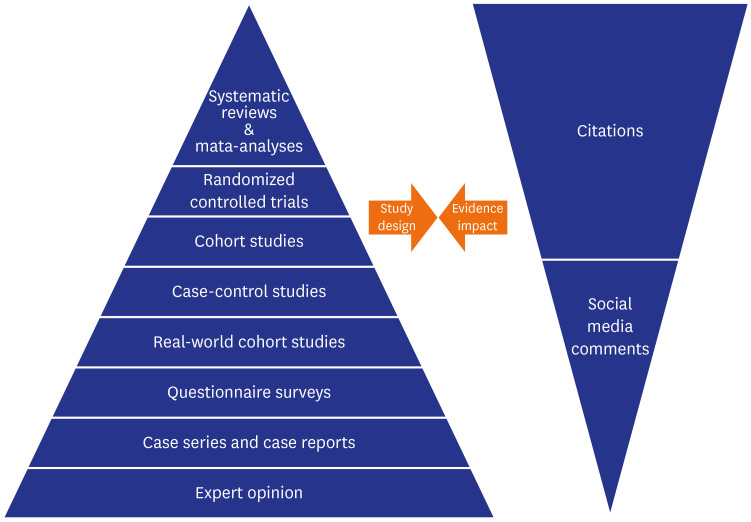
28. Murad MH, Asi N, Alsawas M, Alahdab F. New evidence pyramid. Evid Based Med. 2016; 21(4):125–127. PMID:
27339128.
29. Misra DP, Agarwal V. Real-world evidence in rheumatic diseases: relevance and lessons learnt. Rheumatol Int. 2019; 39(3):403–416. PMID:
30725156.
30. McNair D, Lumpkin M, Kern S, Hartman D. Use of RWE to inform regulatory, public health policy, and intervention priorities for the developing world. Clin Pharmacol Ther. 2022; 111(1):44–51. PMID:
34655224.
31. Florez ID, Amer YS, McCaul M, Lavis JN, Brouwers M. Guidelines developed under pressure. The case of the COVID-19 low-quality “rapid” guidelines and potential solutions. J Clin Epidemiol. 2022; 142:194–199. PMID:
34780983.
32. McPherson SJ, Speed E. NICE rapid guidelines: exploring political influence on guidelines. BMJ Evid Based Med. 2021; bmjebm-2020-111635.
33. Zdravkovic M, Berger-Estilita J, Zdravkovic B, Berger D. Scientific quality of COVID-19 and SARS CoV-2 publications in the highest impact medical journals during the early phase of the pandemic: a case control study. PLoS One. 2020; 15(11):e0241826. PMID:
33152034.
34. Perillat L, Baigrie BS. COVID-19 and the generation of novel scientific knowledge: evidence-based decisions and data sharing. J Eval Clin Pract. 2021; 27(3):708–715. PMID:
33580747.
35. Gaur PS, Zimba O, Agarwal V, Gupta L. Reporting survey based studies - a primer for authors. J Korean Med Sci. 2020; 35(45):e398. PMID:
33230988.
36. Attwell K, Hannah A, Leask J. COVID-19: talk of ‘vaccine hesitancy’ lets governments off the hook. Nature. 2022; 602(7898):574–577. PMID:
35194212.
37. Yurttas B, Poyraz BC, Sut N, Ozdede A, Oztas M, Uğurlu S, et al. Willingness to get the COVID-19 vaccine among patients with rheumatic diseases, healthcare workers and general population in Turkey: a web-based survey. Rheumatol Int. 2021; 41(6):1105–1114. PMID:
33779780.
38. Choi SH, Jo YH, Jo KJ, Park SE. Pediatric and parents’ attitudes towards COVID-19 vaccines and intention to vaccinate for children. J Korean Med Sci. 2021; 36(31):e227. PMID:
34402237.
39. Yessirkepov M, Zimba O, Gasparyan AY. Emerging online tools and platforms for scholarly activities in medicine. Cent Asian J Med Hypotheses Ethics. 2020; 1(2):112–117.
40. Yao H, Zhan C, Sha X. Current situation and distribution equality of public health resource in China. Arch Public Health. 2020; 78(1):86. PMID:
32983449.
41. Chen L, Feng P, Shaver L, Wang Z. Maternal mortality ratio in China from 1990 to 2019: trends, causes and correlations. BMC Public Health. 2021; 21(1):1536. PMID:
34380436.
42. Yin H, Wang S, Zhu Y, Zhang R, Ye X, Wei J, et al. The development of critical care medicine in China: from SARS to COVID-19 pandemic. Crit Care Res Pract. 2020; 2020:3956732. PMID:
32850149.
43. Wang J, Wang Z. Strengths, Weaknesses, Opportunities and Threats (SWOT) analysis of China’s prevention and control strategy for the COVID-19 epidemic. Int J Environ Res Public Health. 2020; 17(7):2235.
44. Kim AM. Psychiatric hospitalization in Korea, 2011-2020: the impact of the Mental Health Act revision of 2017 in consideration of the COVID-19 pandemic. Asian J Psychiatr. 2022; 68:102934. PMID:
34894432.
45. The Lancet. The state of science and society in 2022. Lancet. 2022; 399(10319):1. PMID:
34973708.
46. Bak CK, Krammer JØ, Dadaczynski K, Orkan O, von Seelen J, Prinds C, et al. Digital health literacy and information-seeking behavior among university college students during the COVID-19 pandemic: a cross-sectional study from Denmark. Int J Environ Res Public Health. 2022; 19(6):3676. PMID:
35329363.
47. Zimba O, Radchenko O, Strilchuk L. Social media for research, education and practice in rheumatology. Rheumatol Int. 2020; 40(2):183–190. PMID:
31863133.
48. Zimba O, Gasparyan AY. Social media platforms: a primer for researchers. Reumatologia. 2021; 59(2):68–72. PMID:
33976459.
49. Bode L, Vraga EK. See something, say something: correction of global health misinformation on social media. Health Commun. 2018; 33(9):1131–1140. PMID:
28622038.
50. Madhumathi J, Sinha R, Veeraraghavan B, Walia K. Use of “Social Media”-an option for spreading awareness in infection prevention. Curr Treat Options Infect Dis. 2021; 13(1):14–31. PMID:
33519303.
51. Fleming N. Coronavirus misinformation, and how scientists can help to fight it. Nature. 2020; 583(7814):155–156. PMID:
32601491.
52. Donovan J. Social-media companies must flatten the curve of misinformation. Nature. Forthcoming. 2020; DOI:
10.1038/d41586-020-01107-z.
53. Garrett L. COVID-19: the medium is the message. Lancet. 2020; 395(10228):942–943. PMID:
32171075.
54. Gupta L, Gasparyan AY, Misra DP, Agarwal V, Zimba O, Yessirkepov M. Information and misinformation on COVID-19: a cross-sectional survey study. J Korean Med Sci. 2020; 35(27):e256. PMID:
32657090.
55. Neylan JH, Patel SS, Erickson TB. Strategies to counter disinformation for healthcare practitioners and policymakers. World Med Health Policy. Forthcoming. 2021; DOI:
10.1002/wmh3.487.
56. Bennett S, Glandon D, Rasanathan K. Governing multisectoral action for health in low-income and middle-income countries: unpacking the problem and rising to the challenge. BMJ Glob Health. 2018; 3(Suppl 4):e000880.
57. George A, Jacobs T, Ved R, Jacobs T, Rasanathan K, Zaidi SA. Adolescent health in the Sustainable Development Goal era: are we aligned for multisectoral action? BMJ Glob Health. 2021; 6(3):e004448.
58. Ved R, Sheikh K, George AS, Vr R. Village Health Sanitation and Nutrition Committees: reflections on strengthening community health governance at scale in India. BMJ Glob Health. 2018; 3(Suppl 3):e000681.
59. Ahmadi Livani A, Gohardehi F, Azizi M, Hashemvarzi MR, Taghavi S, Tonekaboni S, et al. Multisectoral actions of mental health during the COVID-19 pandemic in Mazandaran province of Iran. Neuropsychopharmacol Rep. 2022; npr2.12239.
60. Collins T, Akselrod S, Bloomfield A, Gamkrelidze A, Jakab Z, Placella E. Rethinking the COVID-19 pandemic: back to public health. Ann Glob Health. 2020; 86(1):133. PMID:
33102153.
61. Communication, collaboration and cooperation can stop the 2019 coronavirus. Nat Med. 2020; 26(2):151. PMID:
32015560.
62. Imlach F, McKinlay E, Middleton L, Kennedy J, Pledger M, Russell L, et al. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam Pract. 2020; 21(1):269. PMID:
33308161.
63. Perrin PB, Rybarczyk BD, Pierce BS, Jones HA, Shaffer C, Islam L. Rapid telepsychology deployment during the COVID-19 pandemic: a special issue commentary and lessons from primary care psychology training. J Clin Psychol. 2020; 76(6):1173–1185. PMID:
32419164.
64. Shirey MR, Bruck M, Patton E, Bowers D, Watts PI. COVID-19 telehealth fair partnership for capacity building in primary care nursing. Nurs Adm Q. 2022; 46(2):113–124. PMID:
35174796.
65. Yan YY, Fan TY, Zheng YL, Yang HQ, Li TS, Wang HT, et al. Prevention and control of COVID-19 by primary health care facilities in China: a field-survey-based qualitative study in three typical cities. BMC Health Serv Res. 2022; 22(1):399. PMID:
35346179.
66. Rezapour R, Dorosti AA, Farahbakhsh M, Azami-Aghdash S, Iranzad I. The impact of the Covid-19 pandemic on primary health care utilization: an experience from Iran. BMC Health Serv Res. 2022; 22(1):404. PMID:
35346175.
67. Watt T, Sullivan R, Aggarwal A. Primary care and cancer: an analysis of the impact and inequalities of the COVID-19 pandemic on patient pathways. BMJ Open. 2022; 12(3):e059374.
68. Adelekan B, Goldson E, Abubakar Z, Mueller U, Alayande A, Ojogun T, et al. Effect of COVID-19 pandemic on provision of sexual and reproductive health services in primary health facilities in Nigeria: a cross-sectional study. Reprod Health. 2021; 18(1):166. PMID:
34348757.
69. Pérez YM, Gama A, Pedro AR, de Carvalho MJ, Guerreiro AE, Duarte V, et al. The links of stress, substance use and socio-demographic factors with domestic violence during the Covid-19 pandemic in Portugal. J Public Health (Oxf). 2022; fdac024. PMID:
35312006.
70. Rahman R, Huysman C, Ross AM, Boskey ER. Intimate Partner Violence and the COVID-19 Pandemic. Pediatrics. Forthcoming. 2022; DOI:
10.1542/peds.2021-055792.
71. Mohamed AE, Elhadi YA, Mohammed NA, Ekpenyong A, Lucero-Prisno DE. Exploring challenges to COVID-19 vaccination in the Darfur region of Sudan. Am J Trop Med Hyg. 2021; 106(1):17–20. PMID:
34758448.
72. Hashim HT, Miranda AV, Babar MS, Essar MY, Hussain H, Ahmad S, et al. Yemen’s triple emergency: food crisis amid a civil war and COVID-19 pandemic. Public Health Pract (Oxf). 2021; 2:100082. PMID:
34494006.
73. Bizri NA, Alam W, Mobayed T, Tamim H, Makki M, Mushrrafieh U. COVID-19 in conflict region: the Arab levant response. BMC Public Health. 2021; 21(1):1590. PMID:
34445976.
74. Vianna Franco MP, Molnár O, Dorninger C, Laciny A, Treven M, Weger J, et al. Diversity regained: precautionary approaches to COVID-19 as a phenomenon of the total environment. Sci Total Environ. 2022; 825:154029. PMID:
35202694.
75. Nadhamuni S, John O, Kulkarni M, Nanda E, Venkatraman S, Varma D, et al. Driving digital transformation of comprehensive primary health services at scale in India: an enterprise architecture framework. BMJ Glob Health. 2021; 6(Suppl 5):e005242.
76. Booth RG, Allen BN, Bray Jenkyn KM, Li L, Shariff SZ. Youth mental health services utilization rates after a large-scale social media campaign: population-based interrupted time-series analysis. JMIR Ment Health. 2018; 5(2):e27. PMID:
29625954.
77. Lee SH, Pandya RK, Hussain JS, Lau RJ, Chambers EA, Geng A, et al. Perceptions of using infographics for scientific communication on social media for COVID-19 topics: a survey study. J Vis Commun Med. 2022; 45(2):39–47. PMID:
35341427.
78. Jun J, Zhang N, Zain A, Mohammadi E. Social media discussions on the FDA’s modified risk tobacco product authorization of IQOS. Subst Use Misuse. 2022; 57(3):472–480. PMID:
34986075.
79. Tahamtan I, Potnis D, Mohammadi E, Singh V, Miller LE. The mutual influence of the World Health Organization (WHO) and twitter users during COVID-19: network agenda-setting analysis. J Med Internet Res. 2022; 24(4):e34321. PMID:
35275836.
80. Lee S, Nganji JT, Cockburn L. Using twitter to understand the effects of the cameroon anglophone crisis on social determinants of health. Med Confl Surviv. 2021; 37(3):221–247. PMID:
34488511.
81. Bail C. Social-media reform is flying blind. Nature. 2022; 603(7903):766. PMID:
35347297.
82. Ratzan SC, Sommariva S, Rauh L. Enhancing global health communication during a crisis: lessons from the COVID-19 pandemic. Public Health Res Pract. 2020; 30(2):3022010. PMID:
32601655.
83. De Luca F, Laia L, Mehmood A, Vrontis D. Can social media improve stakeholder engagement and communication of Sustainable Development Goals? A cross-country analysis. Technol Forecast Soc Change. 2022; 177:121525.
84. Siau K, Lui R, Mahmood S. The role of a social media editor: what to expect and tips for success. United European Gastroenterol J. 2020; 8(10):1253–1257.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download