This article has been
cited by other articles in ScienceCentral.
Abstract
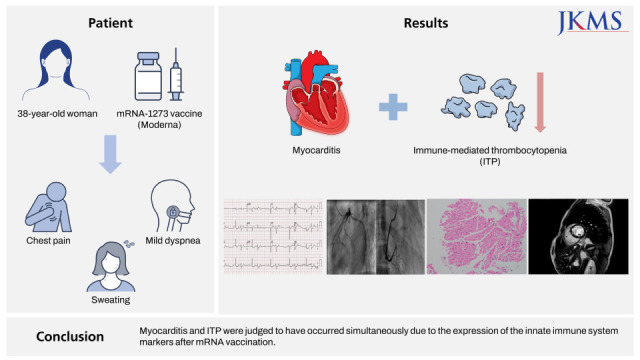
With the global spread of severe acute respiratory syndrome coronavirus 2, several vaccines were developed; messenger RNA (mRNA) vaccines have recently been widely used worldwide. However, the incidence of myocarditis following mRNA vaccination is increasing; although the cause of myocarditis has not yet been clearly identified, it is presumed to be caused by a problem in the innate immune system. Immune-mediated thrombocytopenia (ITP) after vaccination is rare but has been reported and is also assumed to occur by the same mechanism. We report the first case of simultaneous myocarditis and ITP after mRNA vaccination. A 38-year-old woman presented with chest pain, mild dyspnea, and sweating after vaccination with mRNA-1273 vaccine (Moderna) 4 days prior to admission. Upon admission to the emergency department, cardiac enzymes were elevated; blood test performed 5 months ago showed normal platelet count, but severe thrombocytopenia was observed upon admission. After administration of intravenous immunoglobulin, the platelet count improved; subsequently, myocarditis was observed on endomyocardial biopsy. Thus, myocarditis and ITP were judged to have occurred simultaneously due to the expression of the innate immune system markers after mRNA vaccination. The patient was discharged on day 6 of admission.
Keywords: Thrombocytopenia, Myocarditis, COVID-19, Vaccination
INTRODUCTION
Myocarditis and immune-mediated thrombocytopenia (ITP) have rarely been reported after vaccination with the recently developed messenger RNA (mRNA) vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
12 A study reported that the incidence of myocarditis after vaccination with an mRNA vaccine is increasing, especially in young men. Fortunately, in most cases, it presents with mild symptoms and improves with supportive care.
3 However, since it can lead to sudden cardiac death, its prompt diagnosis is crucial in preventing adverse outcomes.
4 Previously, an increase in the incidence of thrombocytopenia after adult vaccination had not been reported; however, new reports show that SARS-CoV-2 vaccines increase the incidence of vaccine-induced thrombosis with thrombocytopenia and ITP.
CASE DESCRIPTION
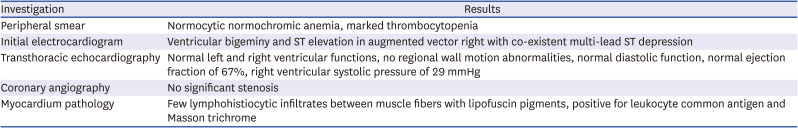
A 38-year-old woman without underlying disease was admitted to the emergency department because of chest pain, mild dyspnea, and sweating. The first dose of mRNA-1273 vaccine (Moderna, Cambridge, MA, USA) was administered 4 days before symptom onset. Electrocardiography showed ventricular bigeminy and ST elevation in augmented vector right with co-existent multi-lead ST depression (
Fig. 1A). Creatinine kinase-MB (CK-MB) was initially normal; however, troponin T was elevated. CK-MB and troponin T levels continued to rise till the following morning after symptom onset. On echocardiography, cardiac function was normal, and regional wall motion abnormalities and myocardial edema were not observed. Moreover, laboratory tests showed that the platelet level was reduced from 283 × 10
9 cells/L measured 5 months ago to 9 × 10
9 cells/L at the time of admission. However, no ecchymosis, purpura, or spontaneous bleeding due to thrombocytopenia was noted.
Fig. 1
Electrocardiogram and coronary angiography of the patient at admission. (A) Initial electrocardiogram, (B) Left coronary artery, (C) Right coronary artery.
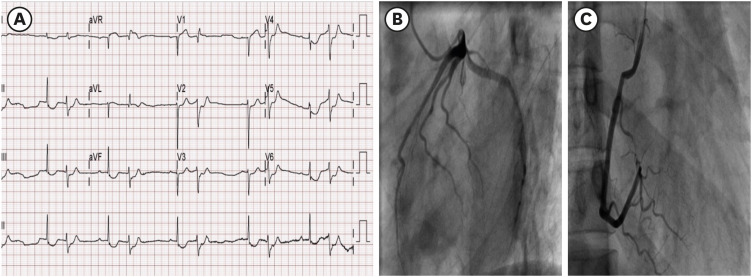
Coronary angiography was performed because of elevated cardiac enzymes and abnormal electrocardiogram findings. No coronary artery stenosis was observed on angiography (
Fig. 1B & 1C), and cardiac enzymes started to show a gradual downward trend 1 day after admission. However, the platelet count did not improve even after 3 days of follow-up. Therefore, on the third day of admission, intravenous immunoglobulin (IVIG) was administered at 400 mg/kg/day for a total of 5 days. The platelet count measured after the first day of IVIG administration showed an upward trend; however, IVIG was stopped after only 2 days because the patient complained of severe headache during IVIG administration. Endomyocardial biopsy was not performed initially because of thrombocytopenia. After IVIG administration, biopsy was performed on day 5 of hospitalization when the platelet count had increased to 50 × 10
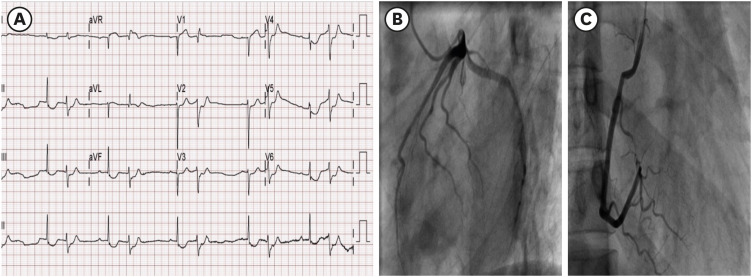
9 cells/L. As for the pathological findings of myocardial tissue, internal nuclei and vacuolated muscle fibers were observed, and lymphohistiocytic infiltrates between muscle fibers were observed (
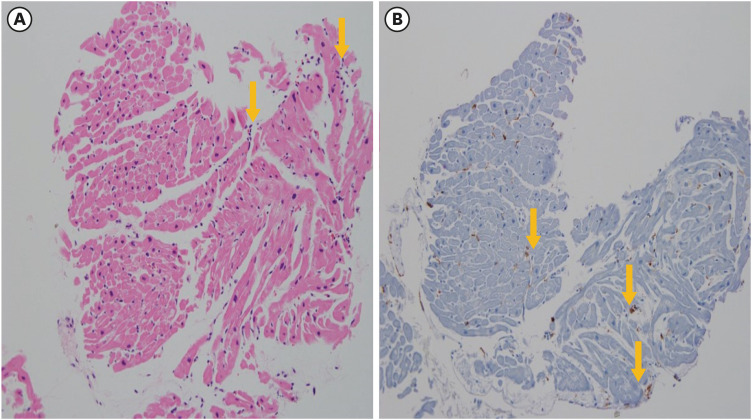
Fig. 2). These findings showed myocarditis in the stage of recovery. Cardiac magnetic resonance (CMR) was performed to confirm the diagnosis and assess the degree of myocardial damage. In CMR, multifocal patchy delayed enhancement at mid of anterior-inferoseptal wall of left ventricle (LV) and subendocardial wall of anterior-inferoseptal wall of LV basal to mid wall was observed. Also, in the T2 image of CMR, high signal intensity at anterior-inferoseptal wall of LV basal to mid wall was observed (
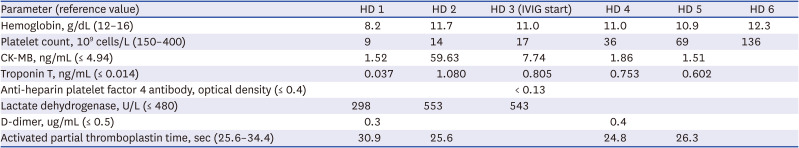
Fig. 3). These findings were judged to be those found in myocarditis. The patient was discharged on day 6 of admission. Results of anti-heparin platelet factor 4 antibody test performed during hospitalization were negative. Results of investigations are presented in
Tables 1 and
2. Considering the patient’s history and clinical course, we concluded that myocarditis and ITP seemed to have occurred simultaneously after mRNA-1273 vaccination.
Fig. 2
Histopathology of the heart of interventricular septum. (A) Hematoxylin and eosin stains show a small amount of lymphohistiocytic infiltration between muscle fibers. (B) Leukocyte common antigen immunohistochemistry stain shows interstitial lymphocyte infiltration.
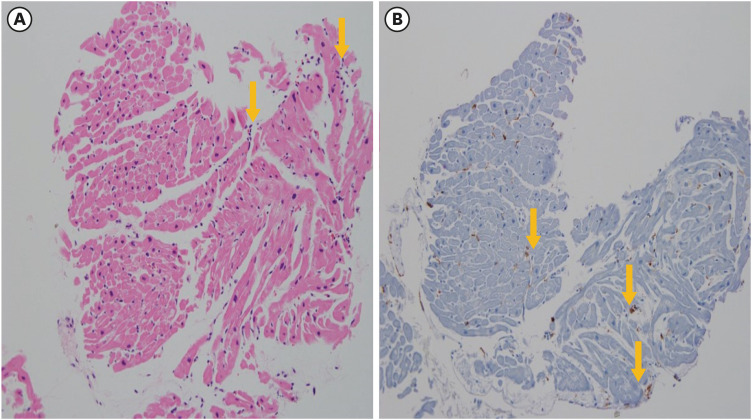
Fig. 3
Cardiac magnetic resonance imaging of myocarditis. (A) T2 imaging shows high signal intensity on mid of anterior-inferoseptal segment. (B) Image with late gadolinium enhancement.
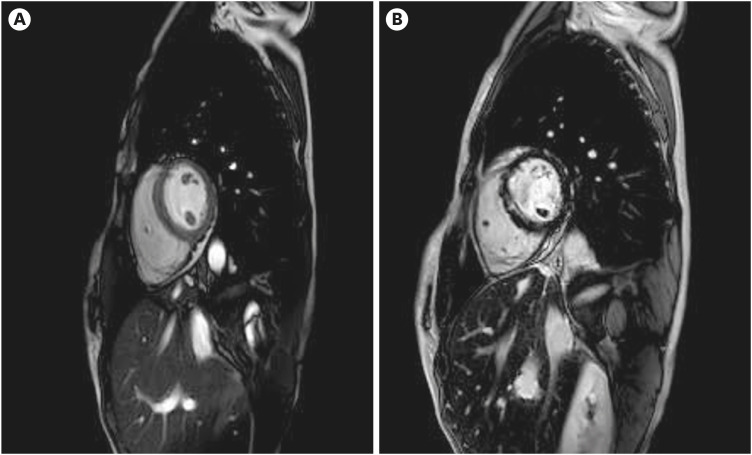
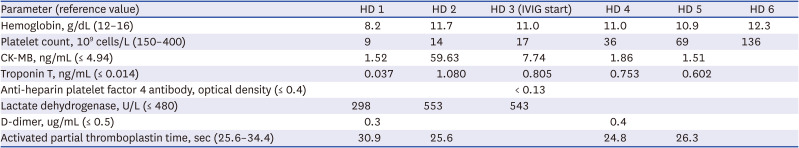
Table 1
Laboratory and imaging findings
|
Parameter (reference value) |
HD 1 |
HD 2 |
HD 3 (IVIG start) |
HD 4 |
HD 5 |
HD 6 |
|
Hemoglobin, g/dL (12–16) |
8.2 |
11.7 |
11.0 |
11.0 |
10.9 |
12.3 |
|
Platelet count, 109 cells/L (150–400) |
9 |
14 |
17 |
36 |
69 |
136 |
|
CK-MB, ng/mL (≤ 4.94) |
1.52 |
59.63 |
7.74 |
1.86 |
1.51 |
|
|
Troponin T, ng/mL (≤ 0.014) |
0.037 |
1.080 |
0.805 |
0.753 |
0.602 |
|
|
Anti-heparin platelet factor 4 antibody, optical density (≤ 0.4) |
|
|
< 0.13 |
|
|
|
|
Lactate dehydrogenase, U/L (≤ 480) |
298 |
553 |
543 |
|
|
|
|
D-dimer, ug/mL (≤ 0.5) |
0.3 |
|
|
0.4 |
|
|
|
Activated partial thromboplastin time, sec (25.6–34.4) |
30.9 |
25.6 |
|
24.8 |
26.3 |
|
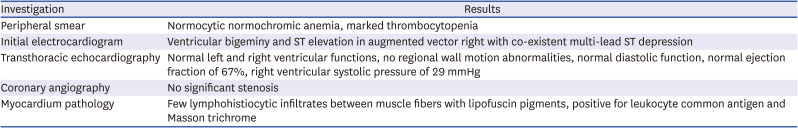
Table 2
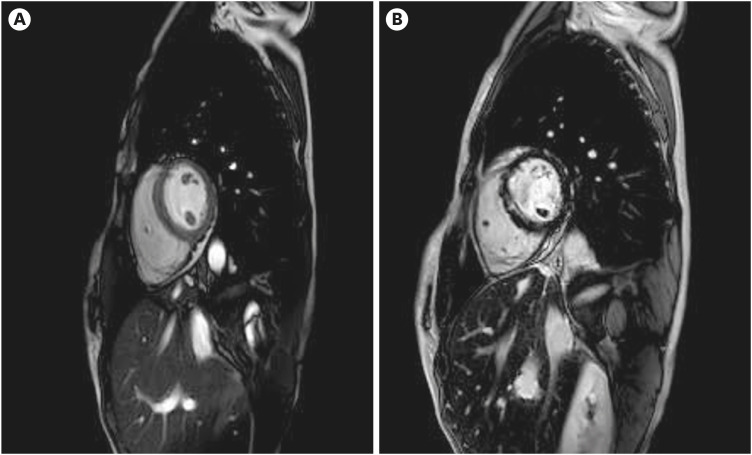
Histopathologic findings
|
Investigation |
Results |
|
Peripheral smear |
Normocytic normochromic anemia, marked thrombocytopenia |
|
Initial electrocardiogram |
Ventricular bigeminy and ST elevation in augmented vector right with co-existent multi-lead ST depression |
|
Transthoracic echocardiography |
Normal left and right ventricular functions, no regional wall motion abnormalities, normal diastolic function, normal ejection fraction of 67%, right ventricular systolic pressure of 29 mmHg |
|
Coronary angiography |
No significant stenosis |
|
Myocardium pathology |
Few lymphohistiocytic infiltrates between muscle fibers with lipofuscin pigments, positive for leukocyte common antigen and Masson trichrome |
Ethnics statement
This case was approved by the Institutional Review Board (IRB) of Chungbuk National University Hospital (IRB No. 2021-11-003), and the IRB waived informed consent for this reporting.
DISCUSSION
Myocarditis is an inflammatory disease of the heart that is caused by infection, exposure to toxic substances, and abnormal activation of the immune system, including autoimmune diseases.
5 Vaccine-related myocarditis has recently been emerging, according to Centers for Disease Control and Prevention (CDC) working case definition, and a confirmed case of acute myocarditis after vaccination is defined as the occurrence of one or more new or worsening symptoms, histologically confirmed myocarditis, or elevated troponin above the upper limit of normal and cardiac magnetic resonance imaging (MRI) findings consistent with myocarditis.
6 In Korea, the same definition is used to make a definitive diagnosis of myocarditis.
7 In addition, ITP is currently judged to be caused by autoimmune diseases.
8 Although the exact mechanism is not known yet, it is currently believed that the cause of vaccine-related myocarditis is an abnormal immune system response.
9
To the best of our knowledge, this is the first case of simultaneous occurrence of myocarditis and ITP after mRNA-1273 COVID-19 vaccination. According to the CDC working case definition for myocarditis, the symptoms, elevated cardiac enzymes, and histopathologic and cardiac MRI findings of our patient all satisfied the criteria for myocarditis.
6 She had a normal platelet count 5 months ago, her anti-heparin platelet factor 4 antibody test was negative, and her platelet count improved immediately after IVIG administration. Therefore, the patient was diagnosed with ITP. She developed symptoms 4 days after vaccination; hence the myocarditis and ITP were considered to be possibly related to mRNA-1273 COVID-19 vaccination.
These symptoms have been reported to occur more frequently after the second dose of mRNA COVID-19 vaccination; however in this case, symptoms occurred after the first dose. Therefore, if bruising, purpura, chest pain, or chest tightness occurs after vaccination, blood tests and electrocardiogram should be performed to diagnose myocarditis and ITP even after the first dose of COVID-19 vaccination.
ACKNOWLEDGMENTS
The authors would like to thank the patients who were well treated and recovered.
References
1. Rosner CM, Genovese L, Tehrani BN, Atkins M, Bakhshi H, Chaudhri S, et al. Myocarditis temporally associated with COVID-19 vaccination. Circulation. 2021; 144(6):502–505. PMID:
34133885.
2. Lee EJ, Cines DB, Gernsheimer T, Kessler C, Michel M, Tarantino MD, et al. Thrombocytopenia following Pfizer and Moderna SARS-CoV-2 vaccination. Am J Hematol. 2021; 96(5):534–537. PMID:
33606296.
3. Witberg G, Barda N, Hoss S, Richter I, Wiessman M, Aviv Y, et al. Myocarditis after COVID-19 vaccination in a large health care organization. N Engl J Med. 2021; 385(23):2132–2139. PMID:
34614329.
4. Choi S, Lee S, Seo JW, Kim MJ, Jeon YH, Park JH, et al. Myocarditis-induced sudden death after BNT162b2 mRNA COVID-19 vaccination in Korea: case report focusing on histopathological findings. J Korean Med Sci. 2021; 36(40):e286. PMID:
34664804.
5. Tschöpe C, Ammirati E, Bozkurt B, Caforio AL, Cooper LT, Felix SB, et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol. 2021; 18(3):169–193. PMID:
33046850.
6. Bozkurt B, Kamat I, Hotez PJ. Myocarditis with COVID-19 mRNA vaccines. Circulation. 2021; 144(6):471–484. PMID:
34281357.
7. Korea Disease Control and Prevention Agency. Press Reference: Current Status of COVID-19 Outbreak and Vaccination in South Korea (9.26). Cheongju: Korea Disease Control and Prevention Agency;2021.
8. Liu Y, Chen S, Sun Y, Lin Q, Liao X, Zhang J, et al. Clinical characteristics of immune thrombocytopenia associated with autoimmune disease: a retrospective study. Medicine (Baltimore). 2016; 95(50):e5565. PMID:
27977588.
9. Heymans S, Cooper LT. Myocarditis after COVID-19 mRNA vaccination: clinical observations and potential mechanisms. Nat Rev Cardiol. 2022; 19(2):75–77. PMID:
34887571.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download