INTRODUCTION
As the survival of preterm infants has increased, the focus of neonatal care has shifted to the importance of growth.
1234 For the catch-up growth of very low birth weight (VLBW) infants, regular comprehensive checkups to monitor growth and provide early intervention to achieve normal growth are essential.
5 Developed countries such as Canada, the United States, Australia, and Japan have conducted high-risk follow-up clinics to improve neonatal outcomes and accumulate long-term growth and development.
67
In Korea, the Korean Neonatal Network (KNN) was launched in 2013 and has collected clinical data on neonatal intensive care unit (NICU) admission and follow-up data at 18–24 and 36 months of age prospectively from 76 NICUs across Korea. Over 70% of VLBW infants born in Korea were registered in the KNN during NICU admission
8; however, the follow-up rate was noted to be approximately 68% at 18–24 months of age and 45% at 36 months of age, showing lower rates in the national data and limiting the data after 3 years of age.
9
The NHIS database includes overall healthcare claims data of the people in Korea, such as the diagnosis, status of outpatients and inpatients, drugs, and laboratory and imaging tests.
10 In addition, the data of national infants’ health screening program were collected in the NHIS database, showing the nationwide infants’ health data linking to the healthcare claims data.
1112 However, there is a remaining issue of bias, such as diagnosis, selection, and accuracy based on the claims data. No detailed clinical data and demographic data resulted in the limitation of the national epidemiology; the follow-up rate in the NHIS of VLBW infants is low, and the use of corrected age rather than chronological age leads to the confusion of real growth and development.
There have been some reports of long-term growth and development of VLBW infants in Korea.
131415
However, a variety of follow-up parameters and tracking time points lead to decreased credibility of the accumulated data. The need to link the KNN and NHIS data is increasing to accumulate more qualified data to lay the groundwork for the efficacy of systemic national population-based data.
We aimed to estimate the nationwide growth outcomes from birth to 5 years in infants born under 1,500 g by integrating the KNN and NHIS databases indirectly from previous studies and to analyze the effects of major morbidities in preterm infants on growth.
Go to :

METHODS
We initially identified the overall follow-up rate based on the birth statistics data of Korea.
An infant born with a birth weight below the 1,500 g was referred to as VLBW, and below 1,000 g was referred to as extremely low birth weight (ELBW). Based on the birth statistics, the total number of VLBW births between 2013–2015 was 8,860. The KNN database included VLBW infants who were born in the KNN-affiliated hospitals or VLBW infants who were transferred to a KNN-affiliated hospital before the 28 days of life. After excluding VLBW infants who died before admission to the NICU, a total of 6,086 VLBW infants were registered in KNN registry between 2013–2015, which shows that the KNN covered 69% of the national VLBW births based on the birth statistics data.
Conversely, the number of VLBW infants who participated in the NHIS health screening program was 5,800, reflecting 65% coverage based on the birth statistics data.
The direct linkage of patient level between the KNN and NHIS databases is impossible because of the regulation of data safety and privacy, and we compared only the number of infants between the two studies. The growth data of the KNN data was adopted form the published article, “Growth failure of very low birth weight infants during the first 3 years: A Korean Neonatal Network.”
16 The NHIS data was adopted partially from the published article, “The impact of neonatal morbidities on child growth and developmental outcomes in very low birth weight infants: A nationwide cohort study” and expanded the population year to 2014 and 2015.
17 After integrating the two extensive pools of data, we serially compared the composite outcome of growth failure and major morbidity in VLBW infants between the NHIS and KNN databases. From 2013 to 2015, 5,650 VLBW infants were discharged alive and registered in the KNN database. Among them, 188 infants with severe malformation or chromosome anomalies, 38 infants who died within 18–24 months of age, 63 infants with inadequate body profile information, such as without body weights, and 2,418 infants who were lost to follow-up were excluded. Afterward, we used data from 2,943 VLBW infants for growth and morbidity.
The number of VLBW infants born between 2013 and 2015 who underwent a national infant health check-up was 5,800. These data were included to compare growth and morbidities in the NHIS data.
In the KNN database, growth failure is defined as birth weight of z-score below −1.28 (10th percentile) using the Fenton and World Health Organization growth charts. According to the KNN manual of operation, bronchopulmonary dysplasia (BPD) was defined as the use of supplemental oxygen or respiratory support at 36 weeks of post-menstrual age, corresponding to moderate to severe BPD using the severity-based definition for BPD of the National Institutes of Health consensus. Periventricular leukomalacia (PVL) was defined on the basis of either head ultrasonography or cranial magnetic resonance imaging confirmed by a radiologist. In the NHIS database, growth failure is defined as the weight below the 10th percentile using the growth chart of the Korean infant. BPD and PVL were identified using the International Classification of Diseases (ICD)-10 codes inputted by hospital, which were diagnosed by the clinical judgment of the neonatologists according to generally known definitions.
BPD were sorted by ICD-10 code P27.1, PVL was sorted by ICD-10 code G93.88.
The time of visit in the follow-up program of the KNN scheduled follow-up 1 at 18–24 months of corrected age and follow-up 2 scheduled at 33–39 months of chronological age by a neonatologist working at a KNN-affiliated hospital. The National Health Screening Program schedules their first visits at 4–6 months of age, second visits at 9–12 months, third visits at 18–24 months, fourth visits at 30–36 months, fifth visits at 42–48 months, and sixth visits at 54–60 months.
18 All check-ups were based on the chronological age, not the corrected age. Health screening programs include medical history, physical examination, anthropometric measurements, screening for visual acuity, developmental screening by the Korean Developmental Screening Test (K-DST), oral examination, and questionnaires with anticipatory guidance. To compare two group longitudinally, we converted KNN data into chronological age to compare the growth percentile at the same time period of NHIS check-up. KNN data has birth date, gestational age and follow up date, so we could calculate the chronological age at follow up visit.
Statistical Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences version 21 (IBM Corp., Chicago, IL, USA). The χ2 test was performed for non-continuous data, and Student’s t-test was performed for continuous data. The level of statistical significance was set at P < 0.05.
Ethics statement
The KNN registry was approved by the Samsung Medical Center Institutional Review Board (2013-03-002) and the Institutional Review Boards of all 70 hospitals participating in the KNN. Written consent was obtained from the parents of the infants during enrollment in the KNN. In the NHIS data, all identifiable variables, including claim-, individual-, and organizational-level identification numbers, were re-generated randomly in the NHIS database to protect the patients’ privacy. This study used the NHIS data (NHIS-2019-1-569) maintained by the NHIS. The study protocol was approved by the Institutional Review Board of Gangnam Severance Hospital (No. 3-2019-0147). The requirement for informed consent was waived.
Go to :

RESULTS
The demographics of the study are presented in
Table 1. The follow-up percentage is calculated on the basis of the annual birth statistics data based on the birth certificate.
Table 1
Number of infants and the rate (%) of follow up based on birth statistics by the Korean Neonatal Network and National Health Insurance Service databases

|
Year |
Birtha
|
Dischargea
|
6 monb
|
12 monb
|
CA 18–24 mona
|
24 monb
|
33–39 mona
|
36 monb
|
48 monb
|
60 monb
|
Birth statistics |
|
2013 |
1,469 |
1,147 |
632 |
766 |
846 |
1,026 |
624 |
1,272 |
1,208 |
1,154 |
2,961 |
|
2014 |
2,160 |
1,598 |
642 |
762 |
1,182 |
1,031 |
839 |
1,238 |
1,245 |
1,136 |
2,871 |
|
2015 |
2,457 |
1,902 |
782 |
987 |
1,400 |
1,254 |
1,109 |
1,520 |
1,480 |
1,152 |
3,032 |
|
Total |
6,086 |
4,647 |
2,056 |
2,515 |
3,428 |
3,311 |
2,572 |
4,030 |
3,933 |
3,442 |
8,864 |
|
Rate (%) |
69 |
52 |
23 |
28 |
39 |
37 |
29 |
45 |
44 |
39 |
100 |

Among 8,864 VLBW infants from the Statistics Korea using birth certificate,
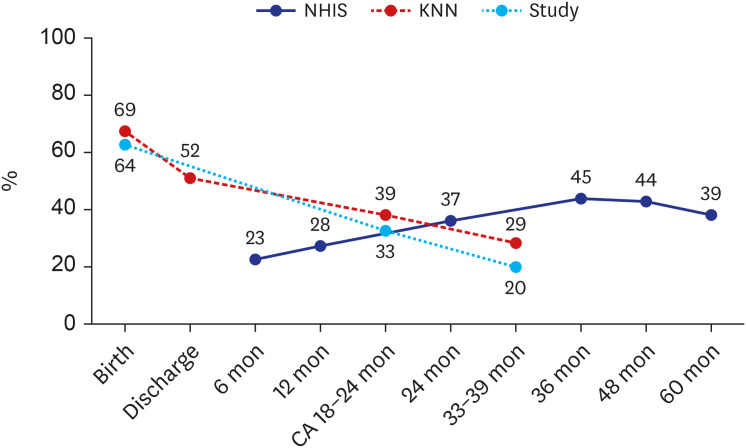
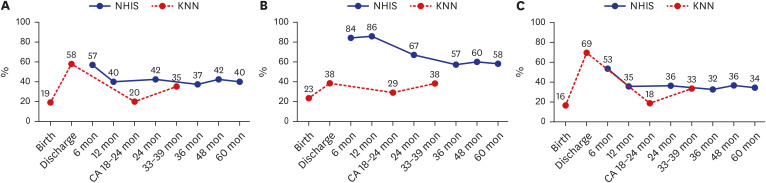
19 6,086 infants (69%) at birth were enrolled in the KNN database. Among 6,068 infants, 3,428 infants (56%) were enrolled at a corrected age of 18–24 months and 2,572 infants (42%) were enrolled at a chronological age of 33–39 months according to the KNN follow-up registry. However, based on the national birth statistics data, the overall follow-up rate of the KNN at 36 months of age was as low as 29%.
Conversely, among 8,864 VLBW infants registered using the birth certificate, 5,800 VLBW infants (65%) underwent the NHIS check-up. The NHIS screening was done in 2,515 infants (28%) at 12 months. At 24 months, 3,311 infants (37%) were followed up, and at 36 months, 4,030 (45%) infants were followed up. The NHIS screening rate was the lowest at first marking 23%; however, it increased by nearly 45% at 36 months, exceeding the KNN follow-up rate.
Fig. 1 shows that the follow-up rate of VLBW infants is different between the KNN and NHIS groups.
 | Fig. 1
Follow up rate (%) of the KNN and NHIS data. The number of very low birth weight infants at birth and discharge is based on the KNN registry.
KNN = Korean Neonatal Network, NHIS = National Health Insurance Service.

|
Dotted line in
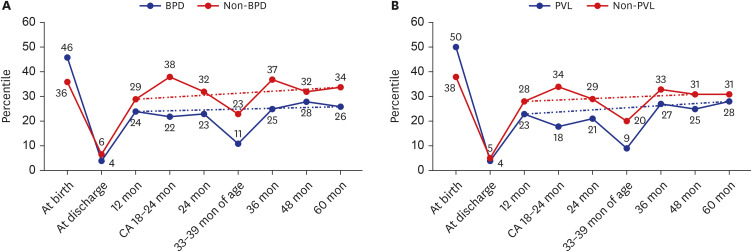
Fig. 1 represents the data of 2,943 VLBW infants enrolled in previous study using KNN database. The prevalence of growth failure is shown in
Fig. 2. Growth failure at corrected age of 18–24 months and 36 months are more common in the NHIS than in the KNN (42% vs 20%
P < 0.001 37% vs 34.5%
P = 0.578), as shown in
Fig. 2A. Among subgroups, there is a difference in the frequency of the growth retardation group between the KNN and NHIS groups in the ELBW group compared to the 1,000–1,500 g group, as shown in
Fig. 2B and C. Infants weighing 1000–1500 g showed difference at 18–24months (
P < 0.001), but at the time of 36 months of corrected age difference decreased (
P = 0.548). However, the ELBW group showed consistent differences in the prevalence of growth failure at 18–24 months (
P = 0.002) to 33-39 months after birth (
P < 0.001).
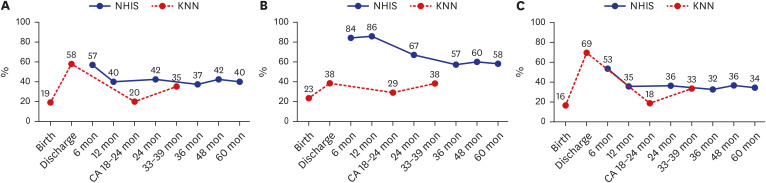 | Fig. 2
Comparison of incidence of growth failure between the KNN and NHIS data. (A) Comparisons made in very low birth weight, (B) in extremely low birth weight, (C) and in the infants with birth weight 1,000–1,500 g.
Growth failure at birth and discharge is defined as the weight below 10th percentiles according to the KNN registry.
KNN = Korean Neonatal Network, NHIS = National Health Insurance Service.

|
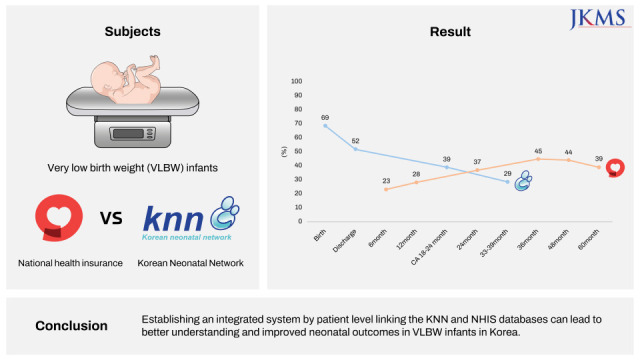
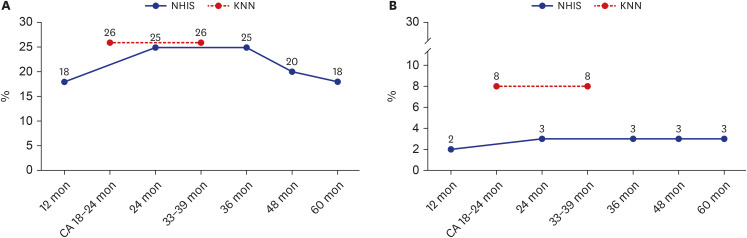
Looking at the prevalence of major morbidities in VLBW infants, the prevalence of BPD is similar between the KNN and NHIS (
P = 0.432), whereas PVL showed a large difference (
P < 0.001) in prevalence between the NHIS and KNN groups, as shown in
Fig. 3.
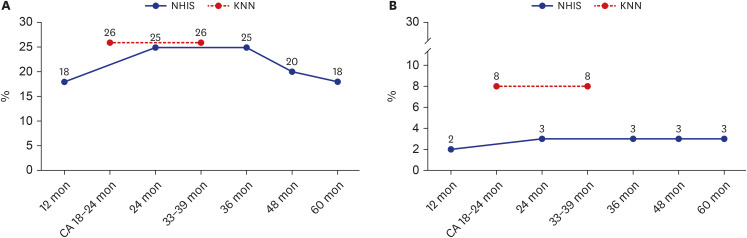 | Fig. 3
Comparison of incidence of BPD and PVL between the KNN and NHIS data. (A) BPD and (B) PVL.
BPD = bronchopulmonary dysplasia, PVL = periventricular leukomalacia, KNN = Korean Neonatal Network, NHIS = National Health Insurance Service.

|
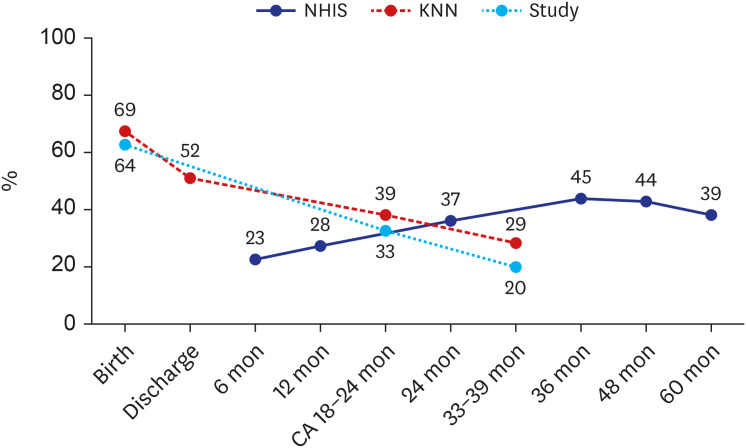
By sequentially integrating data from the NHIS and KNN, we compared long-term growth in two groups with BPD and PVL two major diseases in preterm infants, as shown in
Fig. 4. VLBW infants with BPD and PVL tended to have difficulties in achieving normal catch-up growth in both groups. Although the KNN and NHIS were tracked at the same time, it can be confirmed through the pattern of the graph that the weight percentiles were different. KNN's follow-up at corrected age of 18–24 months and the NHIS follow-up at 24 months are at the same time point, but the weight percentile varies ranging 8-16% of difference at 2 years (BPD:
P = 0.002, PVL:
P = 0.023) and 13-18% difference at 3 years between the KNN and NHIS (BPD:
P < 0.001 PVL:
P < 0.001). Dotted line in
Fig. 4 is a mean line that represents the pattern of optimal growth percentile that can be estimated by integrated database.
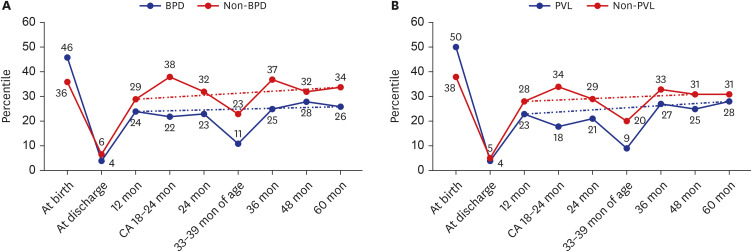 | Fig. 4
Comparison of growth patterns and morbidities between the KNN and NHIS data. (A) Weight percentile of infants with BPD and (B) weight percentile of infants with PVL.
KNN = Korean Neonatal Network, NHIS = National Health Insurance Service, BPD = bronchopulmonary dysplasia, PVL = periventricular leukomalacia.

|
Go to :

DISCUSSION
Currently in Korea, regarding preterm infant data on the birth statistics, the KNN and NHIS have been considered as a national population-based databases; however, the KNN and NHIS databases have different strengths and weaknesses. This study is the first to report the differences in growth outcomes between the KNN database and NHIS database.
The total birth rate is decreasing, estimating a 2.7 million infants in 2020 compared to 10% reduction in 2019, but preterm birth is markedly increasing every year, with such cases occurring in 8.5% of neonates in 2020.
20 Preterm infants, especially VLBW infants, had a high risk for growth and developmental delay or disabilities.
21 In addition, expense of medical use and admission duration was higher in VLBW infants.
22 Close monitoring and early intervention are necessary for VLBW infants. However, information on preterm infants is currently scattered; thus, it is difficult to understand longitudinally and determine the current status of the national data. This lack of data makes it difficult to establish public policies that can help preterm infants to grow. Furthermore, the national statistical management of preterm infants is urgently needed to provide a basis for policy making.
The KNN is a nationwide database, in which detailed data of VLBW infants from birth to 3 years of age are scheduled and collected by trained neonatologists using a standardized manual of operating procedures to minimize differences between sites.
8 However, long-term data after 3 years cannot be collected. The NHIS data is a large-scale, extensive, and stable data based on the nationwide health insurance data generated by the government or public institutions’ involvement.
15 The birth statistics, including mortality, cause of death and national infants’ health checkup data were linked in the NHIS data, which was a representative of the national population-based data. However, it does not include maternal and perinatal factors, nutrition, or complications of prematurity. In addition, non-insurance benefits data or participants’ specific medical treatment, such as physical therapies or occupational therapy performed at private clinics, were not included. In addition, the age at check-up in the National Infant Health Screening Program is mixed based on postnatal age and corrected age depending on the performing physician; thus, causing confusion and misunderstanding of preterm health.
Most preterm infants tend to achieve catch-up growth within the first 2 years of life
23; however, many studies have reported that catch-up growth can continue after infancy, even into adolescence.
24
Poor growth is related to poor neurodevelopmental outcomes; hence, the importance of comprehensive follow-up of VLBW infants is important to improve various long-term outcomes.
2526 However, in Korea, low rates of follow-up and limitation of detailed outcomes remain challenging issues. By indirectly integrating the sporadic clinical data of VLBW obtained in the NHIS and KNN, we identified disparities in the follow-up rate and incidence of morbidities of VLBW infants. We suggest that linking two databases at the patient level can be helpful to understand the longitudinal outcome of VLBW infants and provide proper intervention.
The rate of enrollment in the KNN during NICU admission is high but decreases every subsequent visit. However, the NHIS follow-up rate was low at 6 months, but increased to over 40% at 3–4 years of age. This finding shows that VLBW patients tend to visit tertiary hospitals rather than local clinics immediately after discharge. However, as the baby gets older and parental anxiety decreases, tertiary hospital visits decrease, and visits to local clinics increase due to easy access and convenience. Linking the KNN and NHIS databases at the patient level can be helpful in reducing the follow-up loss and increasing the accessibility to the follow-up clinic, consequently contributing to the improvement of the long-term outcomes of VLBW infants.
The prevalence of growth failure also differed between the two groups. In the KNN database, 58% of VLBW are below 10th percentiles at the time of discharge, 20% at a corrected age of 18–24 months and 35% at a chronological age of 33–39 months. In contrast, in the NHIS database, growth failure is consistently approximately 40%. For subgroup analysis dividing ELBW and birth weight 1,000–1,500 g, we found that the ELBW group showed more discrepancies between the KNN and NHIS. Rate of growth failure at discharge is higher in 1,000–1,500 g than ELBW group. Weight at discharge depends on admission period, which implies that ELBW stays at NICU longer for more specialized treatment and support until stabilization of infant than 1,000–1,500 g group. In ELBW group, rate of growth failure of NHIS is higher at the time of 24 months (P = 0.002) and at the time of 36 months (P < 0.001). NHIS program is based on postnatal age rather than corrected age, so rate of growth failure of ELBW can be biased in NHIS program depending on performing physician. Also, this implies that the follow-up rate in the KNN is higher in the ELBW group than in the 1,000–1,500 g group. It can be estimated that ELBW infants have a lower follow-up rate for infant screening conducted in the NHIS and participate more in the KNN prematurity follow-up program due to more morbidities and require a comprehensive approach to neonatology. In 1,000–1,500g group, rate of growth failure is lower in KNN at the time of 18–24 months (P < 0.001), however shows statistically no significant difference in 36months. This implies that among VLBW infants, 1,000–1,500 g group which represents bigger birth weight achieve catch up growth before 36months and participate NHIS as well as KNN, compared to ELBW group. KNN recommended that follow-up until 3 years of age and linking the NHIS database after 3 years of age to 6 years of age can be useful for careful monitoring and regular assessment.
According to the KNN annual report, among VLBW infants born in 2013–2015, BPD prevalence is 26.7%. By subgroup, BPD occurred in 40.9% of ELBW, 17.8% of 1,000–1,500 g group. PVL prevalence is 8.1% in VLBW. By subgroup, PVL occurred in 10.3% of ELBW, 6.8% of 1,000–1,500 g.
9 Prevalence of BPD in NHIS database is 18–25% according to age, prevalence of PVL in NHIS 2–3% as described in
Fig. 3. Reported global incidence range of BPD is 10–89%, PVL is 3–15% which is consistent with our study.
27282930
The prevalence of BPD rate was similar between the NHIS and KNN, which means that ICD-10 codes were well inputted by the hospitals due to monthly synagis (Palivizumab) vaccination insurance coverage criteria. Conversely, PVL diagnosis showed disparities between the two groups. This may imply a low follow-up rate in the NHIS program in PVL patients due to various comorbidities or a general condition, suggesting a tendency to prefer examinations at the tertiary hospitals according to disease prevalence. This implies that the omission of ICD-10 codes by primary physicians performing the NHIS program is higher, and information on rare diseases may not be sufficient in the NHIS data. Physicians should be aware of the various diagnoses when following preterm infants to accumulate qualified data.
By integrating the KNN and NHIS data at continuous time points according to morbidities, the serial weight percentile after discharge was lower in VLBW infants with BPD or PVL than in those without diagnosis. At the same time point, the KNN and NHIS showed different trends in the weight percentile. If it is continuous data, it should show a smooth pattern, such as a dotted line. There is a limit in the continuous data collection because the total number of target groups at each time point is different, and this leads to data discrepancy.
The major limitation of this study is that we compared two groups indirectly, not with patient-level linking, but by matching the result by group. The data collection time points were somewhat different. Furthermore, detailed information about nutrition, socioeconomic status, familial information, and treatment was not considered in the analysis. The weight was based on the questionnaire of the national health screening program for infants and children, and missing data or selection issues may potentially influence our findings. Finally, the diagnosis of several morbidities was identified according to ICD-10 codes in the NHIS claims database without reviewing the detailed clinical charts including degree or severity. Misclassification or omission may have affected our findings.
As the KNN and NHIS data have their own strengths and weaknesses, linking the KNN and NHIS can lead to improved data accumulation systems by adding some additional information for researchers and policy makers. Correlating the data and providing a platform can help establish supporting policies and perform advanced research. Integrating the big data of the two groups can lay the groundwork for establishing population-based national data that can eventually improve the outcome of high-risk infants and VLBW infants.
In conclusion, by integrating the KNN and NHIS data indirectly at continuous time points according to morbidities, we confirmed the discontinuity and discrepancy between the two databases among VLBW infants.
Establishing an integrated system by patient level linking the KNN and NHIS databases can lead to better understanding and improved neonatal outcomes in VLBW infants in Korea.
Go to :






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download