This article has been
cited by other articles in ScienceCentral.
Abstract
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 that may trigger Guillain-Barre syndrome (GBS) in selected patients. We describe a case of GBS presenting as marked finger extensor weakness in a 73-year-old woman with COVID-19. Her clinical and electrophysiological findings were consistent with a diagnosis of acute motor axonal neuropathy subtype of GBS with prominent finger dropping. Treatment with intravenous immunoglobulin for 5 days completely resolved her finger extension weakness after 19 months, although other involved extremities recovered earlier at 3 months. This study highlights that COVID-19-associated GBS can present in various forms aside from the classic variant, even in patients without any COVID-19 symptoms. Therefore, it is important to always consider the diagnosis of GBS in patients with COVID-19.
Go to :

Graphical Abstract
Go to :

Keywords: Guillain-Barre Syndrome, COVID-19, SARS-CoV-2, Finger Drop
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that remains prevalent to date. Here, we report a case of Guillain-Barre syndrome (GBS) presenting as marked finger extensor weakness in a patient with COVID-19. To the best of our knowledge, this is the first report to describe finger drop-dominant GBS in patients with COVID-19.
Go to :

CASE DESCRIPTION
A 73-year-old woman presented to Keimyung University Dongsan Hospital on April 14, 2020 for generalized weakness of the extremities, more pronounced on the fingers, 2 weeks after exposure to a person with confirmed COVID-19. There was no recent history of diarrhea or respiratory illness. She had no fever or respiratory symptoms. However, real-time reverse transcription-polymerase chain reaction (RT-PCR) using a nasopharyngeal swab was positive for SARS-CoV-2 at the onset of weakness. Neurologic examination revealed severe bilateral asymmetric weakness on finger extension (Medical Research Council [MRC] grades 2 and 3 on the right and left, respectively) with relatively intact finger flexion, wrist extension, and wrist flexion (MRC grade 4) (
Fig. 1A). All remaining upper and lower limb muscles showed mild weakness (MRC grade 4). Deep tendon reflexes were decreased in all extremities. There was no cranial nerve involvement, sensory abnormalities, or ataxia.
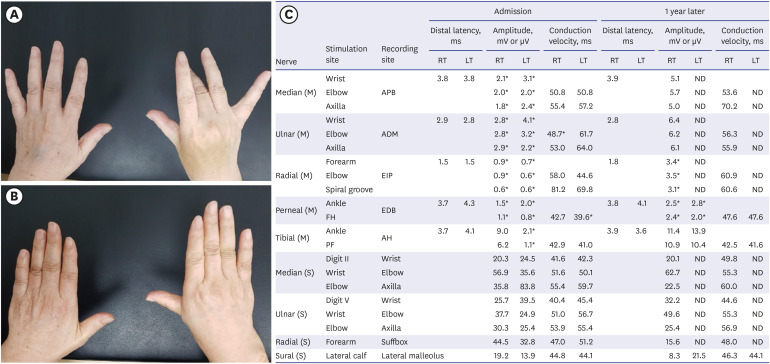
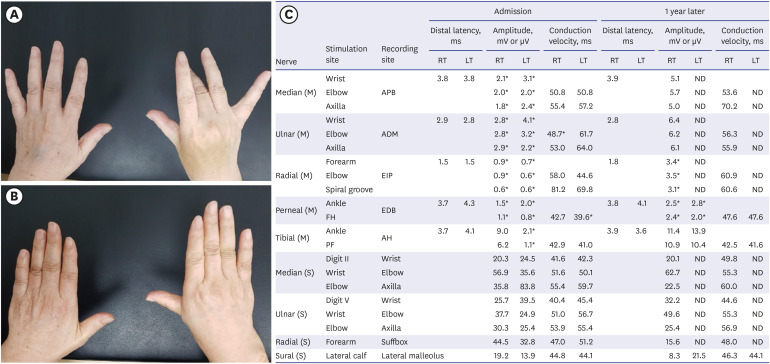 | Fig. 1 Clinical and electrophysiologic findings of the patient. (A) The patient showed bilateral weakness on finger extension, more severe on the right. (B) The finger extension weakness resolved after 19 months. (C) Nerve conduction study revealed axonal motor polyneuropathy on admission with some improvement after 1 year.
|
Nerve conduction study showed decreased amplitude of compound muscle action potentials in all tested motor nerves (
Fig. 1C). Needle electromyography showed active denervation potentials in all extremities and lumbar paraspinal muscles. Cerebrospinal fluid (CSF) analysis showed normal results without albuminocytologic dissociation or pleocytosis. CSF RT-PCR for SARS-CoV-2 was negative. Antiganglioside immunoglobulin G (IgG) and IgM against GM1, GD1b, and GQ1b were negative. Tests for
Campylobacter jejuni, mycoplasma, Epstein-Barr virus, cytomegalovirus, herpes simplex virus, and human immunodeficiency virus were negative.
These findings were consistent with a diagnosis of acute motor axonal neuropathy (AMAN) subtype of GBS with prominent finger dropping. Treatment with intravenous Ig for 5 days greatly improved her condition. A three-month follow-up showed resolution of peripheral weakness except for finger extension, which completely recovered after 19 months (MRC grade 5) (
Fig. 1B).
Ethics statement
Informed consent for publication was obtained from the patient.
Go to :

DISCUSSION
We experienced a COVID-19 patient with GBS presenting with finger extensor weakness. A recent study proposed finger drop-dominant GBS as a new clinical subtype of AMAN with asymmetric and focal weakness patterns, commonly associated with a frequent history of antecedent
C. jejuni enteritis and positive anti-GM1/phosphatidic acid complex or anti-GM1 IgG titers.
1 This variant shows a relatively good prognosis except for the finger extensor weakness.
1 In our case, the patient did not have a history of enteritis or positive anti-GM1 IgG. However, we did not test for anti-GM1/phosphatidic acid complex IgG. Therefore, it is difficult to determine the exact role of these antiganglioside antibodies in the pathogenesis of this case. As in a previous report,
1 our patient showed a good overall outcome despite the widespread denervation potentials in needle electromyography. However, the finger extensor weakness took a long time to recover. This study highlights that some types of COVID-19-related GBS may present as multifocal or asymmetric neuropathy (i.e., finger drop variant), similar to non-COVID-19-related GBS.
Besides the classic GBS, several GBS variants such as Miller Fisher syndrome, pharyngeal-cervical-brachial variant, polyneuritis cranialis, and bifacial weakness with paresthesia have been reported in association with COVID-19.
23 In addition to previous studies, our case further expands the clinical spectrum of GBS in patients with COVID-19.
An interesting point is that our patient remained asymptomatic for COVID-19 despite testing positive on RT-PCR. Since our patient developed GBS symptoms and showed a positive RT-PCR result 14 days after exposure to a confirmed COVID-19 patient, the interval between GBS and COVID-19 is estimated to be less than 14 days. Considering this, parainfectious rather than postinfectious GBS was more likely in our patient. Parainfectious GBS may be related to hyperimmune responses or direct neurotoxic effects rather than molecular mimicry as seen in postinfectious cases.
4 Despite these possible differences in pathogenesis,
4 intravenous Ig showed good responses in COVID-19 patients with parainfectious GBS.
We have highlighted that COVID-19-associated GBS can present in various forms aside from the classic variant, even in patients without any COVID-19 symptoms. Therefore, it is important to always consider the diagnosis of GBS in patients with COVID-19.
Go to :





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download