This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
This study aimed to evaluate the feasibility of surgeon-performed percutaneous transhepatic gallbladder drainage (PTGBD).
Methods
Patients treated with PTGBD for acute cholecystitis (AC), performed by surgeons at Chosun University Hospital for 12 months between March 2017 and February 2018, were enrolled retrospectively, into the S-PTGBD group (n = 134). Patients with PTGBD performed by interventional radiologists for 12 months, 6 months before March 2017, and after February 2018, were included in the X-PTGBD group (n = 107). In addition to the basic characteristics of the patients, severity of AC, comorbidities, intervals from hospital admission to the PTGBDs, procedural times, technical success rates, intention-to-treat rates, and complication rates were evaluated and compared.
Results
Except for the patient’s age (older in S-PTGBD), there were no differences in the patient’s basic profiles, including the severity of the AC and comorbidities. Although the procedural times were significantly shorter in the X-PTGBD group (18.13 minutes vs. 11.39 minutes), effectiveness indicators such as the technical success rates and intention-to-treat rates and safety, such as the major complication rates in the S-PTGBD group, were comparable with those in the X-PTGBD group. The intervals between hospital admissions and PTGBDs were shorter in the S-PTGBD group, although this difference disappeared in the high-risk group. Effectiveness and safety in the high-risk group were also comparable between the groups.
Conclusion
The PTGBDs performed by surgeons are as effective and safe as those performed by interventional radiologists with faster implementation of PTGBD.
Go to :

Keywords: Acute cholecystitis, Drainage, Gallbladder, Surgeons
INTRODUCTION
Acute cholecystitis (AC), the most common biliary disease found in adults, is best treated with cholecystectomy. With the accumulation of experience and techniques in laparoscopic surgery and advancements in patient management, laparoscopic and early cholecystectomies have now been recommended as the standard treatment in patients with AC [
1234]. However, the incidence of AC increases with age because of the increasing prevalence of gallstones, and older patients have more comorbidities [
56]. Older patients with high-risk factors for abdominal surgery are not considered suitable for straightforward cholecystectomies. Thus, there are more patients who need to receive gallbladder drainage first than those who can undergo early cholecystectomies, especially in a tertiary medical center surrounded by many rural areas with aged communities [
7]. Although many approaches have been described [
8], the Tokyo Guidelines 2018 (TG-18) recommend percutaneous transhepatic gallbladder drainage (PTGBD) as the standard method of drainage [
1]. A PTGBD can be offered either as a definitive or temporary measure before a cholecystectomy. It is an effective method for decompressing the septic contents and alleviating the inflammatory processes when there are difficulties in performing immediate surgery. Additionally, because a PTGBD can be offered as a rescue procedure for mortality caused by cholecystitis-related severe sepsis, it is an essential procedure in the medical center, which is responsible for treating patients with AC. The PTGBD has become one of the most common radiological interventional procedures performed on patients in the abdominal surgery department. Although PTGBD is a simple and safe radiological procedure with a low complication rate, it is usually performed by professional radiologists. While studies on the efficacy and safety of PTGBD conducted by interventional radiologists have been published extensively [
9101112], there are no studies evaluating the outcomes of PTGBD when performed by surgeons. This study aimed to assess the effectiveness and safety of PTGBD performed by surgeons.
Go to :

METHODS
This study was approved by the Institutional Review Board of Chosun University Hospital in Gwangju, Korea (No. 2021-10-015). Informed consent was waived because of the retrospective nature of the study.
Patients
During a 12-month period, when an interventional radiologist residing at Chosun University Hospital was absent (from March 2017 to February 2018), hepato-biliary-pancreatic (HBP) surgeons were required to perform PTGBD on their own, after several observations of PTGBD demonstrated by the interventional radiologist. Retrospective data of the patients who received PTGBDs from the surgeons during these 12 months were collected (S-PTGBD group). To compare the outcomes of S-PTGBDs with expert-handed PTGBDs, the data from PTGBDs conducted by an interventional radiologist at our hospital in the same time interval, for a total of 12 months combined before and after 6 months of S-PTGBD period (September 2016 to February 2017 and from March 2018 to August 2018) were collected (X-PTGBD group). Patients who underwent PTGBDs for reasons other than for AC were excluded. Using the diagnostic criteria of TG-18 [
2], AC was diagnosed based on the clinical symptoms, blood test results, and findings on ultrasonography (US) and CT. In the cases of AC with common bile duct stones, patients with obstructed cholangitis were excluded because it was indistinguishable whether improvement of symptoms or laboratory findings were caused by urgent endoscopic retrograde cholangiopancreatography drainages or PTGBDs.
Patients with asymptomatic common bile duct stones were enrolled, and endoscopic retrograde cholangiopancreatography drainages were performed when the patients were in a stable state after the PTGBDs. When there were repeated PTGBDs after the planned or accidental removal of the drainage catheters, only data from the first PTGBD were used for the analysis.
Percutaneous transhepatic gallbladder drainage technique
All procedures were performed in the interventional radiology suite, which had imaging equipment used in fluoroscopy and US, as well as imaging tables and assigned medical staff which included a radiologic technician and nurses. Pethidine (25 mg) was administered to almost all of the patients before the procedure. An attempt was made to insert all the PTGBDs performed by the surgeons using the transhepatic route. After an US-guided puncture of the gallbladder with a Chiba needle under local anesthesia, the Seldinger technique for needle-dilator-catheter exchange along the guidewire under fluoroscopic guidance was used. Finally, an 8.5-French drainage locking pigtail catheter was placed in the gallbladder, and the infected bile was aspirated for culture. Cholecystograms were obtained immediately to confirm the catheter position within the gallbladder [
131415].
Outcomes
In addition to the basic information including age, sex, and body mass index of each patient, the severity of the AC according to the TG-18 [
16] and the severity of the comorbidities using the American Society of Anesthesiologists (ASA) physical status (PS) classification system and the Charlson comorbidity index (CCI) were assessed for disease severity and patient severity. The time interval until the drainage catheter insertion after the hospital visit was calculated to estimate the relevance of the timing. The information associated with the procedure consisted of operator, procedural time, technical success rate, intention-to-treat clinical success rate, and complications. Technical success was defined as the placement of a drainage catheter with the use of imaging guidance to provide continuous drainage of the gallbladder contents. Intention-to-treat clinical success was defined as the reduction of pain, fever, white blood cell counts, and CRPs within 48 hours after the PTGBD [
11]. Complications related to the PTGBD were defined as any event that resulted in an unplanned increase in the level of care, prolonged hospitalization, permanent adverse sequelae, or death. Major complications were defined according to previously published quality improvement guidelines for PTGBD [
11] and included sepsis, hemorrhage, abscess, bile peritonitis (biloma formation), transgression of adjacent structures (intestinal tract and pleura), or death.
Indication for percutaneous transhepatic gallbladder drainage and ‘high-risk patients’
There were no standard indications for PTGBDs at our institution during the study period, and PTGBDs were performed based on the surgeon’s decision. Recently, if the patient was determined to be fit for abdominal surgery, an early cholecystectomy was the standard treatment according to the TG-18 for AC. Thus, we created a subgroup ‘high-risk patients’ to compare the outcomes of the patients who had been identified as those who truly needed PTGBDs, according to the objective guideline, TG-18. In these high-risk patients with a moderate grade of AC, PTGBDs were indicated when early cholecystectomies were not considered safe because of the presence of their comorbidities (ASA PS grade of ≥III or CCI of ≥6) and when antibiotics and general supportive care failed to control the inflammation. In high-risk patients with a severe grade of AC, when there were negative predictive factors including jaundice (total bilirubin of ≥2 mg/dL), neurological dysfunction, or respiratory dysfunction, or when early cholecystectomies were impossible because of the presence of comorbidities (ASA PS grade of ≥3 or CCI of ≥6), PTGBDs were indicated [
2].
Statistical analysis
Data management and analysis were performed using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA). The Student t-test was used to compare the 2 groups for quantitative variables. The categorical variables were assessed using the chi-square test and Fisher exact test. The significance of the results was set at 5%.
Go to :

RESULTS
PTGBD was performed by 2 attending surgeons and 2 surgical residents (under an attendant supervisor) in 142 patients during a 12-month period. PTGBDs were successfully performed by the surgeons in 132 patients (S-PTGBD group) with AC; however, 2 attempts (the 1st and 4th case) failed in the early period due to inexperience; the gallbladder puncture with the Ciba needle did not succeed despite several attempts. The first patient underwent an elective cholecystectomy after conservative treatment, and the fourth patient underwent an emergency laparoscopic cholecystectomy 2 days after the PTGBD attempt because of the deterioration of the symptoms. The PTGBDs performed by the 2 professional interventional radiologists were performed in 107 patients with AC (X-PTGBD group) (
Fig. 1).
 | Fig. 1The composition of the study groups. PTGBD, percutaneous transhepatic gallbladder drainage; S-PTGBD, PTGBD by the surgeon; X-PTGBD, PTGBD by the interventional radiologist.
|
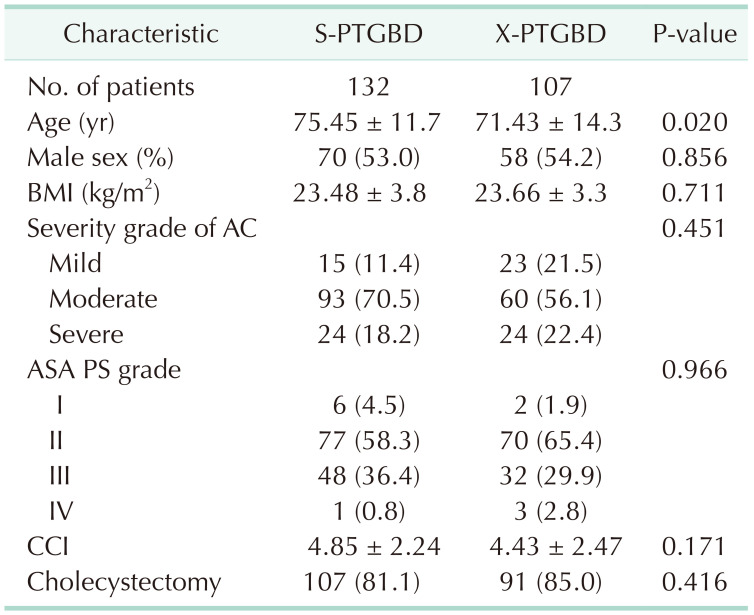
Patients in the S-PTGBD group were older than those in the X-PTGBD group. The severity grade of the AC defined according to the TG-18 was not different between the 2 groups. The physical (ASA PS classification) and comorbidity statuses (CCI) were also not different. The majority of the patients in both of the groups underwent cholecystectomies after PTGBDs (
Table 1).
Table 1
Patient’s characteristics and demographics

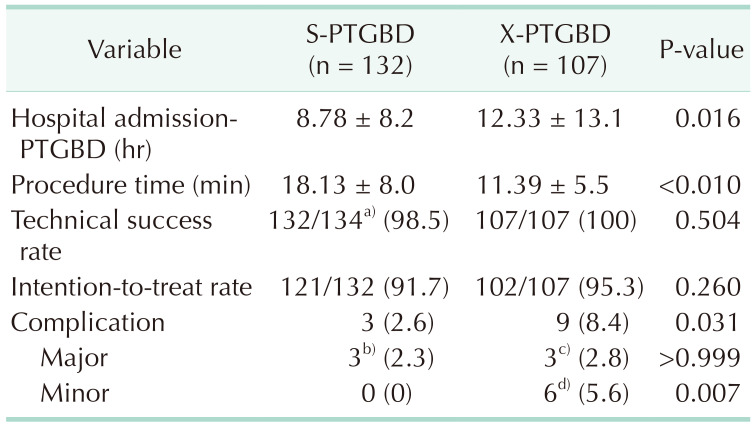
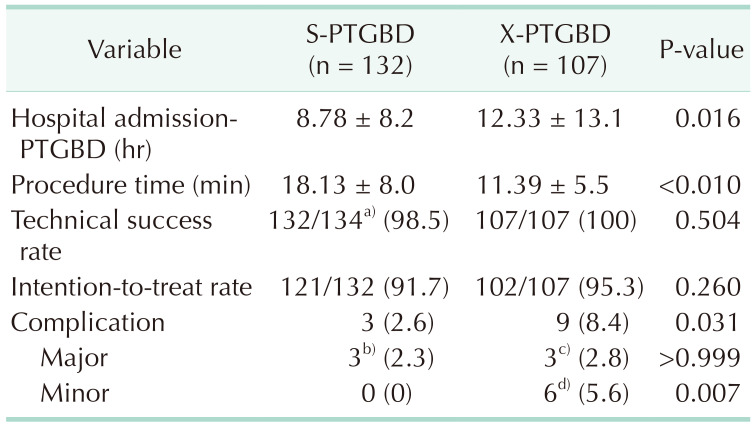
Although there were no differences in the technical success and intention-to-treat rates, the durations between the hospital admission and the implementation of PTGBDs were shorter in the S-PTGBD group, and the procedural times were shorter in the X-PTGBD group (
Table 2). Since more catheter dislodgement occurred inadvertently, there were more complications in the X-PTGBD group; however, there were no significant differences in the major complications between the 2 groups. An 84-year-old female patient died from severe sepsis that developed immediately after a PTGBD in the S-PTGBD group. In the X-PTGBD group, arterial bleeding from the liver puncture site that developed after PTGBD removal during a cholecystectomy was controlled by an electric cauterization of the liver surface. Two bilomas (S-PTGBD, 1 and X-PTGBD, 1) required preoperative drainage because of the presence of symptoms of peritonitis; however, 2 bilomas were found during the cholecystectomies.
Table 2
Procedure-related profiles

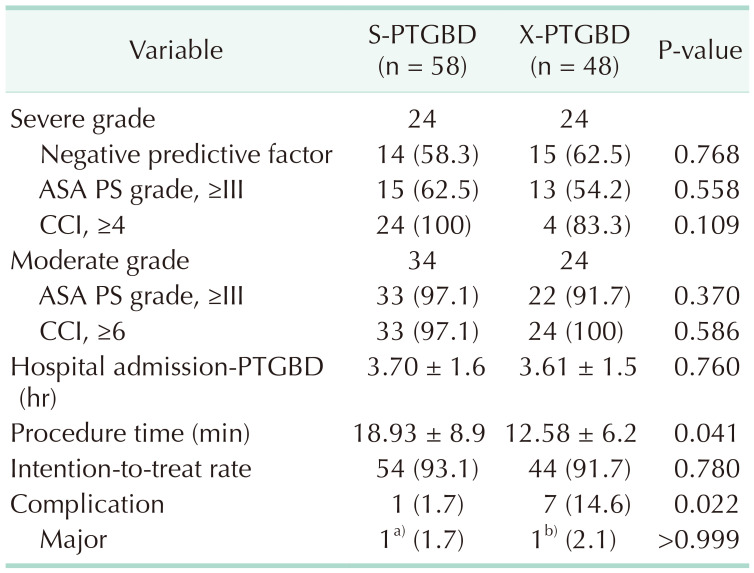
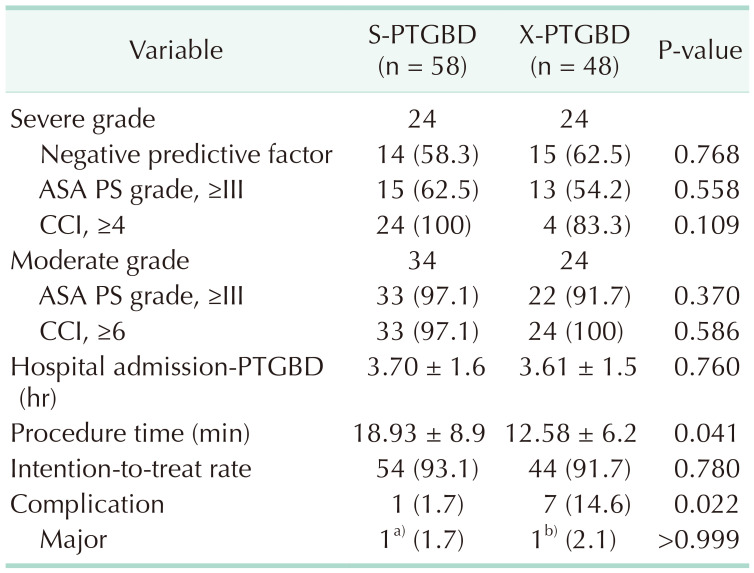
In the analysis of the data set from the high-risk patients (
Table 3), there were no significant differences in time durations from hospital admission to the PTGBDs in which there was a significant difference in the full data set. All the attempts at PTGBDs were successful in the high-risk patients. There was more catheter dislodgement in the X-PTGBD group.
Table 3
High-risk patients

Go to :

DISCUSSION
We performed more than 500 laparoscopic cholecystectomies a year, and 2/3 of the cholecystectomies were performed due to cholecystitis. Many patients who were transferred from elderly care facilities had more aggressive cholecystitis requiring PTGBDs because of their cognitive impairment. All the patients with cholecystitis were cared for by 2 hepatobiliary surgeons at our institution. Without objective indicators or standard guidelines for PTGBDs in our institution during the period of this study, 2 HBP surgeons decided subjectively, whether PTGBDs had to be performed. Generally, when there were gangrenous changes or perforations on the CT images, the patients with AC had severe tenderness or masses in the right upper quadrant area, or their general condition was regarded as infirm, such as the presence of sepsis, in a bedridden state, or with multiple or severe comorbid illnesses. In addition, we did not have consensus regarding emergency or urgent cholecystectomies during the study period. The cholecystectomies were performed electively after the completion of workups for general anesthesia, and this process sometimes required a period of 2 weeks or more, especially in older patients with multiple comorbidities. In these situations, we preferred early PTGBDs for early cholecystectomies. Therefore, 30%–40% of patients with AC should undergo PTGBDs within the period of this study. Although the PTGBDs were performed without standard and consistent protocols, the use of the technically simple and less invasive procedures may improve the patient’s condition rapidly and provide a variety of types of information through the cholecystographies.
With US-guided procedures such as thyroid fine-needle aspirations, central line insertions, thoracocenteses, and paracenteses now being ordinary procedures for the surgeon, the placement of the needle tip into the targeted point under real-time US, even in small vessel lumens or lesions, is not a difficult task for surgical trainees. Radiologic experiences of endovascular interventions by vascular surgeons have made surgeons and surgical trainees familiar with radiologic facilities. Other than the interventional radiologist, doctors working in the radiologic interventional room, such as cardiologists, vascular surgeons, or neurosurgeons, are not strangers to such techniques. Therefore, when the interventional radiologist was absent from our institution, we were easily able to make the decision on the feasibility of performing PTGBD by ourselves.
As shown in
Table 2, despite the lack of differences in the patient characteristics between the S-PTGBD and X-PTGBD groups, except for the patient age, the outcomes of the PTGBDs performed by the surgeon were comparable with the outcomes of the PTGBDs performed by expert interventional radiologists. Although the procedural time was significantly faster in the X-PTGBD group (7 minutes), the technical success rates and intention-to-treat ratios did not differ between the S-PTGBD and X-PTGBD groups. These were also comparable with other investigations [
191011131415]. Furthermore, the quality improvement guidelines for PTGBD published by the Society of Interventional Radiology in 2010 presented thresholds of 90% for the technical success rates and 65%–75% for the intent-to-treat clinical successes [
11]. The outcomes of both the S-PTGBD and X-PTGBD groups were above these thresholds. The major complication rates were low and comparable between the 2 groups. Moreover, there were 6 accidental removals of the PTGBDs (only in the X-PTGBD group). Radiologists usually use a catheter fixation device with adhesive paste, which is attached to the skin. Although its application is convenient, the adhesiveness of this device is weak and it further weakens after several dressing changes. In contrast, the surgeons fix the catheters to the skin with a tagging suture. The skin suture and the tie around the catheter provide firm fixation, preventing inadvertent catheter migration, and simplifying catheter management, especially for long-term use. After identifying this difference, we refixed the catheter with the tagging suture even after the application of adhesive fixation devices if there were any risks of accidental catheter dislodgement, such as in patients with dementia and limited activity, and in long-term use.
The time interval from hospital admission to PTGBDs in the S-PTGBD group was shorter by approximately 4 hours. This result may be explained by the fact that the surgeons who decided that the patient receive a PTGBD performed the PTGBD simultaneously in the S-PTGBD group. However, surgeons in the X-PTGBD group had to consult an interventional radiologist to discuss whether the patient needed a PTGBD and the surgeon would avoid contact with a radiologist at night, unless the situation was urgent, such as in cases with septic shock induced by the AC. This situation explained the longer mean hours and larger standard deviations of time from hospital admission to the PTGBDs in the X-PTGBD group. Short time interval to gallbladder drainage is one of the advantages of surgeon-performed PTGBD. The PTGBD that is safely conducted by surgeons with a fast decision and instantaneous implementation can relieve patient’s symptoms quickly and improve patient’s condition rapidly. Therefore, oral nutritional support and daily activities can be started earlier in the patients with AC.
But this difference disappeared in the analysis of the high-risk patients (
Table 3). Patients who were surgically unfit for early cholecystectomies and who had organ dysfunction or severe comorbidities received drainage procedures urgently in both groups (3.7 ± 1.6 hours after hospital visit in the S-PTGBD group and 3.61 ± 1.5 hours in the X-PTGBD group). This result suggested that PTGBDs were performed within an appropriate time for all the patients who actually needed a drainage procedure for AC.
The main limitation of this study was its retrospective nature without a standard indication for PTGBDs, which limited the data available for analysis. Further research should be undertaken to investigate the feasibility of the indicated PTGBD.
This was the first study to investigate the feasibility of PTGBDs when performed by HBP surgeons. A PTGBD is a simple and safe procedure, and the surgeon-performed PTGBDs for patients with AC had acceptable success rates, intention-to-treat rates, and complication rates. Surgeons can perform PTGBDs as effectively and safely as expert interventional radiologists with more rapid processes in the patients with AC.
Go to :





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download