1. Sharma L. Osteoarthritis of the Knee. N Engl J Med. 2021; 384(1):51–59. PMID:
33406330.
2. Kim YE, Jo MW, Park H, Oh IH, Yoon SJ, Pyo J, et al. Updating disability weights for measurement of healthy life expectancy and disability-adjusted life year in Korea. J Korean Med Sci. 2020; 35(27):e219. PMID:
32657086.
3. Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 2020; 72(2):220–233. PMID:
31908163.
4. Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019; 27(11):1578–1589. PMID:
31278997.
5. Pendleton A, Arden N, Dougados M, Doherty M, Bannwarth B, Bijlsma JW, et al. EULAR recommendations for the management of knee osteoarthritis: report of a task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2000; 59(12):936–944. PMID:
11087696.
6. American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. Pain Med. 2009; 10(6):1062–1083. PMID:
19744205.
7. Bruyère O, Cooper C, Pelletier JP, Maheu E, Rannou F, Branco J, et al. A consensus statement on the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) algorithm for the management of knee osteoarthritis—from evidence-based medicine to the real-life setting. Semin Arthritis Rheum. 2016; 45(4 Suppl):S3–11. PMID:
26806188.
8. McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014; 22(3):363–388. PMID:
24462672.
9. Gore M, Tai KS, Sadosky A, Leslie D, Stacey BR. Use and costs of prescription medications and alternative treatments in patients with osteoarthritis and chronic low back pain in community-based settings. Pain Pract. 2012; 12(7):550–560. PMID:
22304678.
10. Kingsbury SR, Gross HJ, Isherwood G, Conaghan PG. Osteoarthritis in Europe: impact on health status, work productivity and use of pharmacotherapies in five European countries. Rheumatology (Oxford). 2014; 53(5):937–947. PMID:
24489012.
11. Park HR, Cho SK, Im SG, Jung SY, Kim D, Jang EJ, et al. Treatment patterns of knee osteoarthritis patients in Korea. Korean J Intern Med. 2019; 34(5):1145–1153. PMID:
29551051.
12. Cho SK, Jung SY, Choi S, Im SG, Kim H, Choi WS, et al. Factors related to the use of opioids as early treatment in patients with knee osteoarthritis. Arthritis Res Ther. 2019; 21(1):222. PMID:
31685008.
13. Sabha M, Hochberg MC. Non-surgical management of hip and knee osteoarthritis; comparison of ACR/AF and OARSI 2019 and VA/DoD 2020 guidelines. Osteoarthritis and Cartilage Open. 2022; 4(1):100232.
14. Stewart M, Cibere J, Sayre EC, Kopec JA. Efficacy of commonly prescribed analgesics in the management of osteoarthritis: a systematic review and meta-analysis. Rheumatol Int. 2018; 38(11):1985–1997. PMID:
30120508.
15. Puljak L, Marin A, Vrdoljak D, Markotic F, Utrobicic A, Tugwell P. Celecoxib for osteoarthritis. Cochrane Database Syst Rev. 2017; 5(5):CD009865. PMID:
28530031.
16. Park JS, Lee CH. Clinical study using healthcare claims database. J Rheum Dis. 2021; 28(3):119–125.
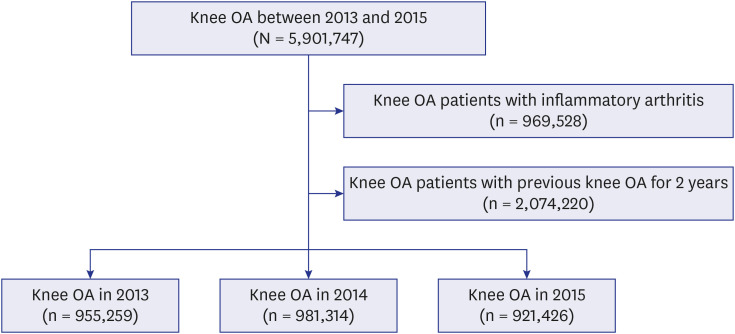
17. Park HR, Im S, Kim H, Jung SY, Kim D, Jang EJ, et al. Validation of algorithms to identify knee osteoarthritis patients in the claims database. Int J Rheum Dis. 2019; 22(5):890–896. PMID:
30729731.
18. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998; 36(1):8–27. PMID:
9431328.
19. Kozma CM, Dickson M, Phillips AL, Meletiche DM. Medication possession ratio: implications of using fixed and variable observation periods in assessing adherence with disease-modifying drugs in patients with multiple sclerosis. Patient Prefer Adherence. 2013; 7:509–516. PMID:
23807840.
20. Dalal D, Dubreuil M, Peloquin C, Neogi T, Zhang Y, Choi H, et al. Meloxicam and risk of myocardial infarction: a population-based nested case-control study. Rheumatol Int. 2017; 37(12):2071–2078. PMID:
29030657.
21. Cryer B, Feldman M. Cyclooxygenase-1 and cyclooxygenase-2 selectivity of widely used nonsteroidal anti-inflammatory drugs. Am J Med. 1998; 104(5):413–421. PMID:
9626023.
22. Curtis E, Fuggle N, Shaw S, Spooner L, Ntani G, Parsons C, et al. Safety of cyclooxygenase-2 inhibitors in osteoarthritis: outcomes of a systematic review and meta-analysis. Drugs Aging. 2019; 36(Suppl 1):25–44. PMID:
31073922.
23. Tang YZ, Zeng P, Liao Y, Qin Z, Zhang H, Li B, et al. Correlation between perioperative parecoxib use and postoperative acute kidney injury in patients undergoing non-cardiac surgery: a retrospective cohort analysis. BMJ Open. 2021; 11(8):e047840.
24. Hochberg MC. Mortality in osteoarthritis. Clin Exp Rheumatol. 2008; 26(5):Suppl 51. S120–S124. PMID:
19026154.
25. Nüesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Jüni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ. 2011; 342:d1165. PMID:
21385807.
26. Cooper C, Chapurlat R, Al-Daghri N, Herrero-Beaumont G, Bruyère O, Rannou F, et al. Safety of oral non-selective non-steroidal anti-inflammatory drugs in osteoarthritis: what does the literature say? Drugs Aging. 2019; 36(1):Suppl 1. 15–24. PMID:
31073921.
27. Park KK, Choi CH, Ha CW, Lee MC. The effects of adherence to non-steroidal anti-inflammatory drugs and factors influencing drug adherence in patients with knee osteoarthritis. J Korean Med Sci. 2016; 31(5):795–800. PMID:
27134504.
28. Wu R, Ma Y, Yang Y, Li M, Zheng Q, Fu G. A clinical model for predicting knee replacement in early-stage knee osteoarthritis: data from osteoarthritis initiative. Clin Rheumatol. 2022; 41(4):1199–1210. PMID:
34802087.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download