1. Tao K, Tzou PL, Nouhin J, Gupta RK, de Oliveira T, Kosakovsky Pond SL, et al. The biological and clinical significance of emerging SARS-CoV-2 variants. Nat Rev Genet. 2021; 22(12):757–773. PMID:
34535792.
2. World Health Organization. WHO coronavirus disease (COVID-19) dashboard. Updated 2020. Accessed July 31, 2021.
https://covid19.who.int/info
.
3. Kang E, Lee SY, Kim MS, Jung H, Kim KH, Kim KN, et al. The physiological burden of COVID-19 stigma: evaluation of the mental health of isolated mild condition COVID-19 patients. J Korean Med Sci. 2021; 36(3):1–13.
4. Choi I, Kim JH, Kim N, Choi E, Choi J, Suk HW, et al. How COVID-19 affected mental well-being: an 11- week trajectories of daily well-being of Koreans amidst COVID-19 by age, gender and region. PLoS One. 2021; 16(4):e0250252. PMID:
33891642.
5. Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med. 2020; 21(5):1059–1066. PMID:
32970555.
6. Nickell LA, Crighton EJ, Tracy CS, Al-Enazy H, Bolaji Y, Hanjrah S, et al. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. 2004; 170(5):793–798. PMID:
14993174.
7. Khalid I, Khalid TJ, Qabajah MR, Barnard AG, Qushmaq IA. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016; 14(1):7–14. PMID:
26847480.
8. Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020; 28(5):1002–1009. PMID:
32255222.
9. Park C, Hwang JM, Jo S, Bae SJ, Sakong J. COVID-19 outbreak and its association with healthcare workers’ emotional stress: a cross-sectional study. J Korean Med Sci. 2020; 35(41):e372. PMID:
33107230.
10. Savoia E, Argentini G, Gori D, Neri E, Piltch-Loeb R, Fantini MP. Factors associated with access and use of PPE during COVID-19: a cross-sectional study of Italian physicians. PLoS One. 2020; 15(10):e0239024. PMID:
33044978.
11. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020; 324(8):782–793. PMID:
32648899.
12. Ontario Agency for Health Protection and Promotion (Public Health Ontario). IPAC recommendations for use of personal protective equipment for care of individuals with suspect or confirmed COVID-19 (6th revision). Updated 2021. Accessed July 31, 2021.
https://www.publichealthontario.ca/
.
13. Zhang SX, Liu J, Afshar Jahanshahi A, Nawaser K, Yousefi A, Li J, et al. At the height of the storm: healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav Immun. 2020; 87(1):144–146. PMID:
32387345.
14. Delgado D, Wyss Quintana F, Perez G, Sosa Liprandi A, Ponte-Negretti C, Mendoza I, et al. Personal safety during the COVID-19 pandemic: realities and perspectives of healthcare workers in Latin America. Int J Environ Res Public Health. 2020; 17(8):2798.
15. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971; 12(6):371–379. PMID:
5172928.
16. Lee JH. Development of the Korean form of Zung’s self-rating anxiety scale. Yeungnam Univ J Med. 1996; 13(2):279–294.
17. Unoki T, Tamoto M, Ouchi A, Sakuramoto H, Nakayama A, Katayama Y, et al. Personal protective equipment use by healthcare workers in Intensive Care Unit during the COVID-19 pandemic in Japan: Comparative analysis with the PPE-SAFE survey. Acute Med Surg. 2020; 7(1):e584.
18. Ranney ML, Griffeth V, Jha AK. Critical supply shortages - the need for ventilators and personal protective equipment during the COVID-19 pandemic. N Engl J Med. 2020; 382(18):e41. PMID:
32212516.
20. Bohlken J, Schömig F, Lemke MR, Pumberger M, Riedel-Heller SG. COVID-19 pandemic: stress experience of healthcare workers - a short current review. Psychiatr Prax. 2020; 47(4):190–197. PMID:
32340048.
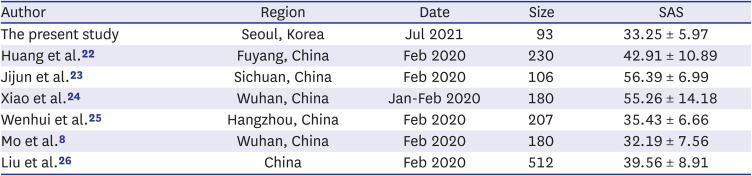
22. Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020; 38(3):192–195. PMID:
32131151.
23. Jijun W, Xian S, Fei C, Yuanjie D, Dechun C, Xingcao J, et al. Investigation on sleep quality of first line nurses in fighting against novel coronavirus pneumonia and its influencing factors. Nurs Res China. 2020; 34(7):558–562.
24. Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020; 26:e923549. PMID:
32132521.
25. Wenhui Z, Er L, Yi Z. Investigation and countermeasures of anxiety of nurses in a designated hospital of novel coronavirus pneumonia in Hangzhou. Health Res. 2020; 40:130–133.
26. Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect. 2020; 148:e98. PMID:
32430088.
27. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020; 323(21):2133–2134. PMID:
32259193.
28. Delaney RK, Locke A, Pershing ML, Geist C, Clouse E, Precourt Debbink M, et al. Experiences of a health system’s faculty, staff, and trainees’ career development, work culture, and childcare needs during the COVID-19 pandemic. JAMA Netw Open. 2021; 4(4):e213997. PMID:
33797552.
29. Pan R, Zhang L, Pan J. The anxiety status of Chinese medical workers during the epidemic of COVID-19: a meta-analysis. Psychiatry Investig. 2020; 17(5):475–480.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download