Abstract
Although decompressive craniectomy is an effective treatment for various situations of increased intracranial pressure, it may be accompanied by several complications. Paradoxical herniation is known as a rare complication of lumbar puncture in patients with decompressive craniectomy. A 38-year-old man underwent decompressive craniectomy for severe brain swelling. He remained neurologically stable for five weeks, but then showed mental deterioration right after a lumbar puncture which was performed to rule out meningitis. A brain computed tomographic scan revealed a marked midline shift. The patient responded to the Trendelenburg position and intravenous fluids, and he achieved full neurologic recovery after successive cranioplasty. The authors discuss the possible mechanism of this rare case with a review of the literature.
Decompressive craniectomy is widely performed to reduce uncontrollable intracranial pressure (ICP) which is difficult to treat by medical management alone5). However, patients who undergo decompressive craniectomy may develop an unusual paradoxical herniation1,4). To date, only a few cases of paradoxical herniation have been reported, and to our knowledge, only one report on paradoxical herniation after decompressive craniectomy for traumatic brain injury has been issued in Korea3). In that case, however, it was not related to lumbar puncture. Measures are needed to raise intracranial pressure against the forces generated by atmospheric pressure and herniation. Here, we present an uncommon case of paradoxical transtentorial herniation after lumbar puncture, which was reversed by the Trendelenburg position and sufficient hydration.
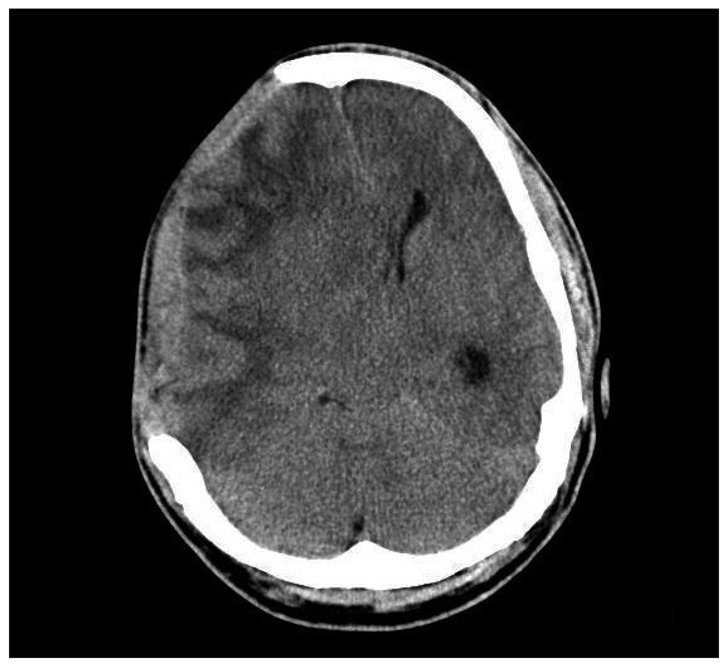
A 38-year-old man was presented with mental deterioration after head injury. Two hours after the accident, he became stuporous with Glasgow Coma Scale of 9. Brain computed tomography (CT) revealed a hemorrhagic contusion in the right frontotemporoparietal region and acute epidural hematoma in the left temporo-occipital region (Fig. 1). Routine laboratory tests, which included platelet count, prothrombin time, and activated partial thromboplastin time were within normal limits. He has not taken any antiplatelet agents prior to the injury. The patient underwent emergent decompressive craniectomy on right frontotemporoparietal region, followed by craniotomy for removal of epidural hematoma on the left side (Fig. 2). Postoperatively, he became conscious and was able to obey commands without any neurologic deficit. Five weeks later, he complained of a febrile sensation and had fever by 38.0℃. Brain CT scan showed no midline shift (Fig. 3). Furthermore, his WBC count was increased to 11500/mL and erythrocyte sedimentation rate to 48 mm/hr. Lumbar puncture was performed to rule out pyogenic meningitis. He underwent an uncomplicated lumbar puncture with an 18-gauge spinal needle followed by the drainage of only 20 mL CSF. The opening pressure was 14 cmH2O without evidence of pyogenic meningitis. CSF analysis revealed 4 WBC cells/mm3 with glucose level of 50 mg/dL. After lumbar puncture, he complained of severe headache and dizziness. Two days later he was found to be deeply drowsy with left hemiparesis to the extent of having difficulty to obey commands. A brain CT showed marked herniation to the left (Fig. 4). Under the diagnosis of paradoxical transtentorial herniation, he was placed in the Trendelenburg position and sufficient hydration was given intravenously. After the conservative treatment alone, he recovered gradually over a week. By then, he was able to obey commands and showed alert consciousness. Follow-up brain CT revealed resolution of the midline shift (Fig. 5). Cranioplasty was performed 4 months after the head injury and brain CT after cranioplasty showed complete resolution of the shift (Fig. 6).
The indications of decompressive craniectomy are expanding1). These include traumatic brain injury with medically refractory intracranial pressures, subdural hematoma, and cerebral swelling due to vasospasm after a subarachnoid hemorrhage. Due to the fact that the cranium of the patients who have undergone craniectomy does not provide a rigid structure, the 'invisible' mass effects of atmospheric pressure and gravity can overwhelm the intracranial contents and transtentorial herniation is possible even in the absence of increased ICP7). Paradoxical herniation has been referred to as the herniation of a brain that has been decompressed surgically, without any extra-axial lesion that could account for the herniation7,11). Those treatments for lowering ICP, such as mannitol, CSF drainage, and hyperventilation, all of which follows the Monro-Kellie doctrine will exacerbate paradoxical herniation, because lowering intracranial pressure increases the pressure gradient across the craniectomy defect6,7). This phenomenon is related to the negative gradient between atmospheric and intracranial pressures, which can be exacerbated by an upright posture, CSF leakage, or dehydration4). Patients who have undergone CSF drainage, such as, external ventriculostomy, ventriculoperitoneal shunt placement, or lumbar puncture are more susceptible to this phenomenon, for these conditions can lower ICP states relatively than that of extra-cranial pressures. In these situations, the brain is sucked down through the tentorial incisural notch essentially and the foramen magnum potentially6). Not surprisingly, the pressure acting over the cerebral cortex may cause neurological deficits. Several authors have claimed that skull defects may create a siphon effect on CSF dynamics, which distorts the dura, underlying cerebral cortex, and venous return, due to scarring and direct pressure to the brain2,9). Symptoms may include focal deficits, brainstem release signs, autonomic instability, changes in level of consciousness, and pupil changes3,4). There are few cases of paradoxical transtentorial herniation after lumbar puncture causing negative pressure gradient between the intracranial space and the spinal canal7,11). Because it is exacerbated by a negative pressure gradient, its management involves eliminating the pressure gradient. In the presented case, we could obtain immediate neurological recovery by placing the patient in the Trendelenburg position and by hydrating adequately. Furthermore, cranioplasty, conceptual conversion of an 'open box' to 'closed box' can sometimes be the definitive treatment for paradoxical herniation. The striking neurological improvements observed in some cranioplasty patients with deteriorated consiousness, particularly in those with sunken scalp flaps, lead to the recognition of 'the syndrome of the trephined'5). Schiffer et al.10) and Liao and Kao6) reported that focal neurological deterioration could be improved after skull defect reconstruction in some hemicraniectomy patients. Furthermore, CT perfusion studies have found that cranioplasty can improve cerebral perfusion8). We successfully managed our patient by adopting the Trendelenburg position and sufficient hydration and by performing early cranioplasty. We advise that the possibility of paradoxical herniation in patients who have undergone decompressive craniectomy when lumbar puncture is performed and lumbar puncture should be carried out carefully in patients with decompressive craniectomy.
Although it has been rare, neurosurgeons should keep in mind the possibility of paradoxical herniation in patients that have undergone decompressive craniectomy whenever lumbar puncture is inevitable. We recommend that the Trendelenburg position with adequate hydration and subsequent cranioplasty should be considered as a preferential treatment option.
References
1. Akins PT, Guppy KH. Sinking skin flaps, paradoxical herniation, and external brain tamponade : a review of decompressive craniectomy management. Neurocrit Care. 2008; 9:269–276. PMID: 18064408.

2. Ban SP, Son YJ, Yang HJ, Chung YS, Lee SH, Han DH. Analysis of complications following decompressive craniectomy for traumatic brain injury. J Korean Neurosurg Soc. 2010; 48:244–250. PMID: 21082053.

3. Cho H, Kim CH, Kim JH, Kim JM. Paradoxical Herniation after decompressive craniectomy for acute subdural hematoma. J Korean Neurosurg Soc. 2006; 40:51–53.
4. Fields JD, Lansberg MG, Skirboll SL, Kurien PA, Wijman CA. "Paradoxical" transtentorial herniation due to CSF drainage in the presence of a hemicraniectomy. Neurology. 2006; 67:1513–1514. PMID: 17060591.

5. Fodstad H, Love JA, Ekstedt J, Fridén H, Liliequist B. Effect of cranioplasty on cerebrospinal fluid hydrodynamics in patients with the syndrome of the trephined. Acta Neurochir (Wien). 1984; 70:21–30. PMID: 6741628.

6. Liao CC, Kao MC. Cranioplasty for patients with severe depressed skull bone defect after cerebrospinal fluid shunting. J Clin Neurosci. 2002; 9:553–555. PMID: 12383414.

7. Oyelese AA, Steinberg GK, Huhn SL, Wijman CA. Paradoxical cerebral herniation secondary to lumbar puncture after decompressive craniectomy for a large space-occupying hemispheric stroke : case report. Neurosurgery. 2005; 57:E594. discussion E594. PMID: 16145506.
8. Richaud J, Boetto S, Guell A, Lazorthes Y. [Effects of cranioplasty on neurological function and cerebral blood flow]. Neurochirurgie. 1985; 31:183–188. PMID: 4033856.
9. Sakamoto S, Eguchi K, Kiura Y, Arita K, Kurisu K. CT perfusion imaging in the syndrome of the sinking skin flap before and after cranioplasty. Clin Neurol Neurosurg. 2006; 108:583–585. PMID: 15921849.

10. Schiffer J, Gur R, Nisim U, Pollak L. Symptomatic patients after craniectomy. Surg Neurol. 1997; 47:231–237. PMID: 9068692.

11. Vilela MD. Delayed paradoxical herniation after a decompressive craniectomy : case report. Surg Neurol. 2008; 69:293–296. discussion 296. PMID: 17586009.

Fig. 1
Initial computed tomography scan shows hemorrhagic contusion in the right fronto-temporo-parietal region with severe brain swelling and epidural hematoma in the left temporo-occipital region.
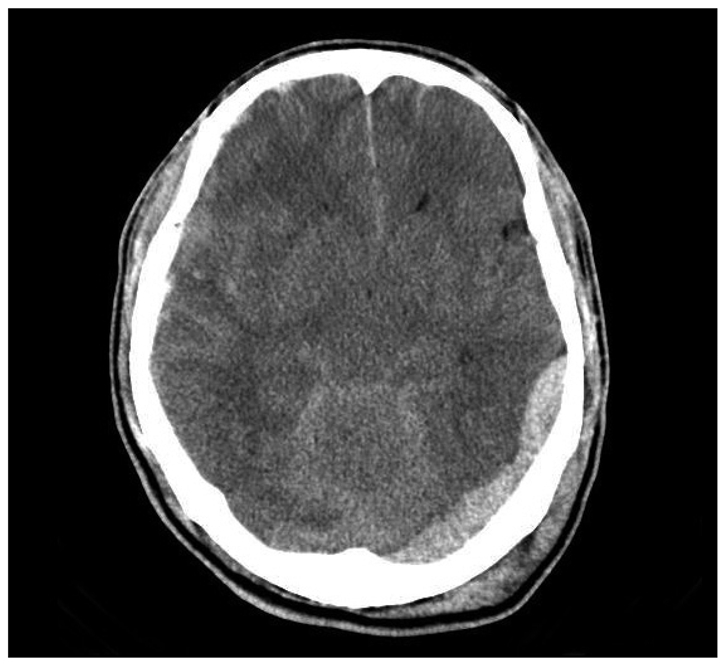
Fig. 2
After emergent right fronto-temporo-parietal craniectomy operation, brain computed tomographic scan shows the removal of epidural hematoma and improvement of brain swelling.
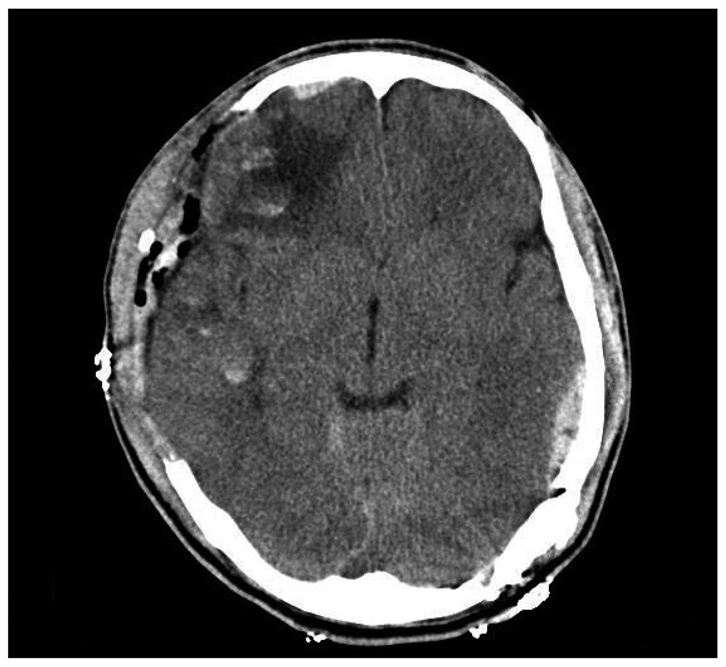
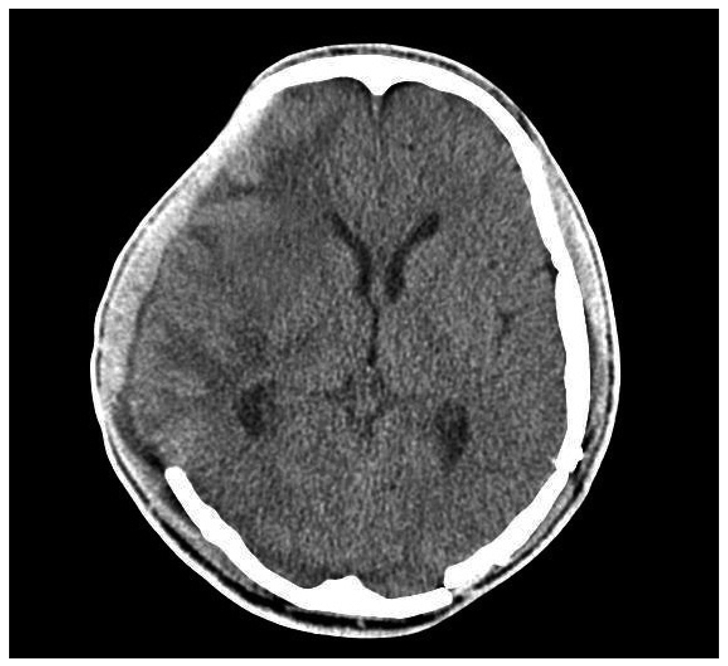
Fig. 3
Computed tomographic scan taken five weeks postoperatively and just before lumbar puncture shows no midline shift.
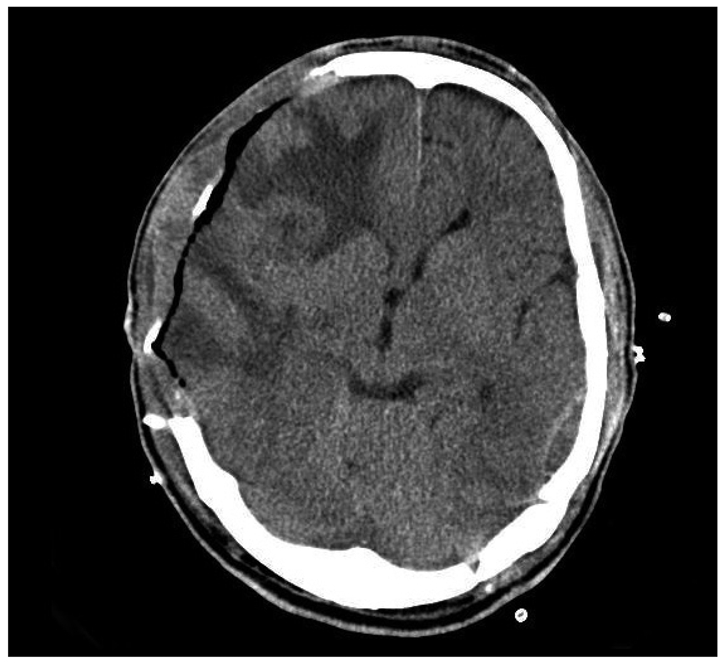
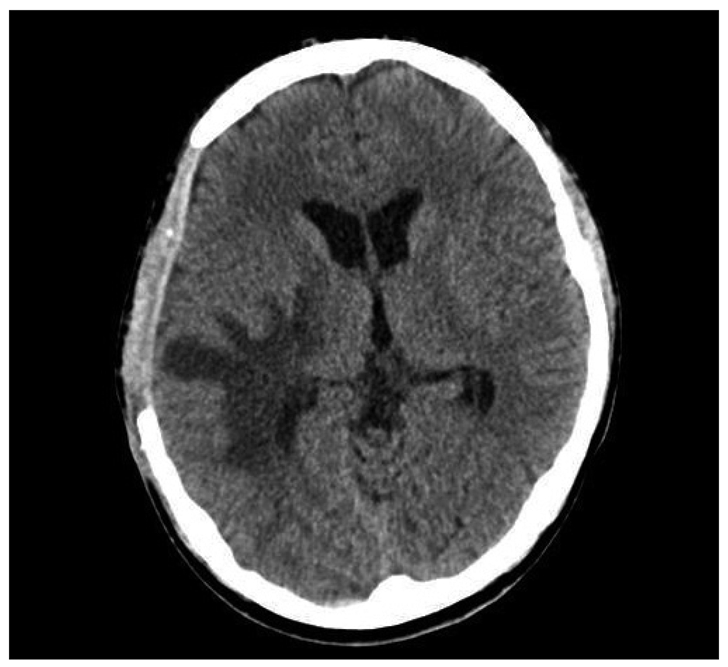
Fig. 4
Brain computed tomographic scan after lumbar puncture reveals midline shift to the left and transtentorial herniation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download