1. Anasetti F, Galbusera F, Aziz HN, Bellini CM, Addis A, Villa T, et al. Spine stability after implantation of an interspinous device : an in vitro and finite element biomechanical study. J Neurosurg Spine. 2010; 13:568–575. PMID:
21039145.

2. Bono CM, Lee CK. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years : influence of technique on fusion rate and clinical outcome. Spine (Phila Pa 1976). 2004; 29:455–463. discussion Z5PMID:
15094543.

3. Byun DH, Shin DA, Kim JM, Kim SH, Kim HI. Finite element analysis of the biomechanical effect of coflex™ on the lumbar spine. Korean J Spine. 2012; 9:131–136. PMID:
25983803.

4. Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003; 85-A:2089–2092. PMID:
14630835.

5. Chen SH, Zhong ZC, Chen CS, Chen WJ, Hung C. Biomechanical comparison between lumbar disc arthroplasty and fusion. Med Eng Phys. 2009; 31:244–253. PMID:
18760654.

6. Chosa E, Goto K, Totoribe K, Tajima N. Analysis of the effect of lumbar spine fusion on the superior adjacent intervertebral disk in the presence of disk degeneration, using the three-dimensional finite element method. J Spinal Disord Tech. 2004; 17:134–139. PMID:
15260097.

7. Erbulut DU, Zafarparandeh I, Hassan CR, Lazoglu I, Ozer AF. Determination of the biomechanical effect of an interspinous process device on implanted and adjacent lumbar spinal segments using a hybrid testing protocol : a finite-element study. J Neurosurg Spine. 2015; 23:200–208. PMID:
25932601.

8. Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis : a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine (Phila Pa 1976). 1997; 22:2807–2812. PMID:
9431616.
9. Gaines RW Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000; 82-A:1458–1476. PMID:
11057475.

10. Goel VK, Monroe BT, Gilbertson LG, Brinckmann P. Interlaminar shear stresses and laminae separation in a disc. Finite element analysis of the L3-L4 motion segment subjected to axial compressive loads. Spine (Phila Pa 1976). 1995; 20:689–698. PMID:
7604345.
11. Jutte PC, Castelein RM. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J. 2002; 11:594–598. PMID:
12522719.

12. Kang KT, Kim HJ, Son J, Yeom JS, Chun HJ. Comparing an instrumented posterior fixation system with rigid and semi-flexible rods using finite element analysis. Int J Precis Eng Manuf. 2015; 16:163–170.

13. Kim HJ, Bak KH, Chun HJ, Oh SJ, Kang TH, Yang MS. Posterior interspinous fusion device for one-level fusion in degenerative lumbar spine disease : comparison with pedicle screw fixation - preliminary report of at least one year follow up. J Korean Neurosurg Soc. 2012; 52:359–364. PMID:
23133725.

14. Kim HJ, Chun HJ, Moon SH, Kang KT, Kim HS, Park JO, et al. Analysis of biomechanical changes after removal of instrumentation in lumbar arthrodesis by finite element analysis. Med Biol Eng Comput. 2010; 48:703–709. PMID:
20440570.

15. Kim TY, Kang KT, Yoon DH, Shin HC, Kim KN, Yi S, et al. Effects of lumbar arthrodesis on adjacent segments : differences between surgical techniques. Spine (Phila Pa 1976). 2012; 37:1456–1462. PMID:
22333957.
16. Lavaste F, Skalli W, Robin S, Roy-Camille R, Mazel C. Three-dimensional geometrical and mechanical modelling of the lumbar spine. J Biomech. 1992; 25:1153–1164. PMID:
1400515.

17. Lo CC, Tsai KJ, Chen SH, Zhong ZC, Hung C. Biomechanical effect after Coflex and Coflex rivet implantation for segmental instability at surgical and adjacent segments : a finite element analysis. Comput Methods Biomech Biomed Engin. 2011; 14:969–978. PMID:
21607887.

18. Park SC, Yoon SH, Hong YP, Kim KJ, Chung SK, Kim HJ. Minimum 2-year follow-up result of degenerative spinal stenosis treated with interspinous u (coflex). J Korean Neurosurg Soc. 2009; 46:292–299. PMID:
19893715.

19. Polikeit A, Nolte LP, Ferguson SJ. The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit : finite-element analysis. Spine (Phila Pa 1976). 2003; 28:991–996. PMID:
12768136.

20. Rohlmann A, Bauer L, Zander T, Bergmann G, Wilke HJ. Determination of trunk muscle forces for flexion and extension by using a validated finite element model of the lumbar spine and measured in vivo data. J Biomech. 2006; 39:981–989. PMID:
16549091.

21. Rohlmann A, Neller S, Claes L, Bergmann G, Wilke HJ. Influence of a follower load on intradiscal pressure and intersegmental rotation of the lumbar spine. Spine (Phila Pa 1976). 2001; 26:E557–E561. PMID:
11740371.

22. Rohlmann A, Zander T, Bergmann G. Spinal loads after osteoporotic vertebral fractures treated by vertebroplasty or kyphoplasty. Eur Spine J. 2006; 15:1255–1264. PMID:
16311752.

23. Serhan H, Mhatre D, Defossez H, Bono CM. Motion-preserving technologies for degenerative lumbar spine : the past, present, and future horizons. SAS J. 2011; 5:75–89. PMID:
25802672.

24. Shirazi-Adl SA, Shrivastava SC, Ahmed AM. Stress analysis of the lumbar disc-body unit in compression. A three-dimensional nonlinear finite element study. Spine (Phila Pa 1976). 1984; 9:120–134. PMID:
6233710.

25. Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bünger CE. 1997 Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion : a prospective, randomized clinical study. Spine (Phila Pa 1976). 1997; 22:2813–2822. PMID:
9431617.
26. Vadapalli S, Sairyo K, Goel VK, Robon M, Biyani A, Khandha A, et al. Biomechanical rationale for using polyetheretherketone (PEEK) spacers for lumbar interbody fusion-a finite element study. Spine (Phila Pa 1976). 2006; 31:E992–E998. PMID:
17172990.

27. Xiao Z, Wang L, Gong H, Zhu D. Biomechanical evaluation of three surgical scenarios of posterior lumbar interbody fusion by finite element analysis. Biomed Eng Online. 2012; 11:31. PMID:
22709659.

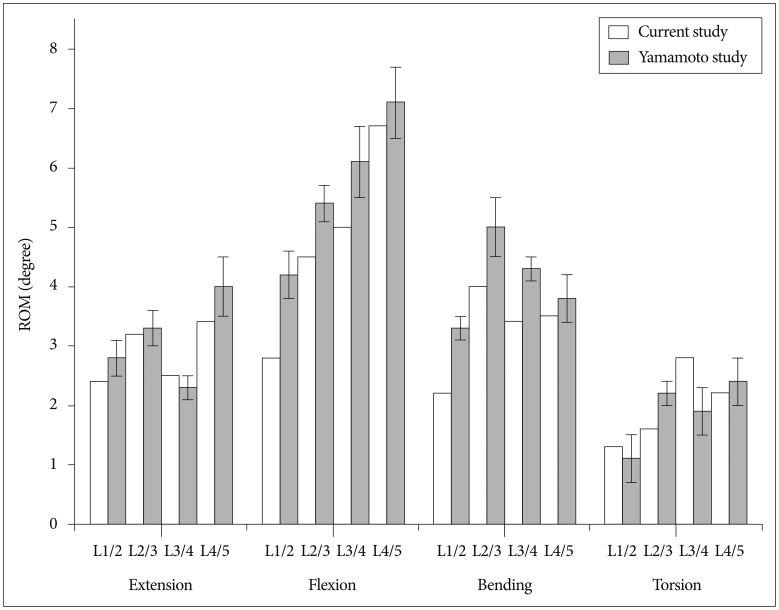
28. Yamamoto I, Panjabi MM, Crisco T, Oxland T. Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine (Phila Pa 1976). 1989; 14:1256–1260. PMID:
2603060.

29. Zhong ZC, Wei SH, Wang JP, Feng CK, Chen CS, Yu CH. Finite element analysis of the lumbar spine with a new cage using a topology optimization method. Med Eng Phys. 2006; 28:90–98. PMID:
16426979.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download