1. Agrawal A, Cincu R, Goel A. Current concepts and controversies in the management of non-functioning giant pituitary macroadenomas. Clin Neurol Neurosurg. 2007; 109:645–650. PMID:
17686573.

2. Beardsley C, Egerton T, Skinner B. Test-re-test reliability and inter-rater reliability of a digital pelvic inclinometer in young, healthy males and females. PeerJ. 2016; 4:e1881. PMID:
27069812.

3. Burke SM, Hwang SW, Mehan WA Jr, Bedi HS, Ogbuji R, Riesenburger RI. Reliability of the modified Tufts Lumbar Degenerative Disc Classification between neurosurgeons and neuroradiologists. J Clin Neurosci. 2016; 29:111–116. PMID:
27021223.

4. Casanueva FF, Molitch ME, Schlechte JA, Abs R, Bonert V, Bronstein MD, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006; 65:265–273. PMID:
16886971.

5. Chang EF, Zada G, Kim S, Lamborn KR, Quinones-Hinojosa A, Tyrrell JB, et al. Long-term recurrence and mortality after surgery and adjuvant radiotherapy for nonfunctional pituitary adenomas. J Neurosurg. 2008; 108:736–745. PMID:
18377253.

6. Cunningham S. Inter-rater reliability and validity of the screenassist lumbar questionnaire : a pilot study. J Man Manip Ther. 2015; 23:254–263. PMID:
26952154.

7. de Divitiis E, Laws ER, Giani U, Iuliano SL, de Divitiis O, Apuzzo ML. The current status of endoscopy in transsphenoidal surgery : an international survey. World Neurosurg. 2015; 83:447–454. PMID:
25535063.

8. Dehdashti AR, Ganna A, Karabatsou K, Gentili F. Pure endoscopic endonasal approach for pituitary adenomas : early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery. 2008; 62:1006–1015. discussion 1015-1017. PMID:
18580798.

9. Dusick JR, Esposito F, Malkasian D, Kelly DF. Avoidance of carotid artery injuries in transsphenoidal surgery with the Doppler probe and micro-hook blades. Neurosurgery. 2007; 60(4 Suppl 2):322–328. discussion 328-329. PMID:
17415170.

10. Ferreli F, Turri-Zanoni M, Canevari FR, Battaglia P, Bignami M, Castelnuovo P, et al. Endoscopic endonasal management of non-functioning pituitary adenomas with cavernous sinus invasion : a 10- year experience. Rhinology. 2015; 53:308–316. PMID:
26301431.

11. Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions. ed 3. Hoboken, NJ: John Wiley & Sons;2004. p. 598–626.
12. Hardy J, Vezina JL. Transsphenoidal neurosurgery of intracranial neoplasm. Adv Neurol. 1976; 15:261–273. PMID:
945663.
13. Ho RW, Huang HM, Ho JT. The influence of pituitary adenoma size on vision and visual outcomes after trans-sphenoidal adenectomy : a report of 78 cases. J Korean Neurosurg Soc. 2015; 57:23–31. PMID:
25674340.

14. Hwang JM, Kim YH, Kim JW, Kim DG, Jung HW, Chung YS. Feasibility of endoscopic endonasal approach for recurrent pituitary adenomas after microscopic trans-sphenoidal approach. J Korean Neurosurg Soc. 2013; 54:317–322. PMID:
24294455.

15. Jung KW, Ha J, Lee SH, Won YJ, Yoo H. An updated nationwide epidemiology of primary brain tumors in republic of Korea. Brain Tumor Res Treat. 2013; 1:16–23. PMID:
24904884.

16. Juraschka K, Khan OH, Godoy BL, Monsalves E, Kilian A, Krischek B, et al. Endoscopic endonasal transsphenoidal approach to large and giant pituitary adenomas : institutional experience and predictors of extent of resection. J Neurosurg. 2014; 121:75–83.

17. Kim BY, Shin JH, Kang SG, Kim SW, Hong YK, Jeun SS, et al. Bilateral modified nasoseptal "rescue" flaps in the endoscopic endonasal transsphenoidal approach. Laryngoscope. 2013; 123:2605–2609. PMID:
23553463.

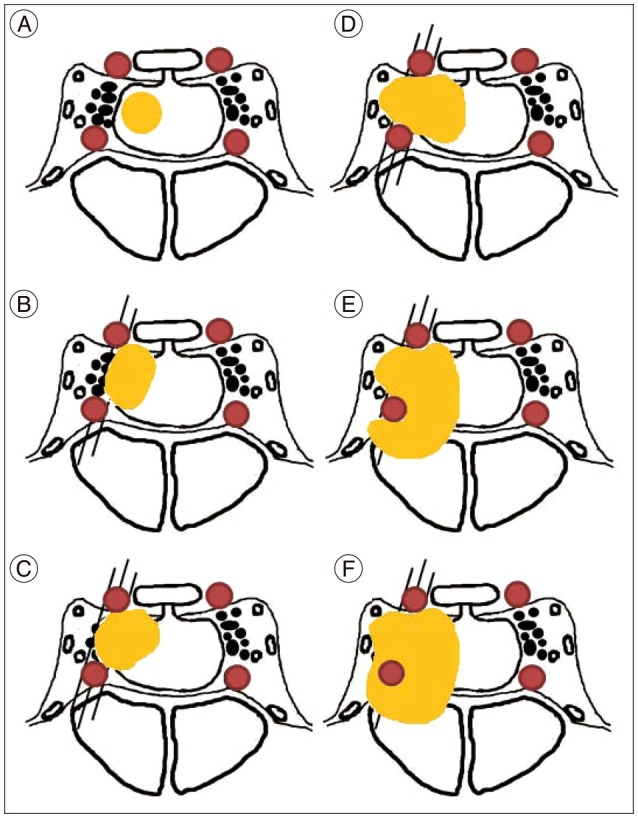
18. Knosp E, Steiner E, Kitz K, Matula C. Pituitary adenomas with invasion of the cavernous sinus space : a magnetic resonance imaging classification compared with surgical findings. Neurosurgery. 1993; 33:610–617. discussion 617-618. PMID:
8232800.

19. Magro E, Graillon T, Lassave J, Castinetti F, Boissonneau S, Tabouret E, et al. Complications related to the endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary macroadenomas in 300 consecutive patients. World Neurosurg. 2016; 89:442–453. PMID:
26902781.

20. Mazur MD, Taussky P, Shah LM, Winegar B, Park MS. Inter-rater reliability of published flow diversion occlusion scales. J Neurointerv Surg. 2016; 1. 20. DOI:
10.1136/neurintsurg-2015-012193. [Epub ahead of print].

21. Micko AS, Wöhrer A, Wolfsberger S, Knosp E. Invasion of the cavernous sinus space in pituitary adenomas : endoscopic verification and its correlation with an MRI-based classification. J Neurosurg. 2015; 122:803–811. PMID:
25658782.

22. Mortini P. Cons : endoscopic endonasal transsphenoidal pituitary surgery is not superior to microscopic transsphenoidal surgery for pituitary adenomas. Endocrine. 2014; 47:415–420. PMID:
25081297.

23. Ostrom QT, Gittleman H, Liao P, Rouse C, Chen Y, Dowling J, et al. CBTRUS statistical report : primary brain and central nervous system tumors diagnosed in the United States in 2007-2011. Neuro Oncol. 16(Suppl 4):2014; iv1–iv63. PMID:
25304271.
24. Park JH, Choi JH, Kim YI, Kim SW, Hong YK. Modified graded repair of cerebrospinal fluid leaks in endoscopic endonasal transsphenoidal surgery. J Korean Neurosurg Soc. 2015; 58:36–42. PMID:
26279811.

25. van Lummel RC, Walgaard S, Hobert MA, Maetzler W, van Dieën JH, Galindo-Garre F, et al. Intra-rater, inter-rater and test-retest reliability of an instrumented timed up and go (iTUG) test in patients with Parkinson's disease. PLoS One. 2016; 11:e0151881. PMID:
26999051.

26. Zaidi HA, Awad AW, Bohl MA, Chapple K, Knecht L, Jahnke H, et al. Comparison of outcomes between a less experienced surgeon using a fully endoscopic technique and a very experienced surgeon using a microscopic transsphenoidal technique for pituitary adenoma. J Neurosurg. 2016; 124:596–604. PMID:
26473774.

27. Zhou T, Wang F, Meng X, Ba J, Wei S, Xu B. Outcome of endoscopic transsphenoidal surgery in combination with somatostatin analogues in patients with growth hormone producing pituitary adenoma. J Korean Neurosurg Soc. 2014; 56:405–409. PMID:
25535518.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download