1. Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy--average 14-year follow-up study. Spine (Phila Pa 1976). 2006; 31:2998–3005. PMID:
17172996.

2. Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ. Anterior correction of cervical kyphotic deformity : effects on myelopathy, neck pain, and sagittal alignment. J Neurosurg. 2004; 100:13–19. PMID:
14748568.

3. Fujiyoshi T, Yamazaki M, Okawa A, Kawabe J, Hayashi K, Endo T, et al. Static versus dynamic factors for the development of myelopathy in patients with cervical ossification of the posterior longitudinal ligament. J Clin Neurosci. 2010; 17:320–324. PMID:
20071177.

4. Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986; 11:521–524. PMID:
3787320.

5. Masaki Y, Yamazaki M, Okawa A, Aramomi M, Hashimoto M, Koda M, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament : anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech. 2007; 20:7–13. PMID:
17285045.

6. Masson C, Leys D, Meder JF, Dousset V, Pruvo JP. [Spinal cord ischemia]. J Neuroradiol. 2004; 31:35–46. PMID:
15026730.
7. Matsunaga S, Nakamura K, Seichi A, Yokoyama T, Toh S, Ichimura S, et al. Radiographic predictors for the development of myelopathy in patients with ossification of the posterior longitudinal ligament : a multicenter cohort study. Spine (Phila Pa 1976). 2008; 33:2648–2650. PMID:
19011547.

8. Morio Y, Nagashima H, Teshima R, Nawata K. Radiological pathogenesis of cervical myelopathy in 60 consecutive patients with cervical ossification of the posterior longitudinal ligament. Spinal Cord. 1999; 37:853–857. PMID:
10602528.

9. Oshima Y, Seichi A, Takeshita K, Chikuda H, Ono T, Baba S, et al. Natural course and prognostic factors in patients with mild cervical spondylotic myelopathy with increased signal intensity on T2-weighted magnetic resonance imaging. Spine (Phila Pa 1976). 2012; 37:1909–1913. PMID:
22511231.

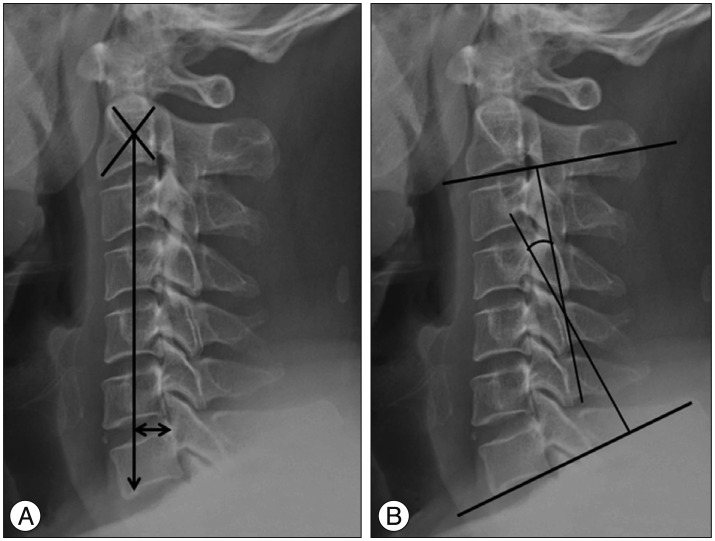
10. Pavlov H, Torg JS, Robie B, Jahre C. Cervical spinal stenosis : determination with vertebral body ratio method. Radiology. 1987; 164:771–775. PMID:
3615879.

11. Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2003; 28:1258–1262. PMID:
12811268.

12. Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2015; 76(suppl 1):S14–S21. PMID:
25692364.

13. Taniyama T, Hirai T, Yamada T, Yuasa M, Enomoto M, Yoshii T, et al. Modified K-line in magnetic resonance imaging predicts insufficient decompression of cervical laminoplasty. Spine (Phila Pa 1976). 2013; 38:496–501. PMID:
22986838.

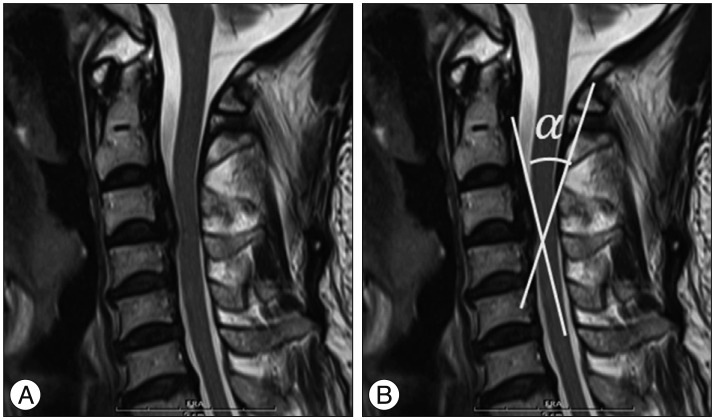
14. Tokuhashi Y, Matsuzaki H, Oda H, Uei H. Effectiveness of posterior decompression for patients with ossification of the posterior longitudinal ligament in the thoracic spine : usefulness of the ossification-kyphosis angle on MRI. Spine (Phila Pa 1976). 2006; 31:E26–E30. PMID:
16395163.
15. Tousignant M, de Bellefeuille L, O'Donoughue S, Grahovac S. Criterion validity of the cervical range of motion (CROM) goniometer for cervical flexion and extension. Spine (Phila Pa 1976). 2000; 25:324–330. PMID:
10703104.

16. Tsukimoto H. On an autopsied case of compression myelopathy with a callus formation in the cervical spinal canal. Nihon Geka Hokan. 1960; 29:1003–1007.
17. Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. 1984; (184):71–84. PMID:
6423334.

18. Vedantam R, Lenke LG, Keeney JA, Bridwell KH. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine (Phila Pa 1976). 1998; 23:211–215. PMID:
9474728.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download