Abstract
Objective
Delayed hinge fracture (HF) that develops after cervical open door laminoplasty can be a source of postoperative complications such as axial pain. However, risk factors related to this complication remain unclear. We performed a retrospective clinical series to determine risk factors for delayed HF following plate-only open-door cervical laminoplasty.
Methods
Patients who underwent plate-only open-door laminoplasty and had available postoperative computed tomography (CT) scans (80 patients with 270 laminae) were enrolled. Hinge status, hinge gutter location, open location, hinge width, number of screws used, operation level, and open angle were observed in the CT to determine radiographic outcome. Demographic data were collected as well. Radiographic and clinical parameters were analyzed using univariate and multivariate logistic regression analysis to determine the risk factors for HF.
Results
Univariate logistic regression analysis results indicated poor initial hinge status, medially placed hinge gutter, double screw fixation on the elevated lamina, upper surgical level, and wide open angle as predictors for HF (p<0.05). Initial hinge status seemed to be the most powerful risk factor for HF (p=0.000) and thus was collinear with other variables. Therefore, multivariate logistic regression analysis was performed excluding initial hinge status, and the results indicated that medially placed hinge gutter, double screw fixation on the elevated lamina, and upper surgical level were risk factors for HF after adjustment for other confounding factors.
Cervical laminoplasty is a standard treatment for multi-segment spinal canal stenosis. It is usually used to treat cervical spondylotic myelopathy, ossification of the posterior longitudinal ligament, and cervical disk herniation associated with developmental spinal canal stenosis13). Open-door laminoplasty is one of the most popular surgical methods that provides enough decompression of the spinal canal over multiple segments and reconstructs the stable laminar arch with sufficient room for the spinal cord27121517). The basic principle of this technique is elastic deformation of thinned lamina, which allows complete healing. When the procedure was relatively new, Hirabayashi used a wire for lamina fixation; however, open lamina reclosure or fracture was a problem23). O'Brien et al.8) modified open-door type laminoplasty by augmenting the procedure with titanium plates to maintain patency of the deformed lamina. Nevertheless, deformed lamina fractures were still observed in several cases21014). These so-called hinge fractures (HFs) could happen intra-operatively while manipulating the hinge but also post-operatively in recovery stage, which are defined as delayed HFs10). However, only few surgeons have investigated about HFs because the lamina is well fused in the majority of cases, and most surgeons believe that HFs do not exert much influence over clinical outcomes. Some recent studies have indicated that HFs can cause axial pain or palsy that may be chronic21014). Our previous study showed that patients with 3 or more HFs experienced significant worsening of visual analog scales for neck (VASn) and neck disability index (NDI) compared with patients with 2 HFs or less in multi-level open door laminoplasty cases10). Nevertheless, risk factors related to this complication remain unclear. Therefore, we radiographically evaluated hinge status and determined risk factors for delayed HFs following plate-only open-door cervical laminoplasty.
From April 2005 to January 2012, 119 patients with cervical myelopathy underwent open-door laminoplasty in our hospitals. Among them, 80 patients who had postoperative computed tomography (CT) scans within 2 years were enrolled in this study. All of the 80 patients suffered from myelopathic symptoms, such as motor weakness, sensory disturbance, or voiding difficulties. Table 1 shows the demographics of the studied patients. There were 45 patients with spondylotic myelopathy, 32 with symptomatic ossification of the posterior longitudinal ligament, and 3 with developmental stenosis. The mean age of the patients was 58 years (range : 32–78 years). The male : female ratio was 49 : 31. Among the patients, 17 were smokers.
All surgeries were performed by a senior surgeon who used a modification of the classic Hirabayashi open-door technique, securing the opened lamina with a titanium miniplate (Medtronic, Memphis, TN, USA)23). Details of the surgical method are described in our previous study10). Briefly, gutters were created at the junction of the lateral mass and lamina. Open side and hinge side gutters were made using a cutting burr and a Kerrison rongeur, respectively. A green-stick deformation of the hinge was produced and laminar elevation and miniplate fixation were performed. One 7 mm screw was placed into the lateral mass through the plate and one 5 mm screw was placed through the plate into the cut lamina in 65 patients. In 16 patients, two screws were used in both the lateral mass and the lamina. One plate was used for each level in all cases.
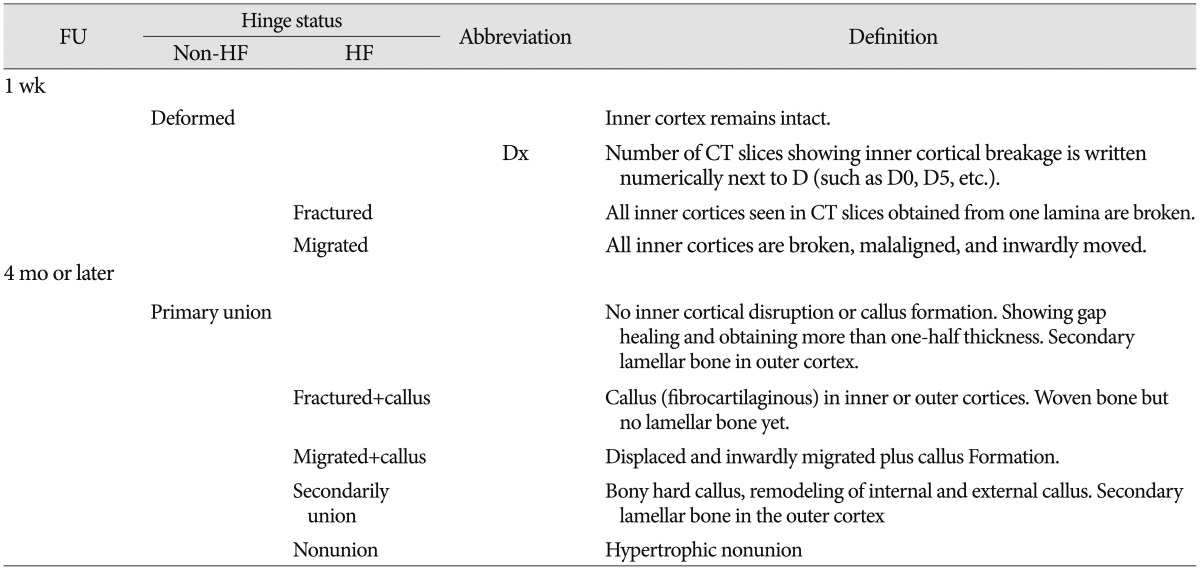
CT scanning was performed with a 16-multidetector CT (MDCT) scanner (Sensation; Siemens, Erlangen, Germany). Images were reconstructed using 2-mm-thick sections with no intervals and were optimized for evaluation of bony structures (width, 1500; center, 450). Postoperative axial CT scans were independently evaluated by three different reviewers (three neurosurgeons). The initial status of the hinge gutter and delayed HFs were evaluated as described previously (Table 2)10). Briefly, hinges were defined as deformed if the ventral cortices were bent but not broken (non-HF). The number of slices with a broken or disconnected inner cortex was counted among six or seven thin slices of CT scans obtained from a single lamina (Dx) which indicates poor hinge status as disconnected number increases. If all of the inner cortices were broken, it was defined as fractured, and if the inner cortices had moved inside, it was defined as migrated and these are all considered as HFs. In later observations, primary union (PU) was considered as non-HF. Contrastively, nonunion, callus formation, and secondary union (SU) which demonstrates healing process occurred after fracture were considered as HF. The healing status of each lamina was determined by consensus of two or more of the three reviewers. Fig. 1 shows radiographic measurements of hinge-side gutter and open-side gutter location, open angle, and hinge width.
Kappa coefficients were used to check the reliability of initial and delayed hinge status assessments among observers. Continuous variables (age, radiographic measurements, number of screws) are shown as means±standard deviations, whereas categorical variables (hinge status, surgical level, sex, and smoking) are expressed as ratios or percentages. Pearson's correlation was used for continuous variables and Spearman's correlation was used for categorical variables. To identify variables independently related to HFs, univariate or multivariate logistic regression analysis were used. In the logistic regression model, the HF group and non-HF group were treated as dependent variables. All tests were two-sided, and a value of p<0.05 was considered statistically significant. All analysis were performed with SPSS software (version 20.0; SPSS, Chicago, IL, USA).
A total of 114 CT scans from 80 patients were available for the assessment of hinge status : 38 patients at 1 week after surgery, and 76 patients at 4 months after surgery or later up until 2 years. The mean number of operated levels was 4.5 (range : 3–7) and the mean number of laminoplasties was 3.3 (range : 2–5). This discrepancy comes from the combination of partial C7 laminotomy and total C3 laminectomy. The total number of levels that had undergone open-door laminoplasty was 270.
The CTs from 80 patients and a total of 270 laminae levels were evaluated for radiographic measurements. The mean hinge open angle was 30±4 degrees (range 21–39 degrees), which was a narrow range. The average hinge and open locations were 1.5±0.9 mm (range 0–4.1 mm) and 0.5±0.7 mm (range 0–3.5 mm), respectively. Hinge width averaged 2.7±0.6 mm (range 1.5–4.6 mm). Initial hinge gutter status (Dx) was evaluated with CTs taken from 38 patients 1 week after surgery, and 10% (12 of 115) of hinges were found to be in danger of fracture or overtly fractured (D6 or worse) (Table 3). However, CTs taken at 4 months or later postoperatively (76 patients) showed an increased number of HFs (117 of 254, 46%) which indicates that majority of HFs occurred at delayed period rather than perioperative period.
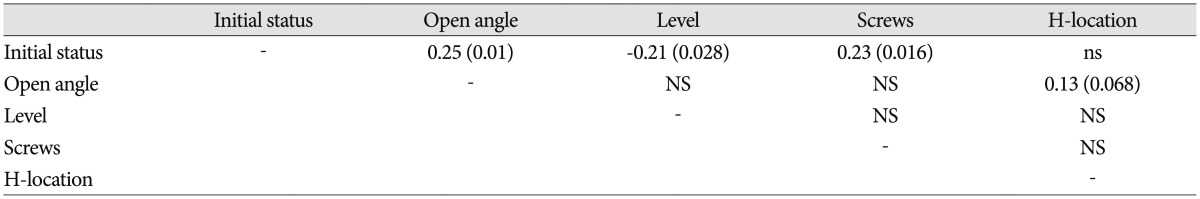
The CT scans of 34 patients, who had both 1-week and later observations, were evaluated to verify the relationship between the independent variables including initial hinge status, open angle, operated level, number of screws used, and hinge-location. Initial hinge status and the open angle, operated level, number of screws used showed high correlation (p<0.05). Results are shown in Table 4.
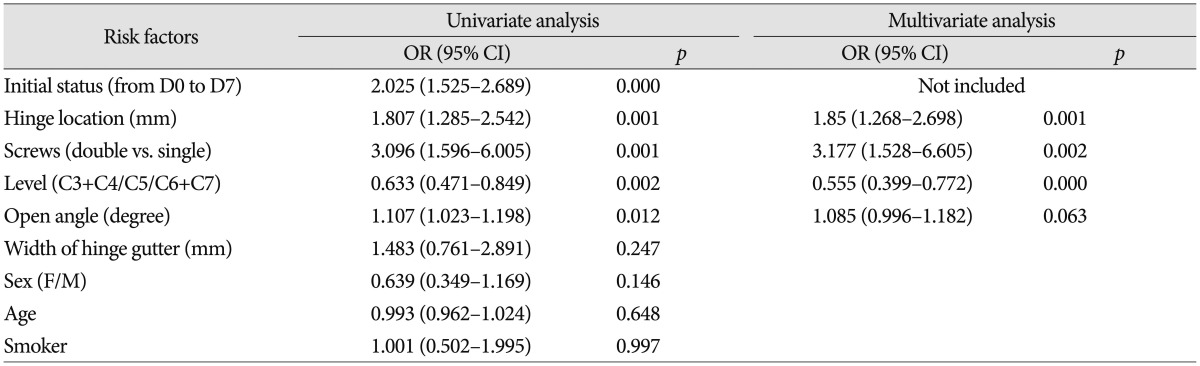
Univariate and multivariate logistic regression analysis were both used to identify HF risk factors among several variables within 80 patients (38 patients for initial hinge status). Hinge width, sex, age, and smoking were statistically nonsignificant (p>0.05). Poor initial hinge status [odds ratio (OR)=2.025, 95% CI=1.525–2.689], medially placed hinge gutter (OR=1.807, 95% CI=1.285–2.542), double screw fixation on the elevated lamina (OR=3.096, 95% CI=1.596–6.005), upper surgical level (OR=0.633, 95% CI=0.471–0.849), and wide open angle (OR=1.107, 95% CI=1.023–1.198) were identified as predictors of HFs by univariate logistic analysis (p<0.05). Among them, the multivariate logistic regression showed that poor initial hinge status (OR=1.982, 95% CI=1.413–2.780), medially placed hinge gutter (OR=2.376, 95% CI=1.271–4.440), and surgical level (OR=0.367, 95% CI=0.204–0.662) were risk factors for HFs after adjustment for other confounding factors, but double screw fixation was excluded. However, because the multivariate analysis results seemed to be biased due to colinearity between initial status and other variables (Table 4), additional multivariate analysis without initial hinge status was performed. Medially placed hinge gutter (OR=1.85, 95% CI=1.286–2.698), double screw fixation on the elevated lamina (OR=3.177, 95% CI=1.528–6.605), upper surgical level (OR=0.555, 95% CI=0.399–0.772), and wide open angle (OR=1.085, 95% CI=0.996–1.182) had very similar ORs to univariate logistic regression analysis and was statistically meaningful (p<0.05) except open angle (p=0.063). Overall results are shown in Table 5.
Laminoplasty typically achieves good operative results. However, there are still some postoperative complications despite many preventative efforts. C5 palsy is a representative complication of laminoplasty, with an average occurrence of 4.6% (range 0–30%) patients after laminoplasty13). Many studies have attempted to determine the pathologic mechanism of C5 palsy, which is still unclear. Satomi et al.15) reviewed postoperative CT scans of patients with weakness on the hinge side, which implicated the lamina dropping into the spinal canal as the cause of weakness in 4 patients among 16. This suggests that the downward displacement of the elevated lamina into the spinal canal might injure the nerve root131415).
Since Hosono et al.4) first reported axial symptoms in 1996, there have been many clinical reports of persistent axial neck and shoulder pain after laminoplasty9). Such pain is currently one of the most well-known complications of cervical laminoplasty. Possible sources of neck pain include dissected nuchal muscles, destroyed zygapophysial joints, and injured nerve roots24). Recently, some authors have postulated that HF may be a source of postoperative pain21014). Hosono et al.4) suggested that the gutter on the hinge side causes shoulder pain until bony union is completed in this area. Tsuji16) reported that hinge gutter shows radiologic union within 1 year and postoperative shoulder pain also subsides within this period. Our previous study also showed that multiple fractures of laminae can aggravate postoperative VASn and NDI.10)
As HF may increase C5 palsy and axial pain occurrence, HF prevention could be important for favorable post-operative outcome. Therefore, risk factors for HFs would be important for precautions. However, to the best of our knowledge, there are no existing studies that determined HF risk factors; this study is the first attempt. In the present study, multivariate logistic regression analysis indicated that poor initial hinge status, medially located hinge gutter, and upper cervical level are risk factors of HFs after laminoplasty. Double screws used for a single lamina are also thought to be a risk factor following interpretation of the multivariate logistic regression analysis excluding initial hinge status.
The prevalence of delayed HF was highly correlated with initial hinge status. As the count of disconnected inner cortex CT slices increased (i.e., D6 or worse), occurrence rate of delayed HF increased simultaneously. The variation in univariate and multivariate logistic regression OR was very small (2.025 vs. 1.982). This indicates poor initial hinge status as a firm risk factor for delayed HFs. This is likely because poor initial hinge status may be similar to an HF. Consequently, as a confounding factor on multivariate logistic regression, initial hinge status could distort the results of other independent factors. Furthermore, poor initial hinge status is highly correlated with other independent factors, thus the real correlation of other factors with HF could be devalued. Therefore, only hinge location, double screws, level, and open angle were sorted out as independent variables and additionally analyzed using multivariate logistic regression. This also has additional meaning to exclude the incomplete data, because initial hinge status data were collected from 38 patients instead of 80.
Hinge gutter location has also been proposed to be an important variable2). In this study, medially placed hinge gutters had a high OR and significant p-value in both univariate and multivariate logistic regression analyses. Specifically, comparing univariate logistic regression to multivariate logistic regression without initial status, OR (1.807 vs. 1.85) was very similar and both p-values (0.001, 0.002) were also highly statistically significant. This means that the medial gutter tends to break easily. This result corresponds with Hirabayashi's study2). The reason for this result is unclear but there are several possibilities. First, the medial lamina is thinner than the lateral lamina and a thin gutter would be fragile. Second, even with the same length of elevation, open angle increases with medial gutter placement. This makes the gutter more compound and stressful, which could lead to HF. However, it is difficult to say if a more lateral hinge gutter always results in a good outcome. Because a lateral hinge gutter is a possible risk factor for C5 palsy and axial pain, some clinicians insist that the outcome of making a medial hinge gutter is better than making a lateral one6).
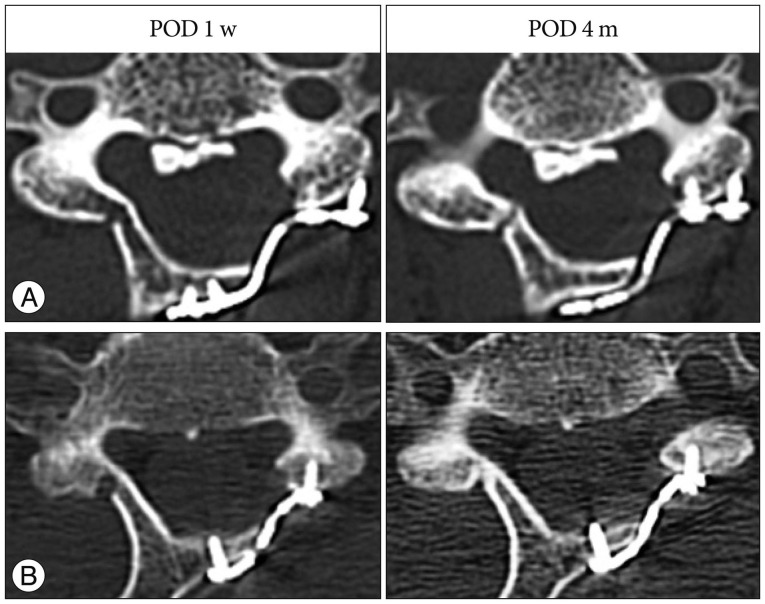
Although there were no significant differences between single screw and double screw use in initial multivariate logistic regression analysis (with initial hinge status), it seems to be a predictor of HF. First, because of the formulaic technique, constant open angle was a prerequisite between two groups (30±4 in single, 29±3 in double). However, there was a significant difference in the initial status average between the two groups (p=0.0163, Mann-Whitney U test; median=D0 in single, D2 in double screw). This revealed that the use of two screws to fill in the lamina may worsen its status. The initial multivariate analysis result seemed to be due to colinearity. It may be that when a screw is tightened in a clockwise rotatory motion, the hinge's unidirectional shear stress might increase. Therefore, second multivariate analysis (without initial hinge status) seemed to be more reliable. Fig. 2 shows representative cases.
Comparing C3 & C4 with C5, or C5 & C6 and C7, the upper level had a high OR compared to the adjacent lower level. The remote level (C3 & C4 and C6 & C7) showed a more significant difference. The reasons for this result are unknown. We hypothesize that it could be because of anatomic predisposition that the upper lamina is usually thinner than the lower. In addition, when elevation has been accomplished, the reformed lamina moves backward and becomes twisted slightly cranially so that its rostral end becomes closer to the upper intact lamina. For this reason, undercutting of the cranial lamina is usually needed. On the contrary, the lower end lamina moves backward and away from the intact lamina below. Hence, the lower end laminae obtain more room to move freely. Thus, on neck extension, the upper lamina is more likely to contact the intact lamina10). Another possible explanation is because of different healing rates. Rhee et al.11) claimed that C6 and C7 tended to have high union rates and healing speed compared to C4 and C5. A high healing rate could draw a low rate of HF.
Univariate logistic regression analysis indicated wide open angle to be a predictor of HF but multivariate analysis did not. Our surgical technique for hinge opening was standardized, thus the open angle varied within a narrow range (30±4 degrees). This could lead to statistical weakness. An OR near 1 also supports this concept. Alternatively, open angle and initial hinge status may essentially be correlated with each other. Using a load deformation curve (Young modulus) as reference, if open angle becomes larger, it will pass by the elastic range and plastic range (deformation), and mechanical failure could occur. In this case, hinge status could be poor at the first week postoperative CT evaluation. Therefore, open angle and hinge status may be colinear, which could distort the multivariate analysis results. In fact, initial hinge status and open angle were positively correlated (r statistic=0.25, p=0.01), as determined by 115 hinges. Multivariate analysis without initial hinge status had a better p-value (0.063 vs. 0.171), but it was still greater than 0.05. Combining two hypotheses could better explain the result. Further information is shown in Table 4, 5.
Hinge width had no correlation with HF (p=0.247). More force should be exerted on a narrow hinge within an equivalent area; thus, we expected that narrow hinge width would be a risk factor for HF, but we did not find a significant correlation between the two. Age was not significantly different in either univariate or multivariate logistic regression analysis. For sex, although it was statistically nonsignificant (p=0.146), females (F : M, OR=0.639) had a trend of fewer HFs.
Satomi et al.14) recommended using careful surgical technique to avoid HF, such as making the hinge gutter more lateral than on the open side and detaching the open side before drilling the hinge side, with frequent hinge stability checks during elevation by pushing the spinous process. Kawaguchi et al.5) suggested a 3 mm diameter drill and an acorn-type bone-cutting bit for making the gutter. In addition, we suggest meticulous screwing on the hinge side and avoiding an unnecessary wide open angle so as not to deform the hinge.
We determined the risk factors for delayed HF following plate-only open-door laminoplasty, which could be a source of axial pain or C5 palsy. Poor initial hinge status, medially placed hinge gutter, double screwed lamina, and upper cervical level seemed to be firm risk factors. Wide open angle could be a predictor as well. For successful clinical outcomes after laminoplasty, surgical and clinical precautions should be considered.
References
1. Handa Y, Kubota T, Ishii H, Sato K, Tsuchida A, Arai Y. Evaluation of prognostic factors and clinical outcome in elderly patients in whom expansive laminoplasty is performed for cervical myelopathy due to multisegmental spondylotic canal stenosis. A retrospective comparison with younger patients. J Neurosurg. 2002; 96(2 Suppl):173–179. PMID: 12450280.

2. Hirabayashi K, Satomi K. Operative procedure and results of expansive open-door laminoplasty. Spine (Phila Pa 1976). 1988; 13:870–876. PMID: 3143157.

3. Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976). 1983; 8:693–699. PMID: 6420895.

4. Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976). 1996; 21:1969–1973. PMID: 8883196.
5. Kawaguchi Y, Matsui H, Ishihara H, Gejo R, Yoshino O. Axial symptoms after en bloc cervical laminoplasty. J Spinal Disord. 1999; 12:392–395. PMID: 10549702.

6. Lee SE, Chung CK, Kim CH, Jahng TA. Symmetrically medial bony gutters for open-door laminoplasty. J Spinal Disord Tech. 2013; 26:E101–E106. PMID: 22935715.

7. Lee TT, Manzano GR, Green BA. Modified open-door cervical expansive laminoplasty for spondylotic myelopathy : operative technique, outcome, and predictors for gait improvement. J Neurosurg. 1997; 86:64–68. PMID: 8988083.

8. O'Brien MF, Peterson D, Casey AT, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine (Phila Pa 1976). 1996; 21:474–483. discussion 484. PMID: 8658252.
9. Ohnari H, Sasai K, Akagi S, Iida H, Takanori S, Kato I. Investigation of axial symptoms after cervical laminoplasty, using questionnaire survey. Spine J. 2006; 6:221–227. PMID: 16651214.

10. Park YK, Lee DY, Hur JW, Moon HJ. Delayed hinge fracture after plate-augmented, cervical open-door laminoplasty and its clinical significance. Spine J. 2014; 14:1205–1213. PMID: 24176811.

11. Rhee JM, Register B, Hamasaki T, Franklin B. Plate-only open door laminoplasty maintains stable spinal canal expansion with high rates of hinge union and no plate failures. Spine (Phila Pa 1976). 2011; 36:9–14. PMID: 21192219.

12. Roselli R, Pompucci A, Formica F, Restuccia D, Di Lazzaro V, Valeriani M, et al. Open-door laminoplasty for cervical stenotic myelopathy : surgical technique and neurophysiological monitoring. J Neurosurg. 2000; 92(1 Suppl):38–43. PMID: 10616056.

13. Sakaura H, Hosono N, Mukai Y, Ishii T, Yoshikawa H. C5 palsy after decompression surgery for cervical myelopathy : review of the literature. Spine (Phila Pa 1976). 2003; 28:2447–2451. PMID: 14595162.
14. Satomi K, Nishu Y, Kohno T, Hirabayashi K. Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976). 1994; 19:507–510. PMID: 8184342.

15. Satomi K, Ogawa J, Ishii Y, Hirabayashi K. Short-term complications and long-term results of expansive open-door laminoplasty for cervical stenotic myelopathy. Spine J. 2001; 1:26–30. PMID: 14588365.

16. Tsuji H. Laminoplasty for patients with compressive myelopathy due to so-called spinal canal stenosis in cervical and thoracic regions. Spine (Phila Pa 1976). 1982; 7:28–34. PMID: 7071659.

17. Wang MY, Shah S, Green BA. Clinical outcomes following cervical laminoplasty for 204 patients with cervical spondylotic myelopathy. Surg Neurol. 2004; 62:487–492. discussion 492-493. PMID: 15576110.

Fig. 1
Radiographic measurements of a) hinge open angle, b) hinge gutter location, c) open gutter location, and d) hinge gutter width.
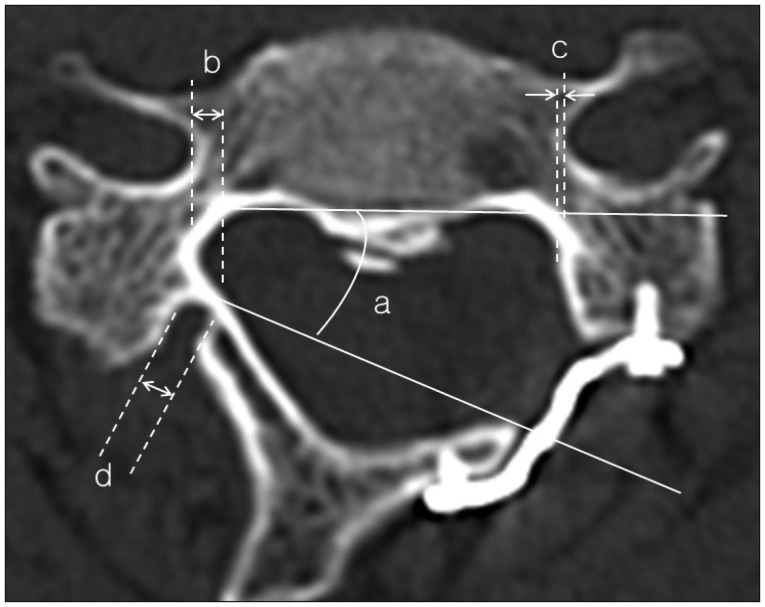
Fig. 2
CTs demonstrating representative cases. Scans were taken 1 week and 4 months postoperatively. A : Open-door laminoplasty operation at C3–6 performed on a 52-year-old female. C4 level is shown and the radiologic measurement is described. Open angle 36°, hinge location 3.5 mm, double screws, initial status d3. B : Open-door laminoplasty operation at C3–6 performed on a 66-year-old male. C6 level is shown and the radiologic measurement is described. Open angle 26°, hinge location 1.2 mm, single screw, initial status d0. Double screwed case (A) shows poor initial hinge status and an unfavorable result.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download