This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
A modified surgical technique of posterior cervical foramintomy called posterior cervical inclinatory foraminotomy (PCIF) was introduced in previous preliminary article. PCIF allows better preservation of facet joint and capsule than conventional techniques. The authors conducted a study to investigate long-term outcomes of PCIF.
Methods
We retrospectively reviewed demographic, radiologic, and clinical data from the patients who underwent PCIFs at our institution. Criteria included a minimum of 48 month follow-up and PCIFs for patients with radiculopathy from foraminal stenosis (C2–T1; single or multilevel) with persistent or recurrent root symptoms despite conservative treatment for more than 3 months. Patients who had undergone previous cervical operation were excluded. The visual analogue scale (VAS) score was used for clinical follow-up, and radiologic follow-up was performed to compare the changes of cervical sagittal alignment, focal angle and disc-space height of treated segment.
Results
The PCIFs were performed between April 2007 and March 2011 on 46 patients (32 males and 14 females) with a total of 73 levels affected. The average duration of follow-up was 74.4 months. Improvements in radiculopathic pain were seen in 39 patients (84.7%), and VAS score decreased from 6.82±1.9 to 2.19±1.9. Posterior neck pain also improved in 25 patients (71.4%) among 35 patients, and VAS score decreased from 4.97±2.0 to 2.71±1.9. The mean disc-space heights of treated segment were 5.41±1.03 mm preoperatively and decreased to 5.17±1.12 mm postoperatively. No statistically significant changes in cervical sagittal alignment, focal angle were seen during the follow-up period (Cox proportional hazards analysis and Student t-test, p>0.05).
Conclusion
The PCIF is highly effective in treating patients with cervical spondylotic radiculopathy, leading to long-lasting relief in pain. Long-term radiologic follow-up showed no significant spinal angular imbalance.
Go to :

Keywords: Cervical, Posterior, Foraminotomy, Cervical spondylosis, Radiculopathy
INTRODUCTION
Posterior surgical approach for cervical spondylotic radiculopathy was introduced in the 1960s
1020) and advanced for decades with development of equipments and techniques. In 1980s, several authors reported case series, and so-called "key-hole" laminoforaminotomy was popularized. It was proven that posterior cervical foraminotomy (PCF) was effective in managing of cervical foraminal stenosis
37813).
There are many advantages for posterior approach than anterior approach. Posterior foraminotomy is effective for spondylotic radiculopathy, easy to access, and able to avoid commonly reported complications of anterior cervical approaches such as esophageal or laryngeal nerve injury. However, some concerns about posterior cervical foraminotomy are same or adjacent segment disease, kyphosis, persistent neck pain, late recurrence.
We have reported two morphometric studies about posterior cervical foraminotomy
1214), and in 2011 we introduced a modified technique called "posterior cervical inclinatory foraminotomy (PCIF)"
4). That is different use of inclinatory drilling out for preserving more facet joint and capsule compared to conventional posterior cervical foraminotomy. In this study, we reported long-term clinical and radiological outcomes of PCIF.
Go to :

MATERIALS AND METHODS
We reviewed all medical records and radiographic images of patients who received PCIF. Between April 2007 and March 2011, total 55 patients received PCIF at our institution. 8 patients with previous cervical operation were excluded, and one patient was lost. So, 46 patients were analyzed in this study.
We examined the patients' history, and neurological exam preoperatively. Symptoms on neck pain and radiculopathy were described in visual analogue scale (VAS) score. If patients had cervical radiculopathy, they were evaluated with cervical neutral and dynamic radiographs, magnetic resonance image (MRI) and computerized tomography (CT). To determine surgical levels, some patients underwent additional exams such as diagnostic selective nerve root blocks or electromyography and nerve conduction study. As mentioned in previous preliminary article
4), operative indication is radiculopathy from foraminal stenosis (C2–T1; single or multilevel) with persistent or recurrent root symptoms despite conservative treatment for more than 3 months. And the patients with cervical disc herniation or central stenosis were excluded. Any patient didn't have motor weakness.
After surgery, we routinely followed up patients every 3 months, and annually. Patient's symptoms and cervical neutral and dynamic radiographs were routinely checked for at each follow-up visit. We measured cervical sagittal alignment, focal angle, disc-space height in preoperative and postoperative radiographs. Cervical sagittal alignment was defined by the Cobb's angle that was formed by lines parallel to inferior margin of C2 vertebral body (VB) and superior margin of C7 VB. Focal angle was defined by the angle that was formed by lines drawn at the superior margin of VB defining the disc space at the operated level and the inferior margin of the inferior VB on the neutral lateral radiographs. Disc-space heights were measured from the midpoint of the vertebra below the surgical level to the midpoint of the vertebra above the surgical level on neutral lateral radiographs. Focal angle and disc-space height were measured three times pre- and postoperatively, with the mean values used for analysis. Instability was defined as motion >2 mm at the operative segment or any adjacent segments on dynamic imaging. Kyphosis was defined as "cervical sagittal alignment" was less than 0°. All values were measured 3 times by different persons and a mean values was adopted.
Statistical analysis was performed to determine factors affecting clinical symptoms and the development of radiologic changes. All statistical analyses were performed using SPSS 20.0 for Windows (SPSS Inc., Chicago, IL, USA).
Go to :

RESULTS
The patient characteristics and preoperative details are shown in
Table 1. Long-term follow-up data were collected for 46 cases. All patients had spondylotic radiculopathy, and their corresponding lesions for foraminal stenosis in CT and MRI. The mean patients' age at operation was 60.9 years (range 42–84 years). 32 patients (69%) were men and 14 (31%) were female. Total 73 levels were affected. Most frequent levels were C5–6 (32 patients), and C6–7 (21 patients). 29 patients underwent single level PCIF, and the other 17 patients (36%) underwent PCIFs on multiple levels. The interval between operation and last follow-up ranged from 48 to 98 months (average 74.4 months).
Table 1
Demographic and preoperative details of 46 PCIF patients


Preoperatively all patients had radiculopathic pain, and 35 patients (76%) had neck pain (
Table 2). After PCIF mean VAS score of radiculopathic pain was improved from 6.82±1.9 to 2.19±1.9. Among 46 patients, 39 patients' radiculopathic pains were improved (84.7%). Mean VAS score of neck pain also was improved from 4.97±2.0 to 2.71±1.9. Among 35 patients who had neck pain, 25 patients (71.1%) experienced improvement. Both radiculopathy and neck pain decreased rapidly in early postoperative period (within 3 months), and continued afterward (
Fig. 1). Age, duration of clinical follow-up, number of surgical level, and occurrence of kyphosis were irrelevant to clinical symptom statistically.
 | Fig. 1Box and whisker plot of clinical outcomes measure by visual analogue scale (VAS). Radiculopathy and neck pain improved rapidly in early postoperative period, and maintained afterward. Box represents the first and third quartile, line inside box is median. *Outlier, more or less than interquartile range.
|
Table 2
Presenting symptoms in 46 PCIF patients


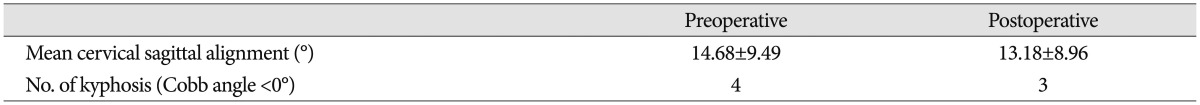
A summary of the preoperative and postoperative radiologic features at the treated level are shown in
Table 3,
4. For the measurements for angle, kyphotic alignment is indicated by a negative value and lordotic alignment is indicated by a positive value. Statistically significant change in cervical sagittal alignment or focal angle was not seen at the follow-up period. There was no significant difference at incidence of kyphosis before and after PCIF. But mean preoperative and postoperative disc-space height were 5.41±1.03 (mm) and 5.2±1.04 (mm). Disc-space height decreased steadily over this time during follow-up period (
p<0.05)(
Fig. 2). There was no relation between radiologic findings (cervical alignment, focal angle, disc-space height) and clinical symptoms statistically. Duration of follow-up did not affect radiologic changes and clinical symptoms.
 | Fig. 2Box and whisker plot of disc height index (DHI). DHI is calculated as disc-space height divided by preoperative height at treated level. DHI decreased statistically during the follow-up period (p<0.05). Box represents the first and third quartile, line inside box is median. *Outlier, more or less than interquartile range.
|
Table 3
Radiologic analysis
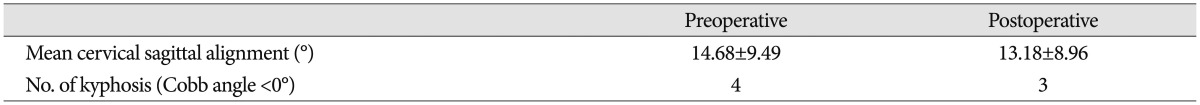

Table 4
Radiologic analysis for each level


Spondylotic radiculopathy worsened in 2 patients. In one patient who underwent C5/6 single level PCIF, recurrence occurred after 22 month. After PCIF again, symptom improved completely. And one another patients refused surgery, then symptom was improved a little after conservative treatment. A postoperative kyphosis (Cobb angle -5°) occurred in one patient who had normal cervical lordosis preoperatively, but her neck pain and radiculopathic pain improved after surgery completely. In our study, there was no other adverse event (instability, CSF leak, nerve root injury, etc.)
Go to :

DISCUSSION
First introduced in 1946 by Frykholm
10) and Scoville
19), the PCF has been an excellent surgical option of treatment for cervical radiculopathy. In comparison with anterior approaches, posterior approach has particular advantages such as ability to decompress multiple levels relatively easily, direct decompression of the involved nerve root under direct visualization, and avoidance of disc space disruption and fusion. Recent literatures have shown that PCF provides symptomatic relief in more than 90% of patients with radiculopathy refractory to nonsurgical treatment
1316).
However, traditional posterior cervical approaches have disadvantages including the risk of persistent axial pain, paraspinal muscle spasm, and postoperative instability from subperiosteal dissection detaching deep muscles, disruption of lamina and facet joint
11). And this approach also has the risk of kyphosis that may accelerate the disc degeneration
213) and symptomatic adjacent-segment and same-segment disease.
6) Jagannathan et al.
13) reported that postoperative loss of lordosis (defined as segmental Cobb angle <10°) was seen in 20% of 162 patients and postoperative instability was seen in 4.9%. Clarke et al.
6) reported that symptomatic adjacent-segment disease and same-segment disease developed in 4.9% and 3.3% retrospectively among 303 patients underwent PCF. In a study for long-term follow-up of PCF, reoperation rate increased over time and reached 24.3% in patients with follow-up periods longer than 10 years due to adjacent-segment disease. These results suggest that traditional PCF may affect stability of treated levels.
To overcome the disadvantages, posterior cervical approaches have advanced to minimally invasive technique under microscope or endoscope
19). Kwon
15) reported that minimally invasive PCF using tubular retractors showed successful surgical effects for cervical radiculopathy and yielded less postoperative kyphosis and axial pain. In a prospective study, 88% of patients no longer had arm pain, and no operation-induced neck pain or instabilities occurred
18). These studies suggest that attempt to minimize posterior cervical structures could reduce postoperative complications of PCF.
We tried to minimize not only paraspinal muscles, but also posterior cervical bony structures, especially facet joints. Several studies reported facet joint violation can cause segmental hypermobility, especially when resected more than 50%
51722). Our PCIF technique can provide adequate decompression with preserving more posterior aspect of the facet joint and capsule. In our study, PCIF had similar improvement rate of radiculopathy and lower complication rate (postoperative kyphosis, persistent axial pain) compared to other studies of PCF. Comparing to a research of Jagannathan et al.
13), the extent of decrease in our study was a little less than that of a conventional PCF, but it was more than age-related changes
21). Disc-height changes were irrelevant to clinical symptoms and loss of lordosis, so we are hard to believe that PCIF affects same-level instability and degeneration. Longer follow-up of this research is needed why disc-height changed.
In preliminary study, we presumed that minimal facet and capsule resection would reduce the complication of PCF. This research showed a favorable outcome at 5-year follow-up. However the periods of studies about traditional PCF usually lasted longer than 10 years, these studies reported that complication rate increased as time passed. Further long-term studies are necessary in order to compared to traditional PCF.
Go to :

CONCLUSION
This study showed that PCIF can be more safe and efficient method to treat cervical spondylotic radiculopathy. Long-term radiologic and clinical results of PCIF suggest that less invasive techniques provide less complications, and no significant spinal angular imbalance.
Go to :

Acknowledgements
This work was supported by research grant from a Pohang SM Christianity Hospital.
Go to :

References
1. Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy : results of a new technique in 100 cases. J Neurosurg. 2001; 95(1 Suppl):51–57. PMID:
11453432.

2. Cağlar YS, Bozkurt M, Kahilogullari G, Tuna H, Bakir A, Torun F, et al. Keyhole approach for posterior cervical discectomy : experience on 84 patients. Minim Invasive Neurosurg. 2007; 50:7–11. PMID:
17546536.

3. Casotto A, Buoncristiani P. Posterior approach in cervical spondylotic myeloradiculopathy. Acta Neurochir (Wien). 1981; 57:275–285. PMID:
7282449.

4. Chang JC, Park HK, Choi SK. Posterior cervical inclinatory foraminotomy for spondylotic radiculopathy preliminary. J Korean Neurosurg Soc. 2011; 49:308–313. PMID:
21716632.

5. Chen BH, Natarajan RN, An HS, Andersson GB. Comparison of biomechanical response to surgical procedures used for cervical radiculopathy : posterior keyhole foraminotomy versus anterior foraminotomy and discectomy versus anterior discectomy with fusion. J Spinal Disord. 2001; 14:17–20. PMID:
11242270.

6. Clarke MJ, Ecker RD, Krauss WE, McClelland RL, Dekutoski MB. Same-segment and adjacent-segment disease following posterior cervical foraminotomy. J Neurosurg Spine. 2007; 6:5–9. PMID:
17233284.

7. Epstein JA, Janin Y, Carras R, Lavine LS. A comparative study of the treatment of cervical spondylotic myeloradiculopathy. Experience with 50 cases treated by means of extensive laminectomy, foraminotomy, and excision of osteophytes during the past 10 years. Acta Neurochir (Wien). 1982; 61:89–104. PMID:
6280455.

8. Fager CA. Posterolateral approach to ruptured median and paramedian cervical disk. Surg Neurol. 1983; 20:443–452. PMID:
6648783.

9. Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy : an initial clinical experience. Neurosurgery. 2002; 51(5 Suppl):S37–S45. PMID:
12234428.
10. Frykholm R. Lower cervical vertebrae and intervertebral discs; surgical anatomy and pathology. Acta Chir Scand. 1951; 101:345–359. PMID:
14868335.
11. Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976). 1996; 21:1969–1973. PMID:
8883196.
12. Hwang JC, Bae HG, Cho SW, Cho SJ, Park HK, Chang JC. Morphometric study of the nerve roots around the lateral mass for posterior foraminotomy. J Korean Neurosurg Soc. 2010; 47:358–364. PMID:
20539795.

13. Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease : a single-surgeon experience with a minimum of 5 years' clinical and radiographic follow-up. J Neurosurg Spine. 2009; 10:347–356. PMID:
19441994.

14. Kim JH, Lee CW, Chun KS, Shin WH, Bae HG, Chang JC. Morphometric relationship between the cervicothoracic cord segments and vertebral bodies. J Korean Neurosurg Soc. 2012; 52:384–390. PMID:
23133729.

15. Kwon YJ. Long-term clinical and radiologic outcomes of minimally invasive posterior cervical foraminotomy. J Korean Neurosurg Soc. 2014; 56:224–229. PMID:
25368765.

16. McAnany SJ, Kim JS, Overley SC, Baird EO, Anderson PA, Qureshi SA. A meta-analysis of cervical foraminotomy : open versus minimally-invasive techniques. Spine J. 2015; 15:849–856. PMID:
25623079.

17. Raynor RB, Pugh J, Shapiro I. Cervical facetectomy and its effect on spine strength. J Neurosurg. 1985; 63:278–282. PMID:
4020449.

18. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes : a prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008; 33:940–948. PMID:
18427313.

19. Scoville WB. Types of cervical disk lesions and their surgical approaches. JAMA. 1966; 196:479–481. PMID:
5952348.

20. Scoville WB, Whitcomb BB, McLaurin R. The cervical ruptured disc; report of 115 operative cases. Trans Am Neurol Assoc. 1951; 56:222–224. PMID:
14913631.
21. Yukawa Y, Kato F, Suda K, Yamagata M, Ueta T. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I : Radiographic data from over 1,200 asymptomatic subjects. Eur Spine J. 2012; 21:1492–1498. PMID:
22310883.

22. Zdeblick TA, Zou D, Warden KE, McCabe R, Kunz D, Vanderby R. Cervical stability after foraminotomy. A biomechanical in vitro analysis. J Bone Joint Surg Am. 1992; 74:22–27. PMID:
1734010.

Go to :







 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download