1. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; 368:893–903. PMID:
23390923.

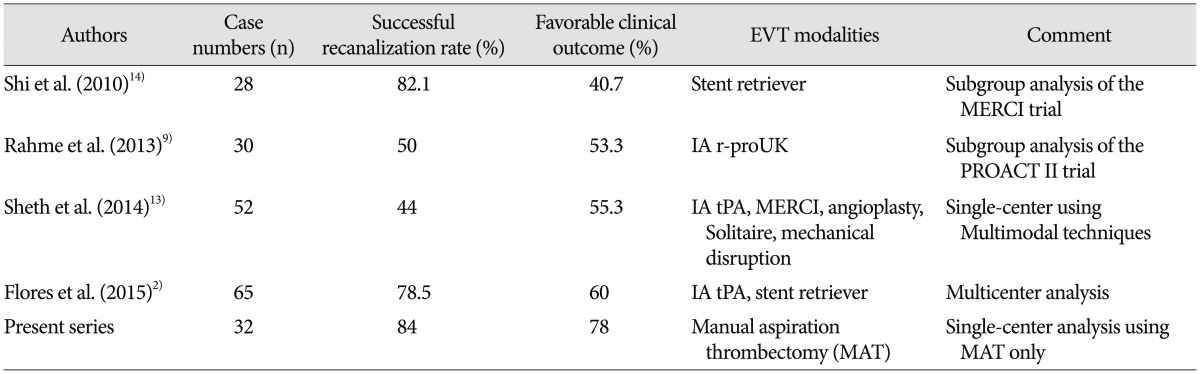
2. Flores A, Tomasello A, Cardona P, de Miquel MA, Gomis M, Garcia Bermejo P, et al. Endovascular treatment for M2 occlusions in the era of stentrievers : a descriptive multicenter experience. J Neurointerv Surg. 2015; 7:234–237. PMID:
24578483.

3. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329. PMID:
18815396.

4. IMS II Trial Investigators. The Interventional Management of Stroke (IMS) II Study. Stroke. 2007; 38:2127–2135. PMID:
17525387.
5. Jankowitz B, Aghaebrahim A, Zirra A, Spataru O, Zaidi S, Jumaa M, et al. Manual aspiration thrombectomy : adjunctive endovascular recanalization technique in acute stroke interventions. Stroke. 2012; 43:1408–1411. PMID:
22382156.
6. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct thrombus retrieval using the reperfusion catheter of the penumbra system : forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol. 2011; 32:283–287. PMID:
21087940.

7. Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2) : a randomised trial. Lancet. 2012; 380:1231–1240. PMID:
22932714.

8. Pereira VM, Gralla J, Davalos A, Bonafé A, Castaño C, Chapot R, et al. Prospective, multicenter, single-arm study of mechanical thrombectomy using Solitaire Flow Restoration in acute ischemic stroke. Stroke. 2013; 44:2802–2807. PMID:
23908066.

9. Rahme R, Abruzzo TA, Martin RH, Tomsick TA, Ringer AJ, Furlan AJ, et al. Is intra-arterial thrombolysis beneficial for M2 occlusions? Subgroup analysis of the PROACT-II trial. Stroke. 2013; 44:240–242. PMID:
23223507.

10. Rahme R, Yeatts SD, Abruzzo TA, Jimenez L, Fan L, Tomsick TA, et al. Early reperfusion and clinical outcomes in patients with M2 occlusion : pooled analysis of the PROACT II, IMS, and IMS II studies. J Neurosurg. 2014; 121:1354–1358. PMID:
25259569.

11. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome : a meta-analysis. Stroke. 2007; 38:967–973. PMID:
17272772.

12. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT) : a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 380:1241–1249. PMID:
22932715.

13. Sheth SA, Yoo B, Saver JL, Starkman S, Ali LK, Kim D, et al. M2 occlusions as targets for endovascular therapy : comprehensive analysis of diffusion/perfusion MRI, angiography, and clinical outcomes. J Neurointerv Surg. 2015; 7:478–483. PMID:
24821842.

14. Shi ZS, Loh Y, Walker G, Duckwiler GR. MERCI and Multi-MERCI Investigators. Clinical outcomes in middle cerebral artery trunk occlusions versus secondary division occlusions after mechanical thrombectomy : pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI trials. Stroke. 2010; 41:953–960. PMID:
20378867.

15. Tomsick T, Broderick J, Carrozella J, Khatri P, Hill M, Palesch Y, et al. Revascularization results in the Interventional Management of Stroke II trial. AJNR Am J Neuroradiol. 2008; 29:582–587. PMID:
18337393.

16. Turk AS, Spiotta A, Frei D, Mocco J, Baxter B, Fiorella D, et al. Initial clinical experience with the ADAPT technique : a direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2014; 6:231–237. PMID:
23624315.

17. Wolpert SM, Bruckmann H, Greenlee R, Wechsler L, Pessin MS, del Zoppo GJ. Neuroradiologic evaluation of patients with acute stroke treated with recombinant tissue plasminogen activator. The rt-PA Acute Stroke Study Group. AJNR Am J Neuroradiol. 1993; 14:3–13. PMID:
8427107.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download