Abstract
Intracranial tuberculous subdural empyema (ITSE) is extremely rare. To our knowledge, only four cases of microbiologically confirmed ITSE have been reported in the English literature to date. Most cases have arisen in patients with pulmonary tuberculosis regardless of trauma. A 46-year-old man presented to the emergency department after a fall. On arrival, he complained of pain in his head, face, chest and left arm. He was alert and oriented. An initial neurological examination was normal. Radiologic evaluation revealed multiple fractures of his skull, ribs, left scapula and radius. Though he had suffered extensive skull fractures of his cranium, maxilla, zygoma and orbital wall, the sustained cerebral contusion and hemorrhage were mild. Eighteen days later, he suddenly experienced a general tonic-clonic seizure. Radiologic evaluation revealed a subdural empyema in the left occipital area that was not present on admission. We performed a craniotomy, and the empyema was completely removed. Microbiological examination identified Mycobacterium tuberculosis (M. tuberculosis). After eighteen months of anti-tuberculous treatment, the empyema disappeared completely. This case demonstrates that tuberculosis can induce empyema in patients with skull fractures. Thus, we recommend that M. tuberculosis should be considered as the probable pathogen in cases with posttraumatic empyema.
Subdural empyema is a rare intracranial infection that usually arises as a complication of meningitis in infants and young children and as a complication of paranasal sinusitis, otitis media, or mastoiditis in older children and adults3611). The organism responsible for a subdural empyema depends on the origin of the infection3). Aerobic and anaerobic streptococci, Haemophilus influenzae, Staphylococcus aureus, and Staphylococcus epidermidis are the most commonly identified organisms3). Mycobacterium tuberculosis (M.tuberculosis) is an extremely rare pathogen in subdural empyema231112). To date, only four cases of microbiologically confirmed intracranial tuberculous subdural empyema (ITSE) have been reported in the English literature231112).
Neurotuberculosis constitutes approximately 5–15% of all cases of extra-pulmonary tuberculosis157). Although tuberculous meningitis and parenchymal granulomas cause most cases of intracranial neurotuberculosis135712), ITSE is an extremely rare condition23111213). Most of the cases have been associated with pulmonary tuberculosis, which was thought to be the origin of hematogenous dissemination2312).
To our knowledge, posttraumatic ITSE with skull fracture has not yet been reported. Our patient experienced a tuberculous empyema after a head trauma that resulted in skull fracture. Although an inactive pulmonary tuberculous lesion was identified on his chest computed tomography (CT) scan, there was no subdural empyema immediately after the skull fracture. Therefore, our case is unique among the previously reported cases because the skull fracture may have affected the occurrence of ITSE.
A 46-year-old man presented to the emergency department with head trauma. He had sustained a fall while working at an approximately 6-meter-high location. Upon arrival at our hospital, he complained of severe pain in his head, face, chest, and left arm. He was alert and oriented, and the initial neurological examination was normal. Although there were some abrasions, he had no lacerations or deep wounds on his head and face. CT scan revealed multiple fractures involving his skull, facial bones, ribs, left scapula and left distal radius. Although the skull and facial bone fractures were extensive in the left fronto-temporal cranium, left maxilla, left zygoma and left orbital wall, the cerebral contusion and intracranial hemorrhage were mild (Fig. 1). Although there was pneumocephalus in the left frontal area, he did not experience cerebrospinal fluid (CSF) rhinorrhea. We performed conservative management after inserting a chest tube to drain the hemothorax.
Eighteen days later, he suddenly experienced a general tonic-clonic seizure. The follow-up brain CT scan revealed fluid collection in the left fronto-temporal skull fracture site and in the left occipital area that had not been present on admission (Fig. 2A). Magnetic resonance imaging (MRI) demonstrated strong enhancement of the dura mater surrounding the left occipital fluid collection, and the fluid was suspected to be a subdural empyema (Fig. 2B).
We performed a craniotomy, and both the left fronto-temporal fluid collection and the left occipital subdural empyema were completely removed. The occipital empyema was thick and dark brownish, making it distinct from the clear fluid in the left fronto-temporal area. There was no traumatic lesion in the occipital area, whereas multiple dural tears were found intraoperatively at the left fronto-temporal skull fracture site.
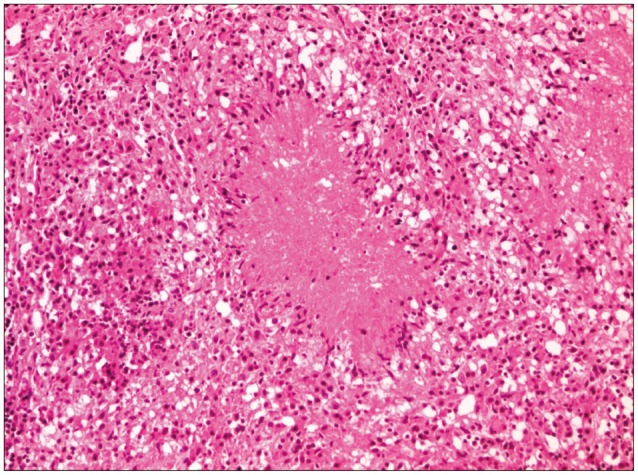
Polymerase chain reaction (PCR) analysis confirmed M. tuberculosis in the empyema. The histopathological examination produced the same result, showing multifocal granulomatous inflammation with extensive caseous necrosis and some acid-fast bacilli (AFB) (Fig. 3). Only M. tuberculosis bacilli were identified without co-infection with other microorganisms. Our patient denied any previous history of tuberculosis elsewhere in his body and presented no clinical evidence of pulmonary tuberculosis. Moreover, sputum AFB stain, culture and PCR tests were all negative. However, we found calcified nodules on a chest CT scan, suggesting inactive tuberculosis.
We administered anti-tuberculous treatment for eighteen months. A follow-up MRI performed six months later showed the complete disappearance of the subdural empyema (Fig. 4).
Most cases of ITSE are closely related to pulmonary tuberculosis. To our knowledge, four cases of ITSE have been published thus far231112). Two of them had pulmonary tuberculosis, which was thought to be the origin of the neurotuberculosis312). Another one of the cases had a history of exposure to an active case of pulmonary tuberculosis2). Whereas only one-third of tuberculous brain abscesses are accompanied by pulmonary tuberculosis1), ITSE seems to be associated more frequently with a pulmonary focus.
Cayli et al.3) reported a 1-year-old boy with ITSE whose infection resulted from hematogenous dissemination of tuberculous bacilli from the primary lesion in the lung. van Dellen et al.12) described ITSE that started as tuberculous osteitis of the cranium, which had originated from pulmonary tuberculosis. Despite a 5-year history of treatment for pulmonary tuberculosis, he had poor compliance in maintaining anti-tuberculous treatment. It is the only case of ITSE that arose in the adult population. Banerjee et al.2) also reported a 12-year-old boy with ITSE. Although the presence of pulmonary tuberculosis was not described, he had a history of exposure to an active case of pulmonary tuberculosis (his father)2). Long-term exposure to pulmonary tuberculosis is likely to cause the inhalation of aerosolized droplets contaminated with tuberculous bacilli. Thus, the hematogenous dissemination of tuberculous bacilli from the lung to the subdural space was considered the probable pathogenic process of his ITSE.
Our patient had inactive pulmonary tuberculosis that was identifiable on chest CT scan, although the sputum AFB culture and PCR test were negative. However, we are not sure that his pulmonary tuberculosis was the source of the subdural empyema as in the aforementioned cases. Although his latent pulmonary lesion may be the source of the empyema, it is very difficult to explain what caused the inactive pulmonary tuberculosis to become active immediately after he sustained the skull fracture. Moreover, the subdural empyema was not present on the initial brain CT scan performed immediately after the trauma, but it was easily detected eighteen days later (Fig. 1B, 2A). Therefore, we believe that the empyema arose after the head trauma, and the effects of the pulmonary tuberculosis were very limited in our ITSE case. We think that the trauma and the resultant skull fracture must have facilitated the development of a subdural empyema by destroying physiological barriers such as the dura, arachnoid or blood-brain barrier, offering the pathogen an entry point. We also believe that the basal skull fracture caused pathologic communication between the cranial cavity and the open air, as evidenced by the pneumocephalus detected on CT scan. Moreover, several dural tears were identified intraoperatively. The dura is an effective barrier to the contiguous spread of all infections212); therefore, the dural tears in our case might have allowed the bacilli to pass into the subdural space and facilitated direct subdural spreading.
Basal skull fractures are closely associated with meningitis with or without CSF leakage8910). The reported incidence of meningitis following basal skull fracture varies from 0.4 to 17.8%9). Dural tears are common because of the firm adherence of the dura to the cranial base8), and CSF rhinorrhea is present in less than 10% of cases with anterior fossa fractures9). Our patient had multiple fractures in the anterior skull base and temporal cranium. In addition, several dural tears were identified intraoperatively near the fracture site. Although our patient had pneumocephalus on the initial CT scan, CSF leakage was not observed.
Meningitis may also occur in the absence of an apparent CSF leak8). The reason is unclear, but it may be related to the intermittent nature of CSF leakage or its spontaneous remission8). Eftekhar et al.4) noted that pneumocephalus significantly increases the risk of meningitis and should therefore be considered equivalent to CSF leakage. Additionally, Scholsem et al.8) recommended surgical repair for an enlarging pneumocephalus and CSF leakage. However, most of the available information about posttraumatic meningitis is mainly for bacterial infections. There is a paucity of literature about tuberculous meningitis that stems from its rarity, although tuberculous meningitis shares some characteristics with bacterial meningitis. We believe that the current case is an important addition to the literature on ITSE, whose clinical characteristics have not yet been elucidated.
M. tuberculosis is notoriously difficult to culture, particularly after treatment has been initiated12). In our case, the AFB culture was negative even though anti-tuberculous treatment had not yet been commenced. Although we failed to culture M. tuberculosis, the diagnosis was confirmed by a PCR test and histopathological examination. Some authors have reported co-infections of tuberculosis with other pathogens such as Staphylococcus aureus in their ITSE cases1112). However, we did not identify any other pathogens by culturing except M. tuberculosis. Therefore, we are sure that the subdural empyema stemmed entirely from M. tuberculosis without the involvement of other bacterial pathogens.
Some physicians recommend the initiation of anti-tuberculous treatment on an empirical basis, even in the absence of laboratory confirmation of the diagnosis, if neurotuberculosis is suspected12). With the advent of human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome, more cases of neurotuberculosis are being diagnosed1). However, our patient was immunocompetent, HIV negative and had no other general risk factors for infection. Thus, we did not suspect tuberculous empyema because it was too rare to be included in a differential diagnosis.
Our patient experienced a tuberculous empyema after head trauma that resulted in a skull fracture. Our case is very unique in that M. tuberculosis caused a subdural empyema in a patient who had a skull fracture after head trauma. We recommend that M. tuberculosis should be considered as a likely pathogen in posttraumatic empyema in patients with skull fractures.
References
1. Ansari MK, Jha S. Tuberculous brain abscess in an immunocompetent adolescent. J Nat Sci Biol Med. 2014; 5:170–172. PMID: 24678219.

2. Banerjee AD, Pandey P, Ambekar S, Chandramouli BA. Pediatric intracranial subdural empyema caused by Mycobacterium tuberculosis--a case report and review of literature. Childs Nerv Syst. 2010; 26:1117–1120. PMID: 20437243.

3. Cayli SR, Onal C, Koçak A, Onmuş SH, Tekiner A. An unusual presentation of neurotuberculosis: subdural empyema. Case report. J Neurosurg. 2001; 94:988–991. PMID: 11409530.
4. Eftekhar B, Ghodsi M, Nejat F, Ketabchi E, Esmaeeli B. Prophylactic administration of ceftriaxone for the prevention of meningitis after traumatic pneumocephalus: results of a clinical trial. J Neurosurg. 2004; 101:757–761. PMID: 15540912.

5. Katti MK. Pathogenesis, diagnosis, treatment, and outcome aspects of cerebral tuberculosis. Med Sci Monit. 2004; 10:RA215–RA229. PMID: 15328498.
6. Lee SK, Kim SW. Fatal subdural empyema following pyogenic meningitis. J Korean Neurosurg Soc. 2011; 49:175–177. PMID: 21556239.

7. Madhavan K, Widi G, Shah A, Petito C, Gallo BV, Komotar RJ. Tuberculoma of the brain with unknown primary infection in an immunocompetent host. J Clin Neurosci. 2012; 19:1320–1322. PMID: 22727748.

8. Scholsem M, Scholtes F, Collignon F, Robe P, Dubuisson A, Kaschten B, et al. Surgical management of anterior cranial base fractures with cerebrospinal fluid fistulae: a single-institution experience. Neurosurgery. 2008; 62:463–439. discussion 469-471. PMID: 18382325.
9. Servais L, Fonteyne C, Christophe C, Prudhon V, Brihaye P, Biarent D, et al. Meningitis following basal skull fracture in two in-line skaters. Childs Nerv Syst. 2005; 21:339–342. PMID: 15798922.

10. Sonig A, Thakur JD, Chittiboina P, Khan IS, Nanda A. Is posttraumatic cerebrospinal fluid fistula a predictor of posttraumatic meningitis? A US Nationwide Inpatient Sample database study. Neurosurg Focus. 2012; 32:E4. PMID: 22655693.

11. Turel MK, Moorthy RK, Rajshekhar V. Multidrug-resistant tuberculous subdural empyema with secondary methicillin-resistant Staphylococcus aureus infection: an unusual presentation of cranial tuberculosis in an infant. Neurol India. 2012; 60:231–234. PMID: 22626710.

12. van Dellen A, Nadvi SS, Nathoo N, Ramdial PK. Intracranial tuberculous subdural empyema: case report. Neurosurgery. 1998; 43:370–373. PMID: 9696093.

13. Vijayakumar B, Sarin K, Mohan G. Tuberculous brain abscess and subdural empyema in an immunocompetent child: significance of AFB staining in aspirated pus. Ann Indian Acad Neurol. 2012; 15:130–133. PMID: 22566728.

Fig. 1
Brain CT scan performed on the first day shows a skull fracture (A) and minimal cerebral contusion and intracranial hemorrhage (B).
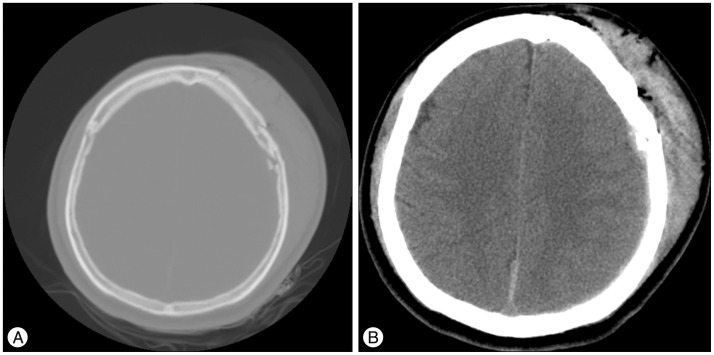
Fig. 2
A: Preoperative brain CT scan performed on the eighteenth day shows left fronto-temporal and left occipital fluid collections. B: Preoperative axial MRI, T1-weighted gadolinium-enhanced images shows the empyema in the left occipital region.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download