1. Akeson WH, Massie JB, Huang B, Giurea A, Sah R, Garfin SR, et al. Topical high-molecular-weight hyaluronan and a roofing barrier sheet equally inhibit postlaminectomy fibrosis. Spine J. 2005; 5:180–190. PMID:
15749618.

2. Alkalay RN, Kim DH, Urry DW, Xu J, Parker TM, Glazer PA. Prevention of postlaminectomy epidural fibrosis using bioelastic materials. Spine (Phila Pa 1976). 2003; 28:1659–1665. PMID:
12897488.

3. Asch HL, Lewis PJ, Moreland DB, Egnatchik JG, Yu YJ, Clabeaux DE, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm. J Neurosurg. 2002; 96(1 Suppl):34–44. PMID:
11795712.

4. Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, et al. The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine (Phila Pa 1976). 1996; 21:1777–1186. PMID:
8855462.
5. Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, et al. The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine (Phila Pa 1976). 1996; 21:1787–1794. discussion 1794-1795. PMID:
8855463.
6. Bryant MS, Bremer AM, Nguyen TQ. Autogeneic fat transplants in the epidural space in routine lumbar spine surgery. Neurosurgery. 1983; 13:367–370. PMID:
6633828.

7. Cauchoix J, Ficat C, Girard B. Repeat surgery after disc excision. Spine (Phila Pa 1976). 1978; 3:256–259. PMID:
152469.

8. Choi MY, Auh SJ, Choi DG, Chang BL. Effect of ADCON-L on adjustable strabismus surgery in rabbits. Br J Ophthalmol. 2001; 85:80–84. PMID:
11133717.

9. Diamond MP, Wexner SD, diZereg GS, Korell M, Zmora O, Van Goor H, et al. Adhesion prevention and reduction : current status and future recommendations of a multinational interdisciplinary consensus conference. Surg Innov. 2010; 17:183–188. PMID:
20798093.

10. DiFazio FA, Nichols JB, Pope MH, Frymoyer JW. The use of expanded polytetrafluoroethylene as an interpositional membrane after lumbar laminectomy. Spine (Phila Pa 1976). 1995; 20:986–991. PMID:
7631246.

11. Einhaus SL, Robertson JT, Dohan FC Jr, Wujek JR, Ahmad S. Reduction of peridural fibrosis after lumbar laminotomy and discectomy in dogs by a resorbable gel (ADCON-L). Spine (Phila Pa 1976). 1997; 22:1440–1446. discussion 1446-1447. PMID:
9231961.

12. Foulkes GD, Robinson JS Jr. Intraoperative dexamethasone irrigation in lumbar microdiskectomy. Clin Orthop Relat Res. 1990; (261):224–228. PMID:
2245548.

13. Ganzer D, Giese K, Völker L, Pietzner U, Follak N, Merk H. Two-year results after lumbar microdiscectomy with and without prophylaxis of a peridural fibrosis using Adcon-L. Arch Orthop Trauma Surg. 2003; 123:17–21. PMID:
12582791.

14. Gerszten PC, Moossy JJ, Bahri S, Kalend A, Martínez AJ. Inhibition of peridural fibrosis after laminectomy using low-dose external beam radiation in a rat model. Neurosurgery. 1999; 44:597–602. discussion 602-603. PMID:
10069597.

15. Gill GG, Sakovich L, Thompson E. Pedicle fat grafts for the prevention of scar formation after laminectomy. An experimental study in dogs. Spine (Phila Pa 1976). 1979; 4:176–186. PMID:
264034.

16. Hellebrekers BW, Trimbos-Kemper TC, Trimbos JB, Emeis JJ, Kooistra T. Use of fibrinolytic agents in the prevention of postoperative adhesion formation. Fertil Steril. 2000; 74:203–212. PMID:
10927033.

17. Hinton JL Jr, Warejcka DJ, Mei Y, McLendon RE, Laurencin C, Lucas PA, et al. Inhibition of epidural scar formation after lumbar laminectomy in the rat. Spine (Phila Pa 1976). 1995; 20:564–570. discussion 579-580. PMID:
7604326.

18. Hong JH, Choe JW, Kwon GY, Cho DY, Sohn DS, Kim SW, et al. The effects of barrier materials on reduction of pericardial adhesion formation in rabbits : a comparative study of a hyaluronan-based solution and a temperature sensitive poloxamer solution/gel material. J Surg Res. 2011; 166:206–213. PMID:
21035131.

19. Jiang ZL, Fletcher NM, Diamond MP, Abu-Soud HM, Saed GM. Hypoxia regulates iNOS expression in human normal peritoneal and adhesion fibroblasts through nuclear factor kappa B activation mechanism. Fertil Steril. 2009; 91:616–621. PMID:
18281043.

20. Jönsson B, Strömqvist B. Repeat decompression of lumbar nerve roots. A prospective two-year evaluation. J Bone Joint Surg Br. 1993; 75:894–897. PMID:
8245078.
21. Kato T, Haro H, Komori H, Shinomiya K. Evaluation of hyaluronic acid sheet for the prevention of postlaminectomy adhesions. Spine J. 2005; 5:479–488. PMID:
16153573.

22. Key JA, Ford LT. Experimental intervertebral-disc lesions. J Bone Joint Surg Am. 1948; 30A:621–630. PMID:
18099522.

23. Kim DW, Chun HJ, Lee SK. Percutaneous needle puncture technique to create a rabbit model with traumatic degenerative disk disease. World Neurosurg. 2015; 84:438–445. PMID:
25886720.

24. Kim SS, Michelsen CB. Revision surgery for failed back surgery syndrome. Spine (Phila Pa 1976). 1992; 17:957–960. PMID:
1387978.

25. Kwon SW, Lim SH, Lee YW, Lee YG, Chu BY, Lee JH, et al. Anti-adhesive effect of poloxamer/alginate/CaCl2 mixture in the rat model. J Korean Surg Soc. 2006; 71:280–287.
26. LaRocca H, Macnab I. The laminectomy membrane. Studies in its evolution, characteristics, effects and prophylaxis in dogs. J Bone Joint Surg Br. 1974; 56B:545–550. PMID:
4421702.
27. Liakakos T, Thomakos N, Fine PM, Dervenis C, Young RL. Peritoneal adhesions : etiology, pathophysiology, and clinical significance. Recent advances in prevention and management. Dig Surg. 2001; 18:260–273. PMID:
11528133.

28. Liu S, Boutrand JP, Bittoun J, Tadie M. A collagen-based sealant to prevent in vivo reformation of epidural scar adhesions in an adult rat laminectomy model. J Neurosurg. 2002; 97(1 Suppl):69–74. PMID:
12120654.

29. Massie JB, Schimizzi AL, Huang B, Kim CW, Garfin SR, Akeson WH. Topical high molecular weight hyaluronan reduces radicular pain post laminectomy in a rat model. Spine J. 2005; 5:494–502. PMID:
16153575.

30. Nagakura T, Hirata H, Tsujii M, Sugimoto T, Miyamoto K, Horiuchi T, et al. Effect of viscous injectable pure alginate sol on cultured fibroblasts. Plast Reconstr Surg. 2005; 116:831–838. PMID:
16141823.

31. Neel HB 3rd. Implants of Gore-Tex. Arch Otolaryngol. 1983; 109:427–433. PMID:
6860217.
32. North RB, Campbell JN, James CS, Conover-Walker MK, Wang H, Piantadosi S, et al. Failed back surgery syndrome : 5-year follow-up in 102 patients undergoing repeated operation. Neurosurgery. 1991; 28:685–690. discussion 690-691. PMID:
1831546.
33. Oh SH, Kim JK, Song KS, Noh SM, Ghil SH, Yuk SH, et al. Prevention of postsurgical tissue adhesion by anti-inflammatory drug-loaded pluronic mixtures with sol-gel transition behavior. J Biomed Mater Res A. 2005; 72:306–316. PMID:
15654699.

34. Park JH, Jeong SH, Lee YJ, Choi SK, Hong SC, Jung EJ, et al. Current status of the use of antiadhesive agents for gastric cancer surgery : a questionnaire survey in South Korea. J Korean Surg Soc. 2013; 84:160–167. PMID:
23487148.

35. Park JS, Cha SJ, Kim BG, Choi YS, Kwon GY, Kang H, et al. An assessment of the effects of a hyaluronan-based solution on reduction of postsurgical adhesion formation in rats : a comparative study of hyaluronan-based solution and two film barriers. J Surg Res. 2011; 168:49–55. PMID:
20036381.

36. Park SO, Han J, Minn KW, Jin US. Prevention of capsular contracture with Guardix-SG (®) after silicone implant insertion. Aesthetic Plast Surg. 2013; 37:543–548. PMID:
23456146.

37. Reigel DH, Bazmi B, Shih SR, Marquardt MD. A pilot investigation of poloxamer 407 for the prevention of leptomeningeal adhesions in the rabbit. Pediatr Neurosurg. 1993; 19:250–255. PMID:
8398849.

38. Ross JS, Robertson JT, Frederickson RC, Petrie JL, Obuchowski N, Modic MT, et al. Association between peridural scar and recurrent radicular pain after lumbar discectomy : magnetic resonance evaluation. ADCON-L European Study Group. Neurosurgery. 1996; 38:855–861. discussion 861-863. PMID:
8692415.
39. Rout UK, Saed GM, Diamond MP. Expression pattern and regulation of genes differ between fibroblasts of adhesion and normal human peritoneum. Reprod Biol Endocrinol. 2005; 3:1. PMID:
15642115.
40. Saed GM, Diamond MP. Modulation of the expression of tissue plasminogen activator and its inhibitor by hypoxia in human peritoneal and adhesion fibroblasts. Fertil Steril. 2003; 79:164–168. PMID:
12524082.

41. Seifer DB, Diamond MP, DeCherney AH. An appraisal of barrier agents in the reduction of adhesion formation following surgery. J Gynecol Surg. 1990; 6:3–10. PMID:
10149754.

42. Shih HN, Fang JF, Chen JH, Yang CL, Chen YH, Sung TH, et al. Reduction in experimental peridural adhesion with the use of a crosslinked hyaluronate/collagen membrane. J Biomed Mater Res B Appl Biomater. 2004; 71:421–428. PMID:
15389509.

43. Shim HS, Lee YW, Lee YM, Oh YH, Kwon SW, Kim JH, et al. Evaluation of resorbable materials for preventing surgical adhesion on rat experiment. J Korean Surg Soc. 2002; 63:179–186.
44. Songer MN, Ghosh L, Spencer DL. Effects of sodium hyaluronate on peridural fibrosis after lumbar laminotomy and discectomy. Spine (Phila Pa 1976). 1990; 15:550–554. PMID:
2402695.

45. Songer MN, Rauschning W, Carson EW, Pandit SM. Analysis of peridural scar formation and its prevention after lumbar laminotomy and discectomy in dogs. Spine (Phila Pa 1976). 1995; 20:571–580. discussion 579-580. PMID:
7604327.

46. Temel SG, Ozturk C, Temiz A, Ersozlu S, Aydinli U. A new material for prevention of epidural fibrosis after laminectomy : oxidized regenerated cellulose (interceed), an absorbable barrier. J Spinal Disord Tech. 2006; 19:270–275. PMID:
16778662.
47. Ward BC, Panitch A. Abdominal adhesions : current and novel therapies. J Surg Res. 2011; 165:91–111. PMID:
20036389.
48. Welch WC, Thomas KA, Cornwall GB, Gerszten PC, Toth JM, Nemoto EM, et al. Use of polylactide resorbable film as an adhesion barrier. J Neurosurg. 2002; 97(4 Suppl):413–422. PMID:
12449195.

49. Yong-Hing K, Reilly J, de Korompay V, Kirkaldy-Willis WH. Prevention of nerve root adhesions after laminectomy. Spine (Phila Pa 1976). 1980; 5:59–64. PMID:
7361199.

50. Young RL, Cota J, Zund G, Mason BA, Wheeler JM. The use of an amniotic membrane graft to prevent postoperative adhesions. Fertil Steril. 1991; 55:624–628. PMID:
2001762.

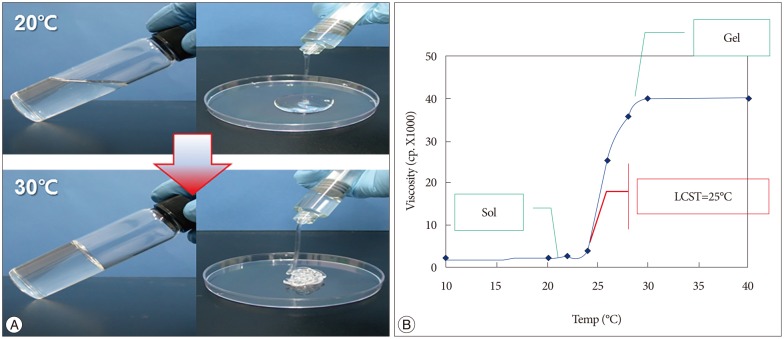
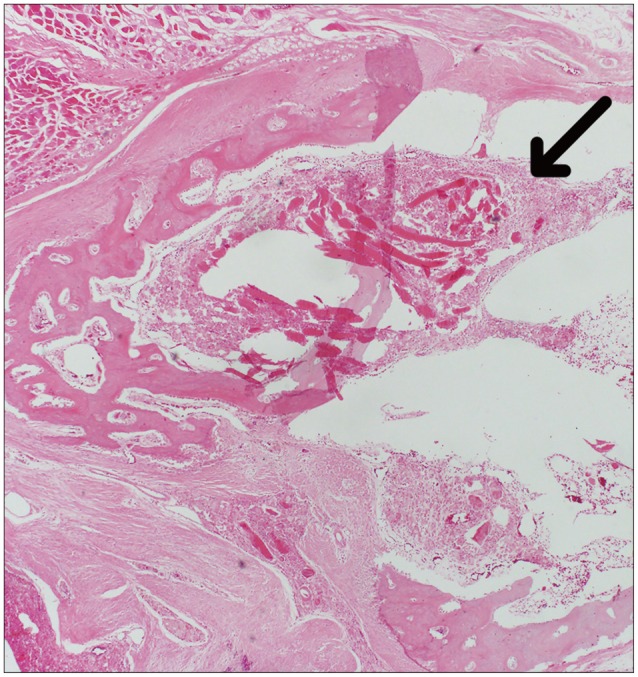
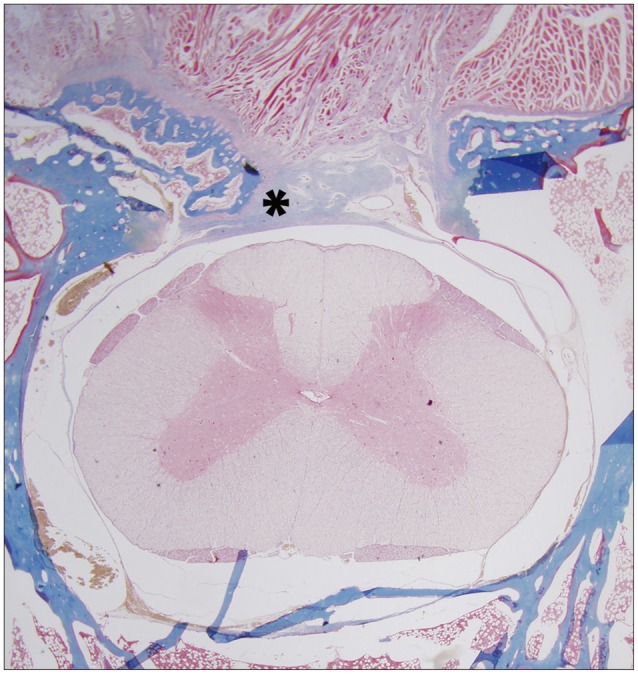
51. Yu CH, Lee JH, Baek HR, Nam H. The effectiveness of poloxamer 407-based new anti-adhesive material in a laminectomy model in rats. Eur Spine J. 2012; 21:971–979. PMID:
22160098.

52. Zavala-Rodriguez JM, Correa Rovelo JM, Martinez-Morales N, Muñoz-Arce C, Bobadilla-Lugo RA, Kross RD, et al. Oxychlorine species suppress postsurgical adhesions in rats. J Surg Res. 2014; 186:164–169. PMID:
23981708.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download