DISCUSSION
PELD is the centerpiece of the minimally invasive surgery techniques. Compared to traditional open microdiscectomy, PELD has many merits like fewer complications and morbidities in the elderly, shorter hospital stays, earlier return to normal activity and thus, higher patient satisfaction
36925). Many reports also showed that endoscopic disc surgery by experienced surgeons can achieve favorable clinical results equivalent to the standard microsurgical technique
314172021). Despite such numerous advantages and inspiring clinical results, endoscopic discectomy has not been universally adopted. There are several reasons for this, including the steep learning curve, anatomical limitations during endoscopic approach, and intraoperative complications. Some cases such as highly migrated, compromised high canal, combined with foraminal stenosis have been considered as relative contraindications in performing PELD, especially to those just beginning career in endoscopic spine surgery
1618). The incidence of failure was significantly higher in those cases due to problems like inadequate exposure, poor visualization, and an inability to reach and grasp herniated fragments. Several approaches and techniques were developed to overcome such limitations and prevent complications. Some surgeons reported other methods, such as the extreme lateral approach, epiduroscopic approach, and suprapedicular approach solve difficult epidural pathology
481622).
Percutaneous endoscopic foraminoplasty techniques have also been performed by many authors as a useful surgical strategy in such limited indications of PELD, and they have reported successful clinical outcomes of PELD combined with foraminoplasty
2571112192429).
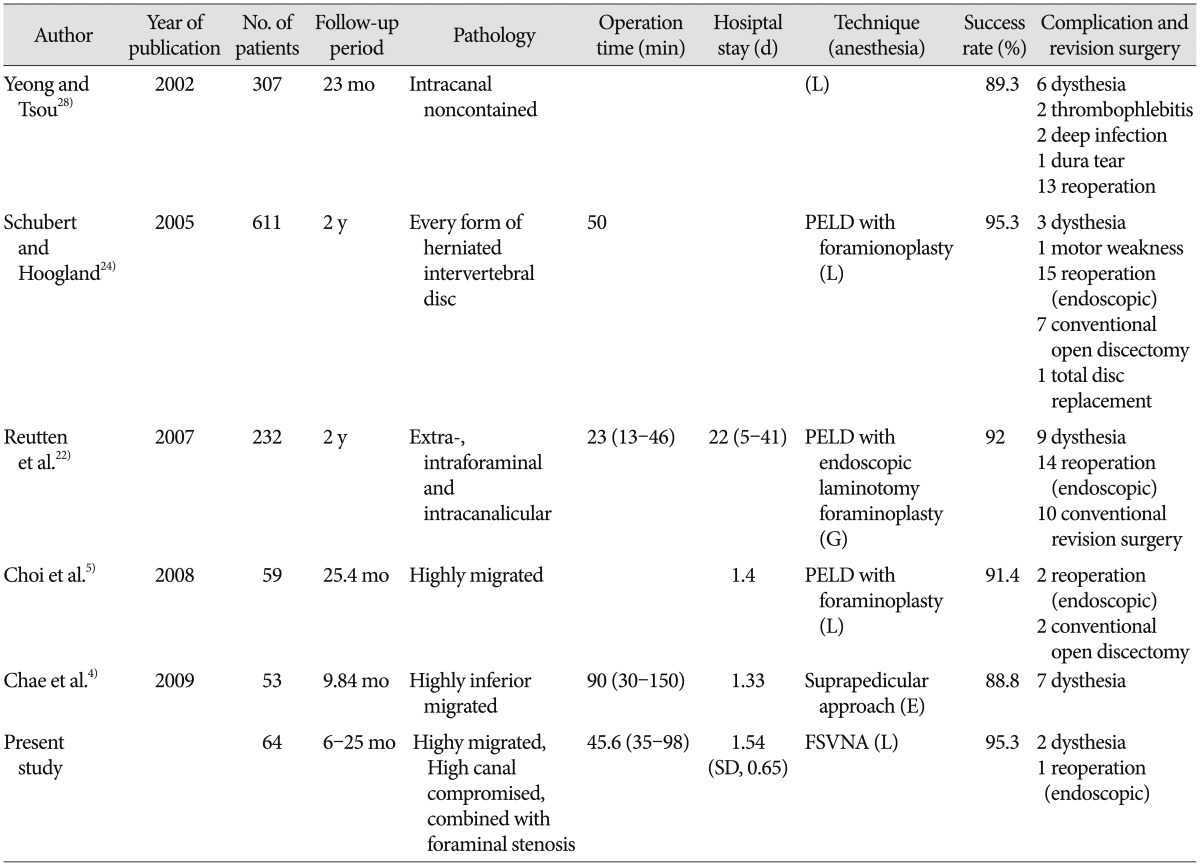
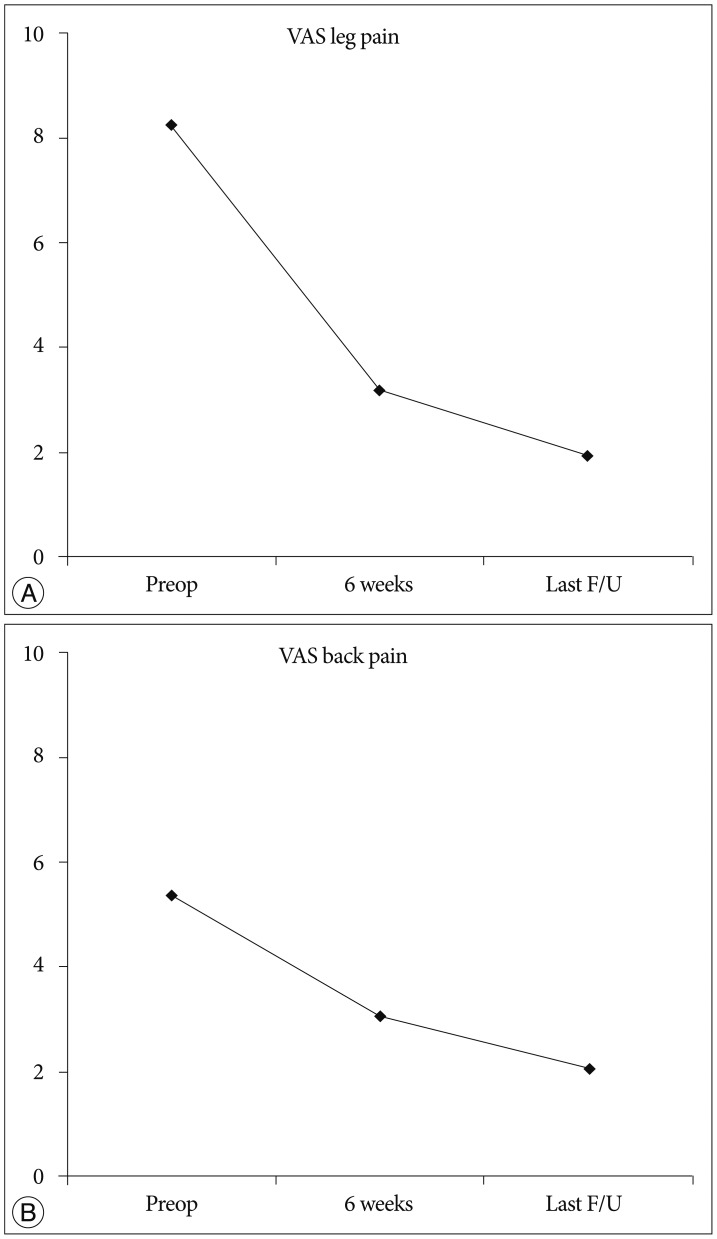
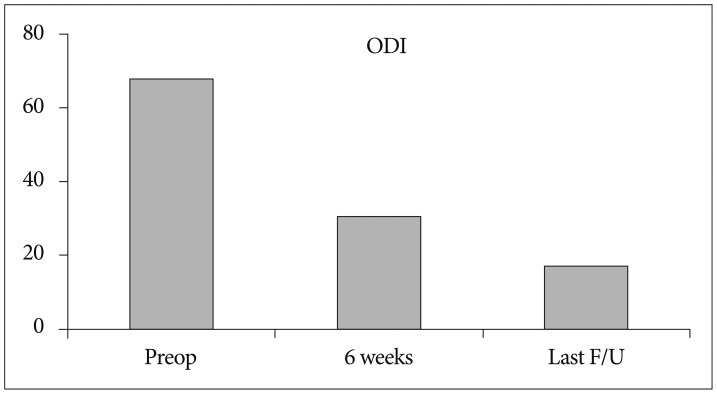
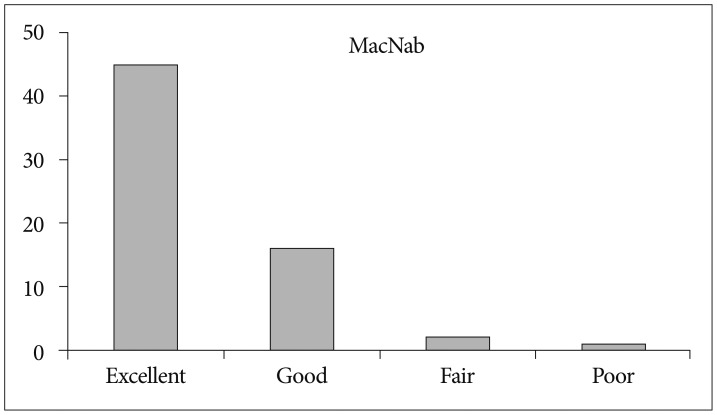
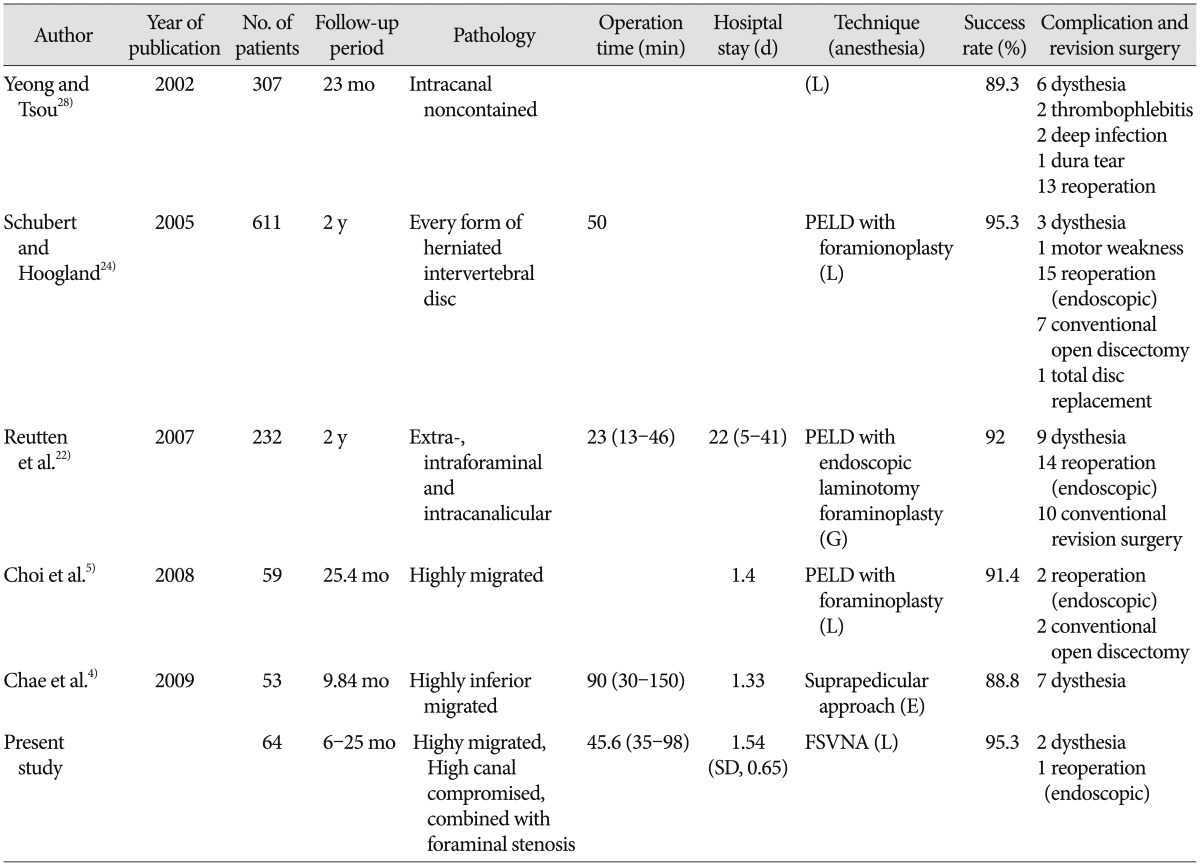
Our results also showed that the foraminoplasty technique is helpful to achieve favorable clinical outcomes of relatively contraindicated case for conducting PELD, such as in highly migrated cases, compromised high canal cases, and cases accompanied by foraminal stenosis. The global success rate in our series was 95.3%. Our surgical data demonstrated a favorable clinical outcome with a relatively low complication rate. It is inspiring that we acquired these results although we didn't include the result of rest of 535 patients who were followed-up but not included in this study because they were thought to be traditionally usual cases in PELD and expected to show better clinical results. These outcomes are comparable to those of other endoscopic techniques (
Table 3). The overall success rates of the case series ranged from 88% to 95%. We think that a direct comparison among those studies is difficult because the type of pathologies and operative technique might be somewhat different. However, it would be helpful to estimate the efficacy of FSVNA compared to other various PELD techniques.
Table 3
Comparison of clinical and surgical results with other percutaneous endoscopic lumbar discectomy for lumbar disc herniation

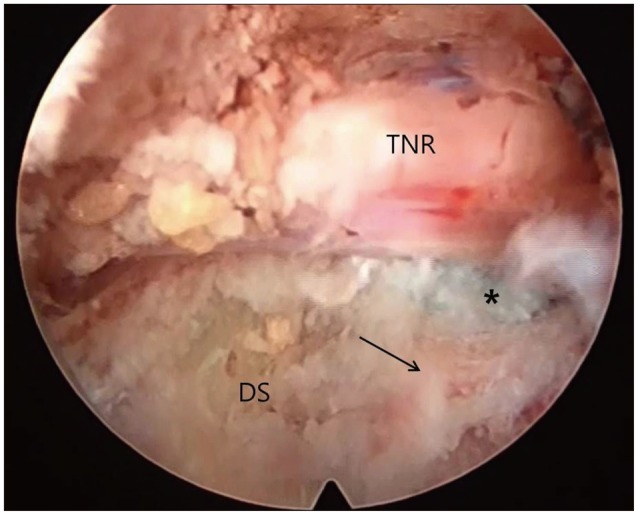
Above all things, the greatest advantage of the foraminoplasty technique is that it allows the surgeon to see enough spinal canal so the pathologic lesion in the epidural space can be easily managed, as compared to the previous conventional endoscopic approach, in which operative view was mostly confined to subligamentous annular level. Such merits enable surgeons not only to see enough epidural space but also to have the route to navigate, find the lesion and reach the relatively hidden zone far from disc space
519). The foraminoplasty technique is useful in highly migrated discs, especially in downward migrated discs. In most cases in which foraminoplasty is used, the decompression of the traversing nerve root in the epidural space could be confirmed at the end stage of procedure directly with endoscopic vision, not by the indirect pulsation of soft tissue like the posterior longitudinal ligament or remnant annulus (
Fig. 8).
Central herniation with high-grade canal compromise showed the highest rate of operative failure, and the rate was significantly different between low- and high-grade canal compromised groups
18). The current technique is basically an "outside-in" technique. In high canal compromised cases, current approach makes it possible to remove the hernia mass occupying the epidural space by just grasping the tip of the hernia mass in the endoscopic view at the subannular portion and pulling it toward the disc without removing nonpathological intradiscal nucleus tissue. Thus, it minimize the chance of neural and nonpathological disc nucleus injury which can occur during the "inside-out" technique to obtain a intradiscal working tunnel or a cavity
152728).
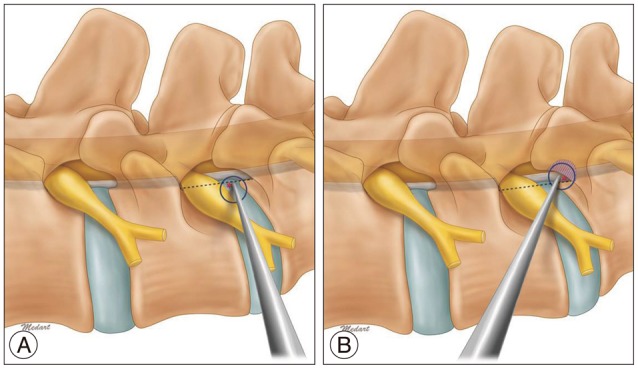
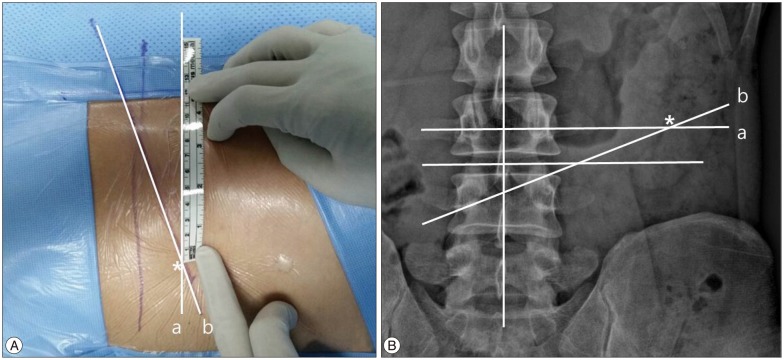
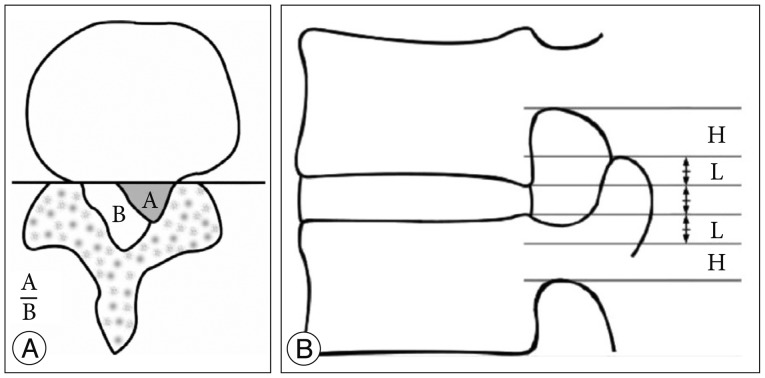
FSVNA is different from previous foraminoplasty techniques in several aspects. Previous foraminoplasty techniques requiring a reamer, which was a floating technique in the foramen region, allowing the shifting of the guiding tube's position or allowing it to slide into the cranial area of the foramen during the reaming procedure. This could lead to ineffective reaming and injury to the upper root. But in the current technique, the guide rod and tube are docked between the SAP and lower vertebral vertebral body. This allows for stable reaming without slipping and shifting of the reaming axis. Stable foraminoplasty, not shifted ventrally or cranially, allows the endoscope to be placed more dorsally close to the epidural space and more caudally far from the upper root, leading to a lower risk of interrupting the disc structure and upper exiting root.
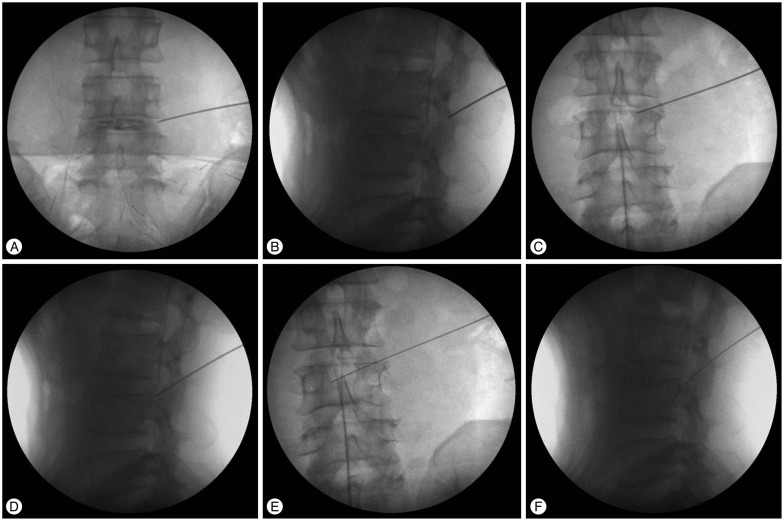
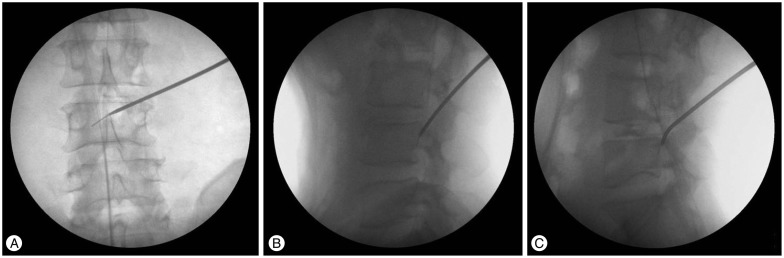
In FSVNA, docking by guide rod is accomplished between dorsal surface of lower vertebral body and ventral surface of superior articular process, not merely at the outskirt of the foramen. Approach angle in axial plane is more crucial than the size of the foramen during docking step of guide rod. Real surgical corridor between lower vertebral body and SAP for initial docking is very narrow. Inclined angle of guide rod axis in axial plane enables this docking maneuver. Precise and meticulous initial needling before the placement of guide wire is tremendously important for the success of docking procedure. It is more easy to get this approach angle in the case which have large foramen. But, sometimes, in the case with stenotic foramen by hypertrophied facet which has very narrow space between lower vertebral body and SAP, it is more difficult. Curved guide rod is needed because such a case doesn't provide enough axial inclination angle anatomically for initial guide rod docking by a straight guide rod.
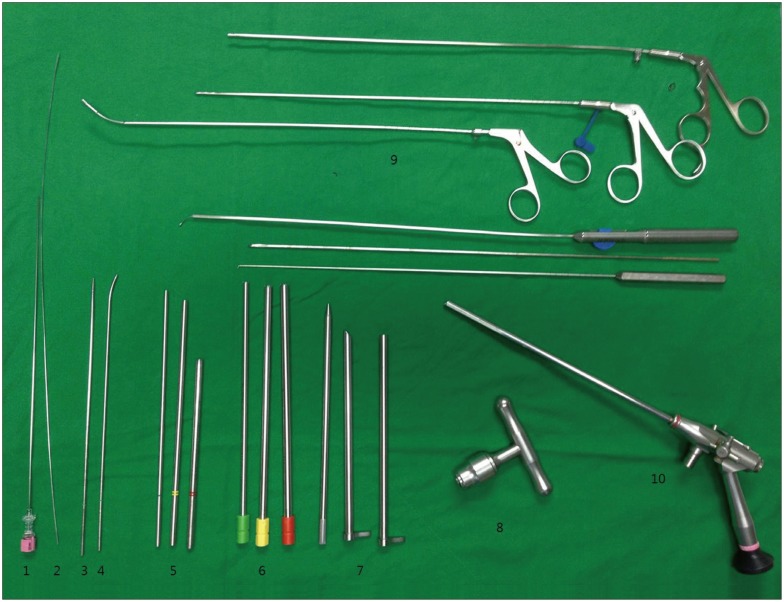
The previous foraminoplasty technique is considered to be challenging; it has steep learning curve and needs a relatively long operation time and expensive endoscopic instruments, like lasers and endoscopic drills, are required. But, the FSVNA procedure itself is simple and takes a very small amount of time (5-10 minutes). It is performed by reamers under C-arm guidance. The endoscopic drill was selectively used in the case of widening the foramen and when decompression of the upper root was needed. But, in most cases it was not necessary.
Neural injury is a point of concern because the current procedure is a blind technique. But, the first structure we encounter in the endoscopic view at the initial stage of the endoscopic surgery after reaming is mostly ligament flavum beyond the sculpted superior articular facet. Ligament flavum and facet capsule function as an anatomical barrier to prevent neural injury from the reamer in foraminoplasty. It is important to not advance the reamer over the medial pedicular line. There were no cases of nerve root injury or dural tear during approach in this clinical series.
Another concern in foraminoplasty is bleeding from an injury to the venous sinus. The endoscopic reamer pushed the resected bone fragment into the location of the venous sinus channel, the sinus was naturally blocked, inducing natural hemostasis. Most of intraoperative bleeding was minimal and spontaneously controlled by compression with the working cannula, as other authors reported
121924).
An advantage of FSVNA is also that it minimizes approach-related complications. Motor weakness and temporary dysthesia have been reported previously as most common complications in PELD. These complications showed an incidence of 2-6.53% according to the authors
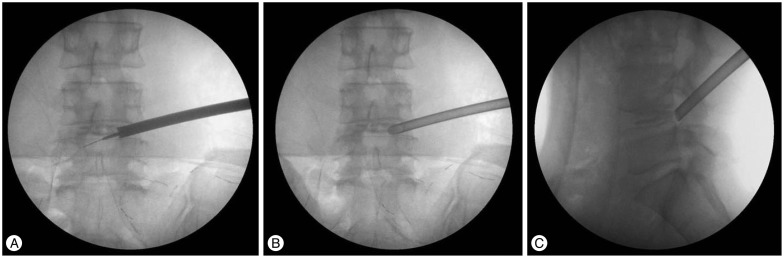
110132123). The symptoms are postulated to come from an irritation of the exiting root or traversing root during the operation. From the results of our current study, the incidence of postoperative dysthesia or motor weakness due to upper root injury was relatively low compared to the incidences reported by other studies. Confirmation of the safe triangle is important preventing this problem. In FSVNA, the space between SAP and lower vertebral body for initial docking by first guide rod is very narrow as mentioned above. But serial guide rod dilation and reaming make more space gradually for next size guide rod docking. Resection area by sequential reaming is ventral portion of SAP. These resected area is most safe anatomical point around Kambin's triangle and most far from the upper root. FSVNA is performed securely through this newly created surgical space (
Fig. 12). It is advantageous when the surgeon approaches and manipulates the working cannula in the safe zone around the foraminal area. We assume that is why the incidence of upper root injury is remarkably low during the approach and entire procedure in FSVNA.
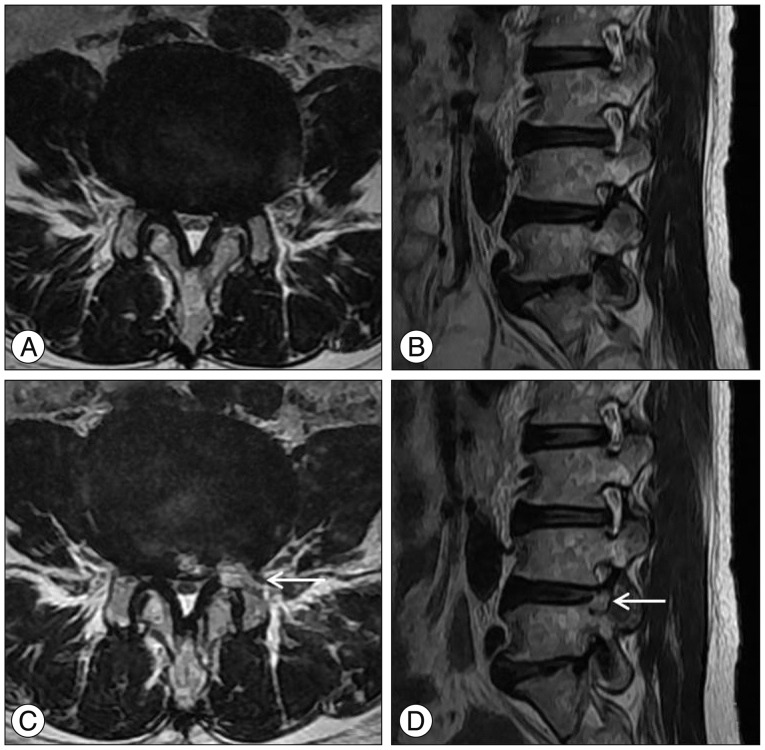
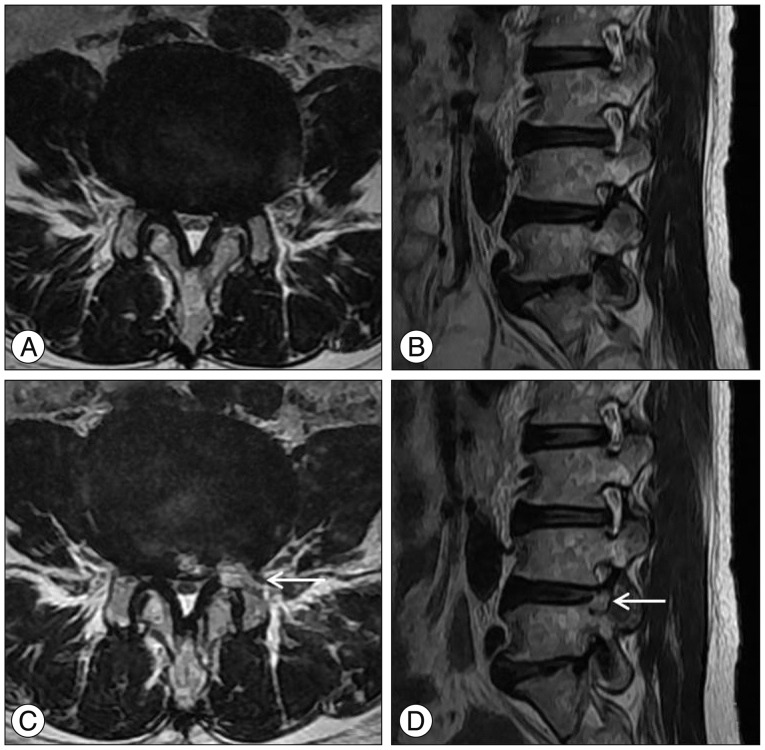 | Fig. 12Illustrated case of a 68-year-old female patient. A and B : Preoperative MR images showing severe foraminal stenosis at the Lt. L4–5 level. C and D : Postoperative MR images showing resected area (arrow) by reamer to provide safe approach route.
|
There were the cases which had already enough large foramen preoperatively. In some cases, no contact of bony structure around foramen was recognized during the first reaming. But, even in the case of large foramen, foraminoplasty was useful to trim the structures around the foramen, like the foraminal ligament and facet capsule, and allows the surgeon to acquire a better endoscopic operative view during the initial stage of the endoscopic procedure. Considering that the time consumed during foraminoplasty was, at most, about 10 minutes, foraminoplasty with reamers is worthwhile as a preparative procedure in selective cases of PELD.
But, regarding the limitations of this technique, in highly superior migrated cases, we experienced some difficulty manipulating the working channel cranially after approach, especially in obese and muscular patients because the initial angle of the working channel was slightly caudal in the coronal plane. But this limitation was overcome by readjusting the guide tube angle more cranially when reaming after placement of the guide rod. A more caudal approach at the upper level from the index level was also another good option to resolve the highly superior migrated cases. Because, as mentioned before, FSVNA is very useful in exploring the pathology which is located caudally.
We evaluated the feasibility of FSVNA in PELD in 64 cases. However, the absolute number of cases and follow-up period are not enough to compare the clinical outcome and the incidence of complications with previous reports. Further long-term study is required to prove the procedure's clinical efficacy and benefit in preventing real incidences of complications. In spite of these limitations, our results show that FSVNA is a safe and reliable method to acquire a favorable clinical outcome in limited indications for PELD.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download