CSF containing cysts at the level of choroidal fissure are rare embryological lesions
3). The choroidal fissure is the narrow cleft between the fornix and thalamus along which the choroid plexus is attached. The edges of the thalamus and fornix bordering this choroidal fissure have small ridges, called the teniae, along which the tela choroidea, the membrane in which the choroid plexus arises, is attached. The choroidal fissure is formed at approximately 8 weeks of embryonic development when the vascular piamater that forms the epithelial roof of the third ventricle invaginates into the medial wall of the cerebral hemisphere. No nervous tissue develops between the ependyma and piamater along this invagination that forms the choroidal fissure, thus creating the thinnest site in the wall of the lateral ventricle. The choroidal arteries, which supply the choroid plexus enter the ventricles through the choroidal fissure. The veins coursing in the walls of the ventricles exit the ventricles bypassing through the margin of the choroidal fissure in the subependymal location to reach the internal cerebral, basal, or great veins
4). Developmental errors may occur at the time of formation of primitive choroid plexus anywhere along the choroid fissure, thus forming a cyst
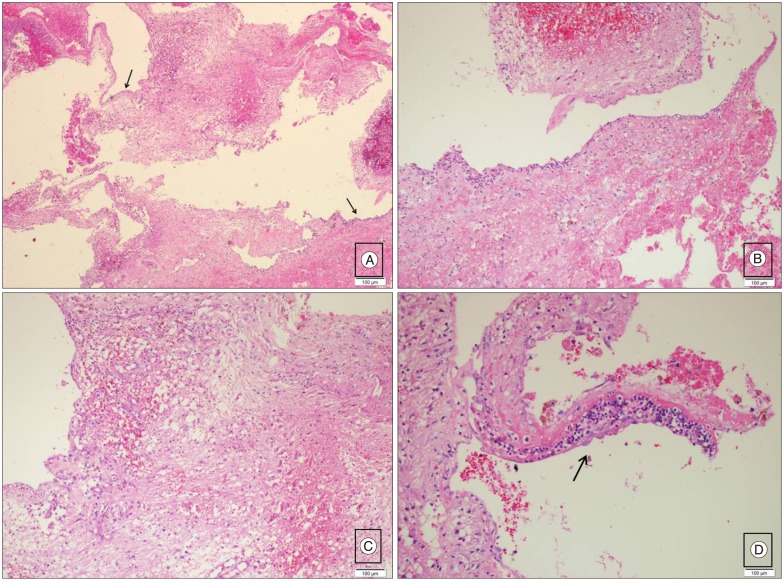
5). However, the etiology is stil controversial. The cysts may be of the neuroepithelial or arachnoid type
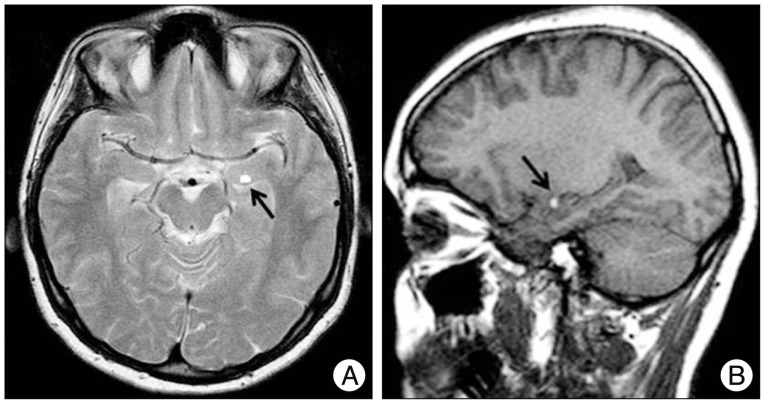
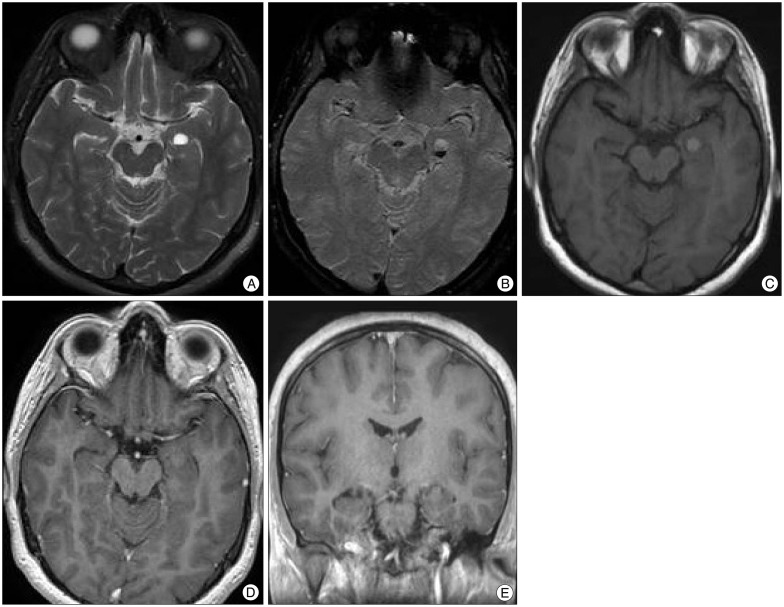
5). Lesions are spherical to ovoid, measure up to several centimeters in size
2). Sherman et al.
5) Reviewed the MRI studies of choroidal fissure cysts and reported 26 cases, mostly adults, with neurological symptoms such as complex migraine, seizure, gait disturbance, tremor, vertigo, hearing loss, paresthesia, hemiparesis and visual scotomata. Clinical follow-up without development of symptoms referable to the cyst average 17.8 months. None of these patients was operated. They reported that the cysts could not explain the patients' signs or symptoms
5). de Jong et al.
3) reported 6 patients with a CSF-containing cyst at the level of choroidal fissure with neurological symptoms such as headache, narcolepsy and hyperactivity disorder. All patients were followed with MRI which demonstrated total absence of progression of the lesions. Conservative treatment was used
3). There are limited reports about choroidal fissure cyst being treated via surgery. These usually require only follow-up. Tubbs et al.
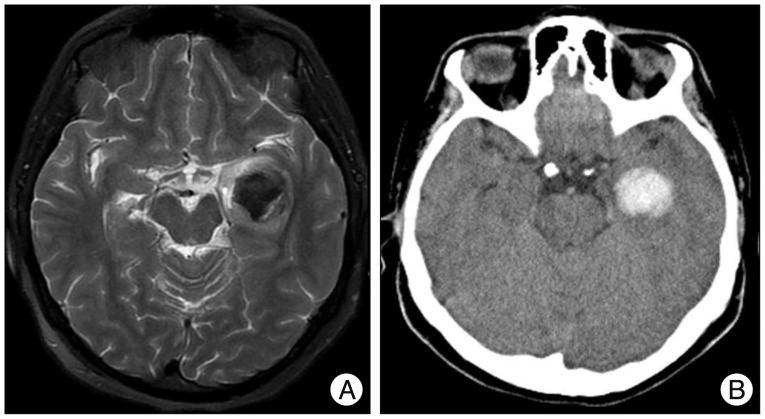
6) reported progression of choroidal fissure cysts which were treated with fenestration and possible ventriculo-peritoneal shunting. Baka and Sanders
1) reported a case of spontaneous hemorrhagic choroid plexus cyst in lateral ventricle. It was thought that the cyst was incidental and was not related to the patient's symptoms. Therefore, no treatment or further investigation was suggested
1). Differentiation between neuroepithelial and arachnoid CSF-containing cysts at the level of choroidal fissure can only be made by histopathological examination
3). Differentiation of benign choroidal fissure cysts from other cysts (cystic neoplasms or infectious cysts) is important because of the need for active treatment in the latter group. Cystic neoplasms or infectious cysts were excluded in our case because of the absence of a solid component, contrast enhancement, perilesional edema or mass effect. Dermoid cyst could also be considered in the differential diagnosis; however, in our case T1 hyperintensity represented hemorrhage and did not correspond to lipid content, since on fat-saturated T2 weighted images, nondependant part of the lesion was bright, not following the signal of fat. The presence of hemorrhage could be explained by the close relationship of the lesion with the choroid plexus of the temporal horn or the presence of heterotopic choroid plexus within the cyst. In cases of choroidal fissure cysts, at least 2 years of clinical and radiological follow-up is recommended, while surgery is indicated only in accompanying life-threatening conditions such as massive hemorrhage.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download