1. Adhiyaman V, Asghar M, Ganeshram KN, Bhowmick BK. Chronic subdural haematoma in the elderly. Postgrad Med J. 2002; 78:71–75. PMID:
11807186.

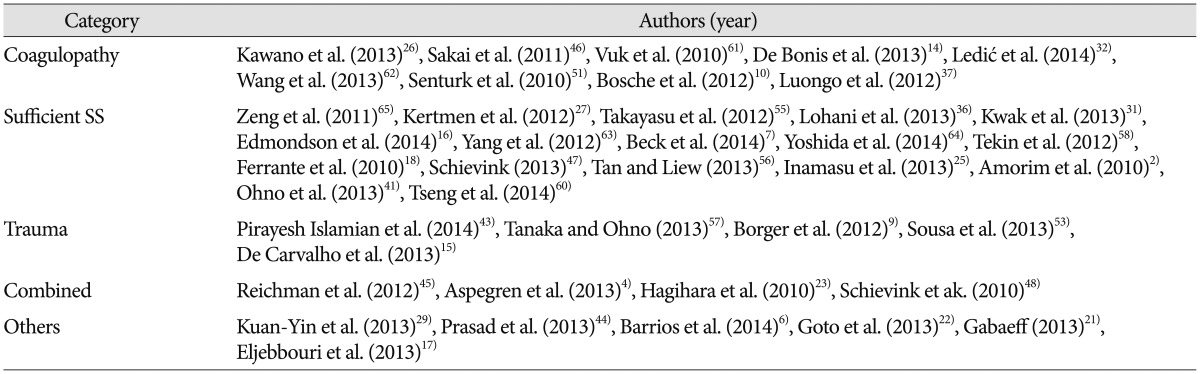
2. Amorim JA, Remígio DS, Damázio Filho O, de Barros MA, Carvalho VN, Valença MM. Intracranial subdural hematoma post-spinal anesthesia : report of two cases and review of 33 cases in the literature. Rev Bras Anestesiol. 2010; 60:620–629. 344–349. PMID:
21146058.

3. Arpino L, Gravina M, Basile D, Franco A. Spontaneous chronic subdural hematoma in a young adult. J Neurosurg Sci. 2009; 53:55–57. PMID:
19546844.
4. Aspegren OP, Åstrand R, Lundgren MI, Romner B. Anticoagulation therapy a risk factor for the development of chronic subdural hematoma. Clin Neurol Neurosurg. 2013; 115:981–984. PMID:
23128014.

5. Balser D, Farooq S, Mehmood T, Reyes M, Samadani U. Actual and projected incidence rates for chronic subdural hematomas in United States Veterans Administration and civilian populations. J Neurosurg. 2015; 20:1–7.

6. Barrios L, Clément R, Visseaux G, Bord E, Le Gall F, Rodat O. A case of atypical chronic subdural hematoma : a spontaneous rupture of dural lymphoma nodule. J Forensic Leg Med. 2014; 22:145–147. PMID:
24485439.

7. Beck J, Gralla J, Fung C, Ulrich CT, Schucht P, Fichtner J, et al. Spinal cerebrospinal fluid leak as the cause of chronic subdural hematomas in nongeriatric patients. J Neurosurg. 2014; 121:1380–1387. PMID:
25036203.

8. Berhouma M, Houissa S, Jemel H, Khaldi M. Spontaneous chronic subdural hematoma of the posterior fossa. J Neuroradiol. 2007; 34:213–215. PMID:
17572494.
9. Borger V, Vatter H, Oszvald Á, Marquardt G, Seifert V, Güresir E. Chronic subdural haematoma in elderly patients : a retrospective analysis of 322 patients between the ages of 65-94 years. Acta Neurochir (Wien). 2012; 154:1549–1554. PMID:
22772400.

10. Bosche B, Molcanyi M, Noll T, Kochanek M, Kraus B, Rieger B, et al. Occurrence and recurrence of spontaneous chronic subdural haematoma is associated with a factor XIII deficiency. Clin Neurol Neurosurg. 2013; 115:13–18. PMID:
22541133.

11. Bosma JJ, Miles JB, Shaw MD. Spontaneous chronic and subacute subdural haematoma in young adults. Acta Neurochir (Wien). 2000; 142:1307–1310. PMID:
11201648.

12. Cheng SY, Chang CK, Chen SJ, Lin JF, Tsai CC. Chronic subdural hematoma in elderly taiwan patients : a retrospective analysis of 342 surgical cases. Int J Geront. 2014; 8:37–41.

13. D'Errico AP, German WJ. Chronic Subdural Hematoma. Yale J Biol Med. 1930; 3:11–20. PMID:
21433469.
14. De Bonis P, Trevisi G, de Waure C, Sferrazza A, Volpe M, Pompucci A, et al. Antiplatelet/anticoagulant agents and chronic subdural hematoma in the elderly. PLoS One. 2013; 8:e68732. PMID:
23874740.

15. De Carvalho D, Almenawer S, Lozej M, Noble H, Murty NK. Spontaneous chronic subdural hematoma in a 22-year-old healthy woman. World Neurosurg. 2013; 80:654.e9–654.e11. PMID:
23182734.

16. Edmondson L, Upshaw JE, Tuuri RE. A 14-year-old male with a 10-week history of headaches. Pediatr Ann. 2014; 43:220222–223. PMID:
24972416.

17. Eljebbouri B, Okacha N, Boucetta M. Chronic subdural hematoma infected by Campylobacter fetus. Surg Infect (Larchmt). 2013; 14:563–564. PMID:
23930907.
18. Ferrante E, Arpino I, Citterio A, Wetzl R, Savino A. Epidural blood patch in Trendelenburg position pre-medicated with acetazolamide to treat spontaneous intracranial hypotension. Eur J Neurol. 2010; 17:715–719. PMID:
20050898.

19. Fogelholm R, Heiskanen O, Waltimo O. Chronic subdural hematoma in adults. Influence of patient's age on symptoms, signs, and thickness of hematoma. J Neurosurg. 1975; 42:43–46. PMID:
1167376.
20. Forster MT, Mathé AK, Senft C, Scharrer I, Seifert V, Gerlach R. The influence of preoperative anticoagulation on outcome and quality of life after surgical treatment of chronic subdural hematoma. J Clin Neurosci. 2010; 17:975–979. PMID:
20580997.

21. Gabaeff SC. Investigating the possibility and probability of perinatal subdural hematoma progressing to chronic subdural hematoma, with and without complications, in neonates, and its potential relationship to the misdiagnosis of abusive head trauma. Leg Med (Tokyo). 2013; 15:177–192. PMID:
23434514.

22. Goto T, Ohshima S, Miura K, Shibuya T, Sato W, Dohmen T, et al. A chronic subdural hematoma in a patient receiving combination therapy with pegylated interferon alfa-2b and ribavirin for chronic hepatitis C. Intern Med. 2013; 52:2057–2060. PMID:
24042512.

23. Hagihara N, Abe T, Kojima K, Watanabe M, Tabuchi K. Coexistence of cranial and spinal subdural hematomas : case report. Neurol Med Chir (Tokyo). 2010; 50:333–335. PMID:
20448430.

24. Hong JC, Kim MS, Chang CH, Kim SH. Arachnoid cyst with spontaneous intracystic hemorrhage and chronic subdural hematoma. J Korean Neurosurg Soc. 2008; 43:54–56. PMID:
19096549.

25. Inamasu J, Watabe T, Ganaha T, Yamada Y, Nakae S, Ohmi T, et al. Clinical characteristics and risk factors of chronic subdural haematoma associated with clipping of unruptured cerebral aneurysms. J Clin Neurosci. 2013; 20:1095–1098. PMID:
23669172.

26. Kawano H, Yamamoto D, Uchihashi Y, Wakahashi K, Kawano Y, Sada A, et al. Severe inhibitor-negative acquired factor XIII/13 deficiency with aggressive subdural haemorrhage. Blood Coagul Fibrinolysis. 2013; 24:638–641. PMID:
23511901.

27. Kertmen H, Gürer B, Yilmaz ER, Sekerci Z. Chronic subdural hematoma associated with an arachnoid cyst in a juvenile taekwondo athlete : a case report and review of the literature. Pediatr Neurosurg. 2012; 48:55–58. PMID:
22832284.

28. Kim BW, Jung YJ, Kim MS, Choi BY. Chronic subdural hematoma after spontaneous intracranial hypotension : a case treated with epidural blood patch on c1-2. J Korean Neurosurg Soc. 2011; 50:274–276. PMID:
22102965.

29. Kuan-Yin T, Dueng-Yuan H, Hsin-I M. Subdural hematoma associated with skull and dural metastasis of gastric carcinoma : a case report. Turk Neurosurg. 2013; 23:796–799. PMID:
24310465.
30. Kuramae T, Inamasu J, Nakagawa Y, Nakatsukasa M. Spontaneous intracranial hypotension presenting without orthostatic headache complicated by acute subdural hematoma after drainage for chronic subdural hematoma--case report. Neurol Med Chir (Tokyo). 2011; 51:518–521. PMID:
21785248.

31. Kwak YS, Hwang SK, Park SH, Park JY. Chronic subdural hematoma associated with the middle fossa arachnoid cyst : pathogenesis and review of its management. Childs Nerv Syst. 2013; 29:77–82. PMID:
22914923.

32. Ledić D, Girotto D, Pal S, Kolbah B. Risk factors for subdural bleeding in elderly population. Coll Antropol. 2014; 38:1195–1198. PMID:
25842756.
33. Lee KS, Bae WK, Doh JW, Bae HG, Yun IG. Origin of chronic subdural haematoma and relation to traumatic subdural lesions. Brain Inj. 1998; 12:901–910. PMID:
9839025.
34. Lee KS, Bae WK, Park YT, Yun IG. The pathogenesis and fate of traumatic subdural hygroma. Br J Neurosurg. 1994; 8:551–558. PMID:
7857535.

35. Lindvall P, Koskinen LO. Anticoagulants and antiplatelet agents and the risk of development and recurrence of chronic subdural haematomas. J Clin Neurosci. 2009; 16:1287–1290. PMID:
19564115.

36. Lohani S, Robertson RL, Proctor MR. Ruptured temporal lobe arachnoid cyst presenting with severe back pain. J Neurosurg Pediatr. 2013; 12:281–283. PMID:
23829378.

37. Luongo M, Pizzuti M, Godano U. Bilateral chronic subdural non-traumatic hematoma associated with von Willebrand's type I disease : a case report. Acta Neurochir (Wien). 2012; 154:1087–1088. PMID:
22392015.

38. Markwalder TM. Chronic subdural hematomas : a review. J Neurosurg. 1981; 54:637–645. PMID:
7014792.
39. Missori P, Domenicucci M, Sassun TE, Tarantino R, Peschillo S. Alterations in the intracranial venous sinuses in spontaneous nontraumatic chronic subdural hematomas. J Clin Neurosci. 2013; 20:389–393. PMID:
23219821.

40. Mori K, Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases : clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir (Tokyo). 2001; 41:371–381. PMID:
11561347.

41. Ohno T, Iihara K, Takahashi JC, Nakajima N, Satow T, Hishikawa T, et al. Incidence and risk factors of chronic subdural hematoma after aneurysmal clipping. World Neurosurg. 2013; 80:534–537. PMID:
23072878.

42. Park HR, Lee KS, Shim JJ, Yoon SM, Bae HG, Doh JW. Multiple densities of the chronic subdural hematoma in CT scans. J Korean Neurosurg Soc. 2013; 54:38–41. PMID:
24044079.

43. Pirayesh Islamian A, Polemikos M, Krauss JK. Chronic subdural haematoma secondary to headbanging. Lancet. 2014; 384:102. PMID:
24998813.

44. Prasad BC, Chandra VV, Varaprasad G. Dural metastases in chronic myeloid leukemia presenting as subdural hematoma. Turk Neurosurg. 2012; 22:777–778. PMID:
23208914.

45. Reichman J, Singer S, Navi B, Reiner A, Panageas K, Gutin PH, et al. Subdural hematoma in patients with cancer. Neurosurgery. 2012; 71:74–79. PMID:
22705720.

46. Sakai N, Akamine S, Tokuyama T, Sugiyama K, Kanayama N, Namba H. Chronic subdural hematoma in a patient with congenital afibrinogenemia successfully treated with fibrinogen replacement. Neurol Med Chir (Tokyo). 2011; 51:780–783. PMID:
22123482.

47. Schievink WI. Stroke and death due to spontaneous intracranial hypotension. Neurocrit Care. 2013; 18:248–251. PMID:
23196352.

48. Schievink WI, Maya MM, Moser FG, Tourje J. Spectrum of subdural fluid collections in spontaneous intracranial hypotension. J Neurosurg. 2005; 103:608–613. PMID:
16266041.

49. Schievink WI, Maya MM, Pikul BK, Louy C. Spontaneous spinal cerebrospinal fluid leaks as the cause of subdural hematomas in elderly patients on anticoagulation. J Neurosurg. 2010; 112:295–299. PMID:
19199465.

50. Seçkin H, Kazanci A, Yigitkanli K, Simsek S, Kars HZ. Chronic subdural hematoma in patients with idiopathic thrombocytopenic purpura: a case report and review of the literature. Surg Neurol. 2006; 66:411–414. discussion 414PMID:
17015125.

51. Senturk S, Guzel E, Bayrak AH, Bukte Y, Guzel A. Factor X deficiency presenting with bilateral chronic subdural hematoma. Pediatr Neurosurg. 2010; 46:54–57. PMID:
20516741.

52. Sim YW, Min KS, Lee MS, Kim YG, Kim DH. Recent changes in risk factors of chronic subdural hematoma. J Korean Neurosurg Soc. 2012; 52:234–239. PMID:
23115667.

53. Sousa EB, Brandão LF, Tavares CB, Borges IB, Neto NG, Kessler IM. Epidemiological characteristics of 778 patients who underwent surgical drainage of chronic subdural hematomas in Brasília, Brazil. BMC Surg. 2013; 13:5. PMID:
23452673.

54. Taarnhoj P. Chronic subdural hematoma; historical review and analysis of 60 cases. Cleve Clin Q. 1955; 22:150–156. PMID:
13261320.

55. Takayasu T, Harada K, Nishimura S, Onda J, Nishi T, Takagaki H. Chronic subdural hematoma associated with arachnoid cyst. Two case histories with pathological observations. Neurol Med Chir (Tokyo). 2012; 52:113–117. PMID:
22362297.
56. Tan VE, Liew D. A case of chronic subdural hematoma following lumbar drainage for the management of iatrogenic cerebrospinal fluid rhinorrhea : pitfalls and lessons. Ear Nose Throat J. 2013; 92:513–515. PMID:
24170465.

57. Tanaka Y, Ohno K. Chronic subdural hematoma - an up-to-date concept. J Med Dent Sci. 2013; 60:55–61. PMID:
23918031.
58. Tekin T, Colak A, Kutlay M, Demircan MN. Chronic subdural hematoma after endoscopic third ventriculostomy : a case report and literature review. Turk Neurosurg. 2012; 22:119–122. PMID:
22274985.
59. Thirumal Y, Alugolu R. Spontaneous chronic subdural hematoma following Plasmodium vivax malaria : a rare association. J Vector Borne Dis. 2014; 51:73–74. PMID:
24717209.
60. Tseng JH, Tseng MY, Liu AJ, Lin WH, Hu HY, Hsiao SH. Risk factors for chronic subdural hematoma after a minor head injury in the elderly : a population-based study. Biomed Res Int. 2014; 2014:218646. PMID:
25295251.
61. Vuk A, Stancić V, Rincić G, Ledinsky M, Grbac L, Stancić N. Nontraumatic bilateral subdural hematoma caused by antiaggregation therapy : case report and review of the literature. Acta Clin Croat. 2010; 49:163–168. PMID:
21086734.
62. Wang HS, Kim SW, Kim SH. Spontaneous chronic subdural hematoma in an adolescent girl. J Korean Neurosurg Soc. 2013; 53:201–203. PMID:
23634275.

63. Yang AI, Balser DS, Mikheev A, Offen S, Huang JH, Babb J, et al. Cerebral atrophy is associated with development of chronic subdural haematoma. Brain Inj. 2012; 26:1731–1736. PMID:
22759238.

64. Yoshida H, Takai K, Taniguchi M. Leakage detection on CT myelography for targeted epidural blood patch in spontaneous cerebrospinal fluid leaks : calcified or ossified spinal lesions ventral to the thecal sac. J Neurosurg Spine. 2014; 21:432–441. PMID:
24949904.

65. Zeng T, Shi SS, Lin YF. Chronic subdural hematoma associated with sylvian arachnoid cyst in juvenile athletes : report of two cases and literature review. Chin J Traumatol. 2011; 14:174–177. PMID:
21635806.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download