Abstract
Rheumatoid arthritis (RA) is a chronic inflammatory disease involving multiple joints. The cervical spine is often affected, and cases involving atlantoaxial joint can lead to instability. Anterior atlantoaxial subluxation in RA patients can lead to posterior neck pain or occipital headache because of compression of the C2 ganglion or nerve. Here, we report the successful treatment of a RA patient with occipital radiating headache using pulsed radiofrequency therapy at the C2 dorsal root ganglion.
Go to : 
Rheumatoid arthritis (RA) is characterized by an abnormal immune response, leading to progressive synovial inflammation and joint destruction6). The cervical spine is often affected, and cervical pain is reported by 40-88% of RA patients. Radiological examination shows cervical subluxation in 43-86% of RA patients12). Atlantoaxial subluxation accounts for 65% of cervical complications associated with RA. Cervical subluxation occurs primarily as anterior atlantoaxial subluxation (20%), representing the most common cervical lesion in RA11). Atlantoaxial subluxation develops via multiple mechanisms, including inflammation of the transverse cruciate ligament around the dens and erosion of the dens itself8). Compression of the second cervical dorsal root ganglion (DRG) may also occur in patients with atlantoaxial subluxation, leading to headaches in the occipital region. We report a case in which pulsed radiofrequency (PRF) therapy was successful in controlling posterior neck pain and radiating occipital pain in a RA patient with atlantoaxial subluxation.
Go to : 
A 74-year-old female patient visited our pain clinic complaining of right posterior neck pain and occipital radiating pain occurring for the past 2-3 years. The patient had been diagnosed with RA 30 years prior. The patient was being treated with 5 mg/day prednisolone, 1300 mg/day acetaminophen, 25 mg/week etanercept and 10 mcg/week buprenorphine (patch). The patient had also been diagnosed with hypertension and osteoporosis.
The posterior neck pain was continuous with a dull quality, and the pain intensity was rated as 6/10 on the visual analog scale (VAS). For pain intensity, the VAS ranges from "no pain" (score of 0) to "pain as bad as it could be" or "worst imaginable pain" (score of 10). The patient complained of right occipital radiating, electric shock-like paroxysmal pain during neck movement, with a pain intensity of 10/10 on the VAS. Radiating pain did not occur without neck motion or when the patient was in a supine position. Physical examination confirmed the occurrence of pain in the right occipital area precipitated by cervical movement and severe tenderness in the right 4th, 5th, and 6th cervical facet joint regions.
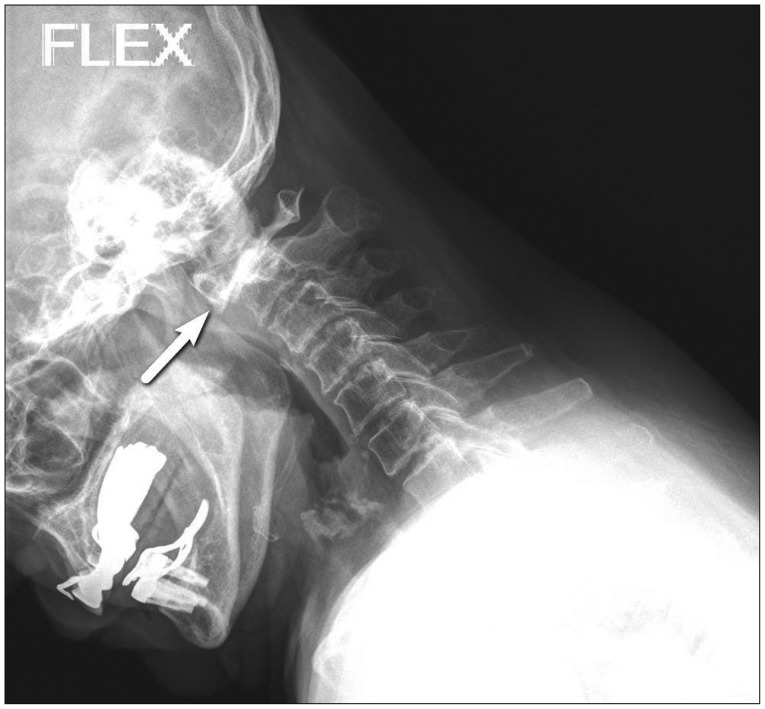
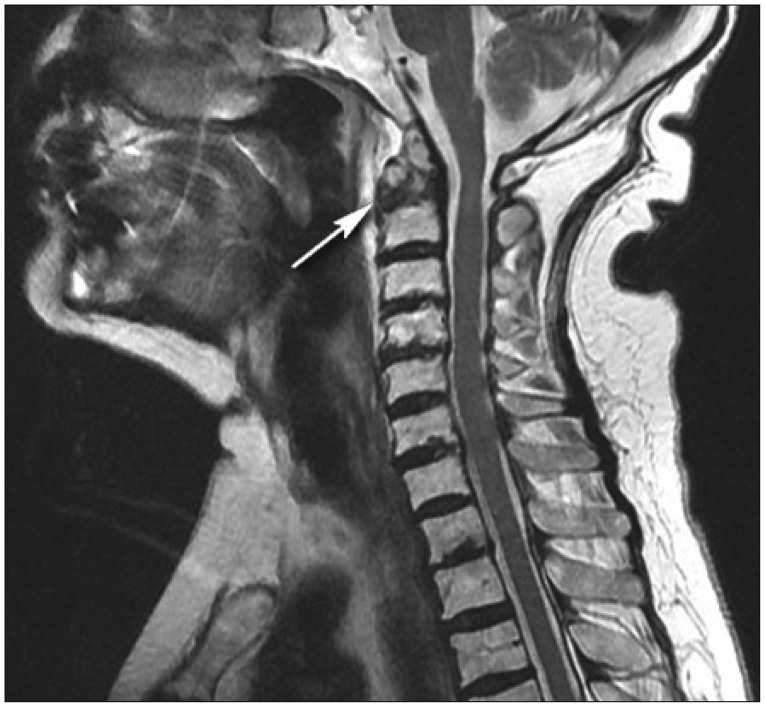
The atlantodental interval (ADI) was measured as 4.5 mm, based on a simple lateral cervical radiographic examination (Fig. 1). A cervical magnetic resonance imaging (MRI) study revealed a fracture of the odontoid process (type II), myelopathy associated with instability, limited flexion and extension associated with focal sagittal segmental instability in the atlantoaxial joint, and severe cervical spondylosis (Fig. 2).
Initial treatment consisted of right 3rd occipital and right 4th, 5th, and 6th cervical medial branch blocks under fluoroscopic guidance. Levobupivacaine (0.3 mL; 0.75%) and triamcilonone (1 mg) were injected at each level. Although the posterior neck pain intensity was reduced to a VAS score of 3, the radiating occipital pain was not affected. We next performed a cervical epidural block and repeated treatment after 1 week. A 20-gauge Touhy needle was inserted into the right side interlaminar space of the 5th cervical spine and 6th cervical spine under fluoroscopic guidance. We confirmed the location of the epidural space using a contrast medium (iopamidol 1 mL) after feeling loss of resistance (LOR) and subsequently injected lidocaine (0.5%; 6 mL) and betamethasone (2 mg). The intensity of the radiating occipital pain was reduced to a VAS score of 3 for 2 days after each block.
We next performed a C2 DRG block after suspecting that the pain could be associated with C2 radiculopathy, owing to atlantoaxial joint instability. Lidocaine (1%; 3 mL) and betamethasone (2 mg) were injected using a 22-gauge ciba needle, after confirming the location of the right C2 DRG under flouroscopic guidance using 0.5 mL iopamidol. Following this treatment, the pain disappeared for 2 days but increased thereafter. After confirming the positive result, the patient was scheduled for PRF therapy.
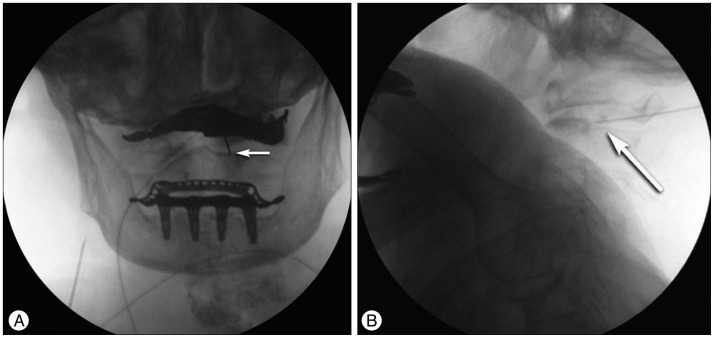
PRF therapy was performed in the prone position using a C-arm for appropriate needle positioning. A 21-gauge 10-cm insulated needle was inserted between the lamina of atlas and the lamina of axis, by referring to lateral images, and was advanced toward the center of the C2 pedicle, by referring to anterior-posterior images. The needle tip did not cross the medial side of the pedicle during the procedure. The C2 nerve ganglion was identified by applying a 50-Hz, 0.6-V electrical stimulation, using a radiofrequency generator, and injecting contrast medium (iopamidol; 0.5 mL). PRF therapy was performed at 42℃ for 120 seconds and repeated three times (Fig. 3). The patient has not complained of any occipital radiculopathy for 6 months, and the posterior neck pain has since been reduced to a VAS score of 3.
Go to : 
RA patients with atlantoaxial subluxation complain of occipital and posterior neck pain, which is aggravated by cervical locomotion and is sometimes accompanied by crepitation. Additional neuralgia of the face, ear and occiput can occur as a result of C2 root compression10). Subtle changes may be masked in the case of severe peripheral articular disease11). Several physical examinations may help with diagnosis. A positive result of the Sharp-Pruser test is described as a clunking sensation associated with spontaneous atlantoaxial reduction during neck extension. Lhermitte's phenomenon, characterized by electric shock-like sensations of the extremities in response to forward flexion of the head, may also be present6). These symptoms are caused by irritation of the C2 nerve ganglia and nerve root, since the second cervical DRG is exposed to the atlantoaxial zygapophygeal joint16).
Atlantoaxial instability is defined as loss of the stable configuration of the anterior C1-2 synovial articulation, resulting in abnormal movement. Although most patients with cervical spine involvement are asyptomatic for years, they show approximately 50% radiological progression during follow-up1). A positive diagnosis is made if the ADI exceeds 3 mm8), as assessed by lateral cervical radiographic examination. Our patient had an ADI of 4.5 mm. The average onset time for myelopathy is 16.6 years in RA patients, but it can be detected earlier in males, particularly in cases associated with the peripheral joints and long-term use of steroids9). Myelography or MRI can accurately diagnose neural compression, spinal stenosis, bony erosion, and others; however, simple X-ray images are a cost-efficient means of predicting neurological complications by measuring the anterior ADI or posterior ADI5).
The pathophysiology of anterior atlantoaxial subluxation is similar to that observed in other peripheral joints and involves proliferation of fibroblasts and inflammatory cells, resulting in rheumatoid pannus. This pannus destroys cartilage, ligaments and bones by generating collagenase and other proteolytic enzymes. The resulting destructive synovitis induces ligament laxity and bony erosion, which leads to cervical spine instability and subluxation7).
Diverse methods, beginning with palliative treatment, have been applied to treat pain caused by irritation of the C2 nerve ganglion and nerve root associated with anterior atlantoaxial subluxation. Surgical approaches include micro decompression, neurectomy and atlantoaxial fusion, while other interventions, such as RF therapy have also been used14). However, limited data exist regarding the effects of conventional RF (CRF) and PRF on pain caused by anterior atlantoaxial subluxation. Shim and Shim13) reported pain relief lasting 6 months after CRF in two RA patients with anterior atlantoaxial subluxation. Similarly, Zhang et al.6) reported pain relief lasting 6 months after PRF in patients with cervicogenic headaches. PRF provides a long-term reduction in headaches with minimal procedural risks in selected patients with medically intractable occipital neuralgia4). These studies suggest that PRF therapy may be an effective alternative treatment for patients with posterior neck pain due to anterior atlantoaxial subluxation.
Although the exact mechanism of PRF action is not known, it is believed to involve changes in neurotransmission at the site of stimulation2). Unlike CRF, which can cause nerve and tissue injuries because of the relatively high temperature involved, PRF uses a pulsating high-frequency stimulation at a temperature below 42℃ for 0.5 s, repeated at 20-ms intervals. Due to the relatively short procedural duration and lower risk, PRF can be applied to regions known to be at a relatively high risk of complications2). PRF provides a shorter duration of pain relief than does CRF, but it has fewer complications and is safer. It has also been shown that PRF is effective in cases where the needle approach would be difficult technically2). PRF can also be used to treat neuropathic pain, because it does not destroy nerves or block their transmission. Conversely, CRF damages nerves and therefore is not used frequently for neuropathic pain3).
Facet joint pain due to severe c-spine spondylosis was considered to be the cause of the patient's continuous neck pain. Consistent with this, pain was reduced efficiently after a cervical medial branch block. We suspected that the radiating occipital pain experienced during neck movement was associated with C2 radiculopathy and therefore performed a C2 DRG block, which successfully reduced radiating pain for 2 days. The patient subsequently received additional PRF therapy and was pain-free for more than 6 months.
Go to : 
References
1. Ahn JK, Hwang JW, Oh JM, Lee J, Lee YS, Jeon CH, et al. Risk factors for development and progression of atlantoaxial subluxation in Korean patients with rheumatoid arthritis. Rheumatol Int. 2011; 31:1363–1368. PMID: 20422194.

3. Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008; 12:37–41. PMID: 18417022.

4. Choi HJ, Oh IH, Choi SK, Lim YJ. Clinical outcomes of pulsed radiofrequency neuromodulation for the treatment of occipital neuralgia. J Korean Neurosurg Soc. 2012; 51:281–285. PMID: 22792425.

5. Dreyer SJ, Boden SD. Natural history of rheumatoid arthritis of the cervical spine. Clin Orthop Relat Res. 1999; (366):98–106. PMID: 10627723.

6. Hohl JB, Grabowski G, Donaldson WF III. Cervical deformity in rheumatoid arthritis. Semin Spine Surg. 2011; 23:181–187.

7. Kim DH, Hilibrand AS. Rheumatoid arthritis in the cervical spine. J Am Acad Orthop Surg. 2005; 13:463–474. PMID: 16272271.

8. Mathews JA. Atlanto-axial subluxation in rheumatoid arthritis. Ann Rheum Dis. 1969; 28:260–266. PMID: 5772521.

9. Mathews JA. Atlanto-axial subluxation in rheumatoid arthritis. A 5-year follow-up study. Ann Rheum Dis. 1974; 33:526–531. PMID: 4441130.

10. Monsey RD. Rheumatoid arthritis of the cervical spine. J Am Acad Orthop Surg. 1997; 5:240–248. PMID: 10795060.

11. Nguyen HV, Ludwig SC, Silber J, Gelb DE, Anderson PA, Frank L, et al. Rheumatoid arthritis of the cervical spine. Spine J. 2004; 4:329–334. PMID: 15125859.

12. Reiter MF, Boden SD. Inflammatory disorders of the cervical spine. Spine (Phila Pa 1976). 1998; 23:2755–2766. PMID: 9879101.

13. Shim JH, Shim JC. Radiofrequency C2 ganglionotomy in atlantoaxial subluxation : short term follow up. J Korean Pain Soc. 2001; 14:193–198.
14. van Suijlekom H, Van Zundert J, Narouze S, van Kleef M, Mekhail N. 6. Cervicogenic headache. Pain Pract. 2010; 10:124–130. PMID: 20415729.
15. Yamashita T, Yoshino S, Nagashima M, Saitou K, Shu G, Matuoka T, et al. Prevalence of cervical lesions in rheumatoid arthritis : cross-sectional study on 263 patients. Mod Rheumatol. 2000; 10:211–215. PMID: 24383631.

16. Zhang J, Shi DS, Wang R. Pulsed radiofrequency of the second cervical ganglion (C2) for the treatment of cervicogenic headache. J Headache Pain. 2011; 12:569–571. PMID: 21611808.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download