Abstract
Objective
Lumbar spinal stenosis is conventionally treated with surgical decompression. However, bilateral decompression and laminectomy is more invasive and may not be necessary for lumbar stenosis patients with unilateral radiculopathy. We aimed to report the outcomes of unilateral laminectomy and bilateral pedicle screw fixation with fusion for patients with lumbar spinal stenosis and unilateral radiculopathy.
Methods
Patients with lumbar spinal stenosis with unilateral lower extremity radiculopathy who received limited unilateral decompression and bilateral pedicle screw fixation were included and evaluated using visual analog scale (VAS) pain and the Oswestry Disability Index (ODI) scores preoperatively and at follow-up visits. Ligamentum flavum thickness of the involved segments was measured on axial magnetic resonance images.
Results
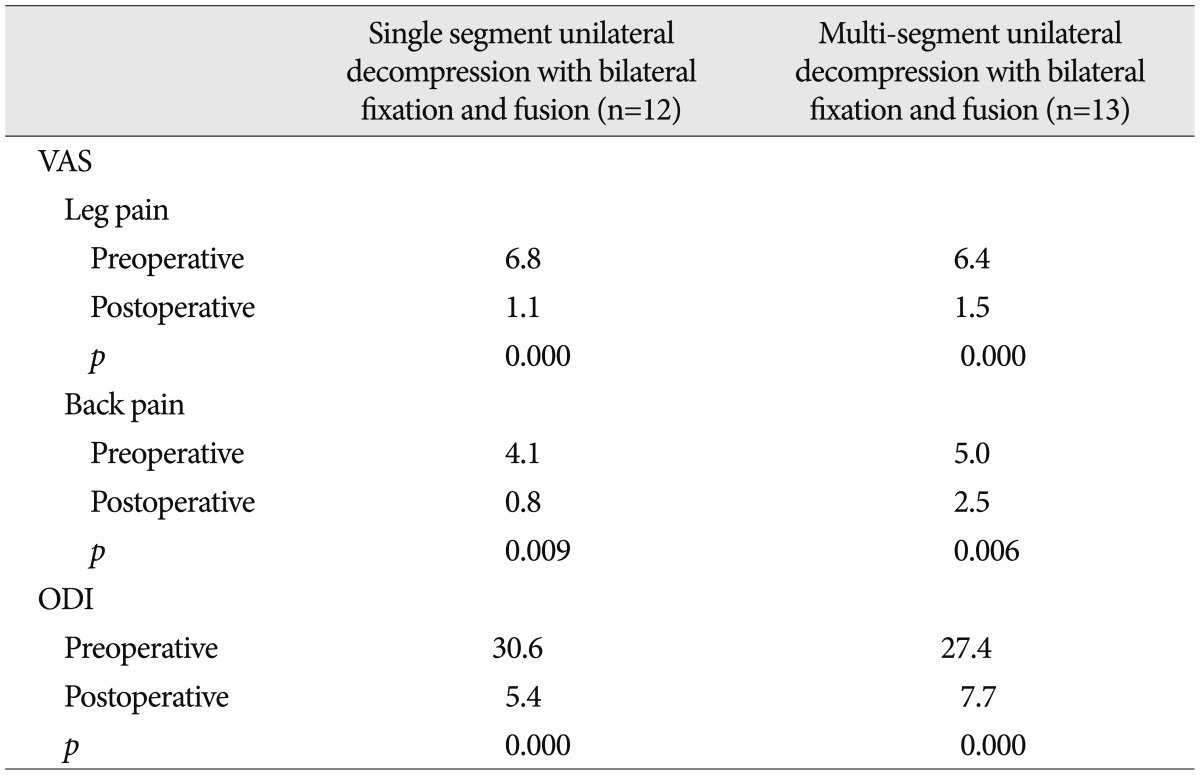
Twenty-five patients were included. The mean preoperative VAS score was 6.6±1.6 and 4.6±3.1 for leg and back pain, respectively. Ligamentum flavum thickness was comparable between the symptomatic and asymptomatic side (p=0.554). The mean follow-up duration was 29.2 months. The pain in the symptomatic side lower extremity (VAS score, 1.32±1.2) and the back (VAS score, 1.75±1.73) significantly improved (p=0.000 vs. baseline for both). The ODI improved significantly postoperatively (6.60±6.5; p=0.000 vs. baseline). Significant improvement in VAS pain and ODI scores were observed in patients receiving single or multi-segment decompression fusion with fixation (p<0.01).
Conclusion
Limited laminectomy and unilateral spinal decompression followed by bilateral pedicle screw fixation with fusion achieves satisfactory outcomes in patients with spinal stenosis and unilateral radiculopathy. This procedure is less damaging to structures that are important for maintaining posterior stability of the spine.
Lumbar spinal stenosis typically manifests itself as radiating pain and numbness in the lower extremity with or without back pain and/or intermittent claudication311). The condition has been traditionally treated with surgical decompression with good to excellent outcomes in approximately 80% of the patients16). Current prevailing approaches for lumbar spinal stenosis include laminectomy of the involved segment, minimally invasive bilateral decompression laminectomy in combination with pedicle screw fixation and fusion, and unilateral laminectomy with bilateral decompression and pedicle screw instrumentation. These approaches have overall yielded good outcomes. However, bilateral decompression and laminectomy are more invasive and may cause lumbar vertebral instability11), and the surgical procedure is complicated and is time-consuming, which may predispose to dural rupture and increase risk of complications that could aggravate radiculopathy. In addition, some lumbar spinal stenosis patients only have unilateral radiculopathy311) and the above approaches may not be fully applicable to this group of patients.
To address these deficiencies, we have performed unilateral laminectomy and decompression with bilateral pedicle screw instrumentation for lumbar spinal stenosis patients with unilateral radiculopathy. The purpose of this study is to report the outcomes of unilateral decompression and bilateral pedicle screw fixation with fusion for patients with lumbar spinal stenosis with unilateral radiculopathy. Our hypothesis is decompression of the asymptomatic side in patients with only unilateral lower extremity radiculopathy is unnecessary.
We retrospectively reviewed the surgical and radiological data of patients with lumbar spinal stenosis treated at the Department of Orthopedics Surgry, Peking University Third Hospital, Beijing, China between July, 2008 and September, 2011. A subject was included 1) if he or she had clinically and radiologically defined lumbar spinal stenosis9); 2) if unilateral radiating numbness and pain was present in the lower extremity with or without back pain, with or without intermittent claudication; 3) if thickening of the ligamentum flavum of the lumbar vertebrae was demonstrated on magnetic resonance imaging (MRI) without lumbar disc herniation or only symmetrical disc bulging; 4) if lumbar vertebral segments were demonstrable on X-ray images, with degenerative spondylolisthesis <grade I; 5) had received conservative management for more than 3 months; 6) 1 to 3 segments between L3 to S1 received decompression and fixation segment. Conservative management consisted of rest, non-steroid anti-inflammatory drugs, neurotrophic drugs, and epidural/nerve blocks. Exclusion criteria were : 1) no radiating pain in the lower extremity and if numbness was absent; 2) MRI or computed tomography (CT) findings were predominantly disc herniation, including lateral, central or far lateral lumbar disc herniation; 3) lumbar isthmic spondylolysis was present; 4) lumbar spondylolisthesis >grade I; 5) a prior history of lumbar surgery; 6) history of psychiatric disorders and drug or alcohol abuse; 7) bilateral radiculopathy. The study protocol was approved by Peking University Third Hospital Medical Science Research Ethics Committee. Patient consent was not required because of the retrospective nature of the study.
To determine the range of surgical decompression and fixation, patients were asked to describe the distribution of radiating leg pain and numbness. They were examined to determine if lower limb paralgesia and muscle weakness were present to clarify the range of neurological deficits. The range of ligamentum flavum hypertrophy shown on MRI studies and facet joint hypertrophy and spinal stenosis were assessed. Based on the aforementioned findings, the range of decompression and instrumentation was determined.
All surgeries were performed by a single surgeon with more than 20 years of spine surgery experience. In general, interbody fusion was chosen for single or double segment fusion, and posterolateral fusion was chosen for L3-S1 fusion. First, bilateral pedicle screws were inserted in the segment being instrumented. For unilateral decompression, the lamina and ligamentum flavum of the symptomatic side were excised to the root of the spinous process. Decompression up to the midline was done using a narrow osteotome and Kerrison rongeur at the base of the spinous process to partially relieve central canal stenosis. In single segment unilateral decompression, the inferior 1/3 of the superior lamina and the superior 1/4 of the inferior lamina of the symptomatic side were excised. In double segment unilateral decompression, the lamina of the symptomatic side between 2 segments was excised for contiguity of decompression. For lateral decompression in patients undergoing transforaminal lumbar interbody fusion, the symptomatic side superior and inferior facet joints of the decompressed segment were excised. After the superior and inferior lumbar endplates to be fused were curetted, an interbody fusion device of appropriate height was selected and the interbody space was filled with morselized bone. For posterolateral fusion, only the medial portion of the superior and inferior facet joints was excised, and the facet joint capsules with thickened inner linings and ligamentum flavum were excised with a Kerrison rongeur and bone curette. The part of the ligamentum flavum at the symptomatic side root of the spinous process was removed, and the nerve roots and the dura of the symptomatic side of the involved segment were decompressed and exposed. Otherwise, the lamina, the facet joint, and ligamentum flavum of the asymptomatic contralateral side were left intact. The spinous process and the interspinous ligaments in the midline were left intact also. The spinal canal, dura, and nerve roots of the asymptomatic contralateral side were not disturbed. Then, morselized autogenous bone or that mixed with morselized allogenous bone were grafted into the bilateral interspaces of the transverse processes that were decorticated. After the bilateral rods were connected and pedicle screws were tightened, the contralateral lamina of the asymptomatic side was decorticated, and the corresponding facet joint of the asymptomatic side was destroyed and morselized bone were grafted in.
The thickness of the ligamentum flavum of the involved segments was measured on axial T1-weighted or T2-weighted MRI images perpendicular to the spinal canal axis and parallel to the intervertebral space, where the ligamentum flava were seen along their entire length (Fig. 1). A line was drawn along the laminar side of the ligament curve, and along the side of the ligament facing the spinal canal, and the width of the ligamentum flavum was measured where it appeared the thickest. The thickness of ligamentum flavum was measured at the same place on both sides2). The paired t test was performed to compare the ligamentum flavum thickness of the symptomatic and asymptomatic side.
Patients were followed up at 3, 6, and 12 months after surgery by telephone interview, and once every year thereafter. The presence and duration of back pain, intermittent claudication, and radiating numbness and pain in the lower extremity were documented. Pain was evaluated using a visual analogue scale (VAS) where 0-3 indicates mild pain, which is tolerable and does not interfere with rest; 4-6 represents pain that interferes with rest, but is still tolerable; 7-10 indicates intolerable pain. VAS pain scores were collected from patients preoperatively, postoperatively, and at the last follow-up. The effect of pain on daily quality of life was assessed using the Oswestry Disability Index (ODI)10).
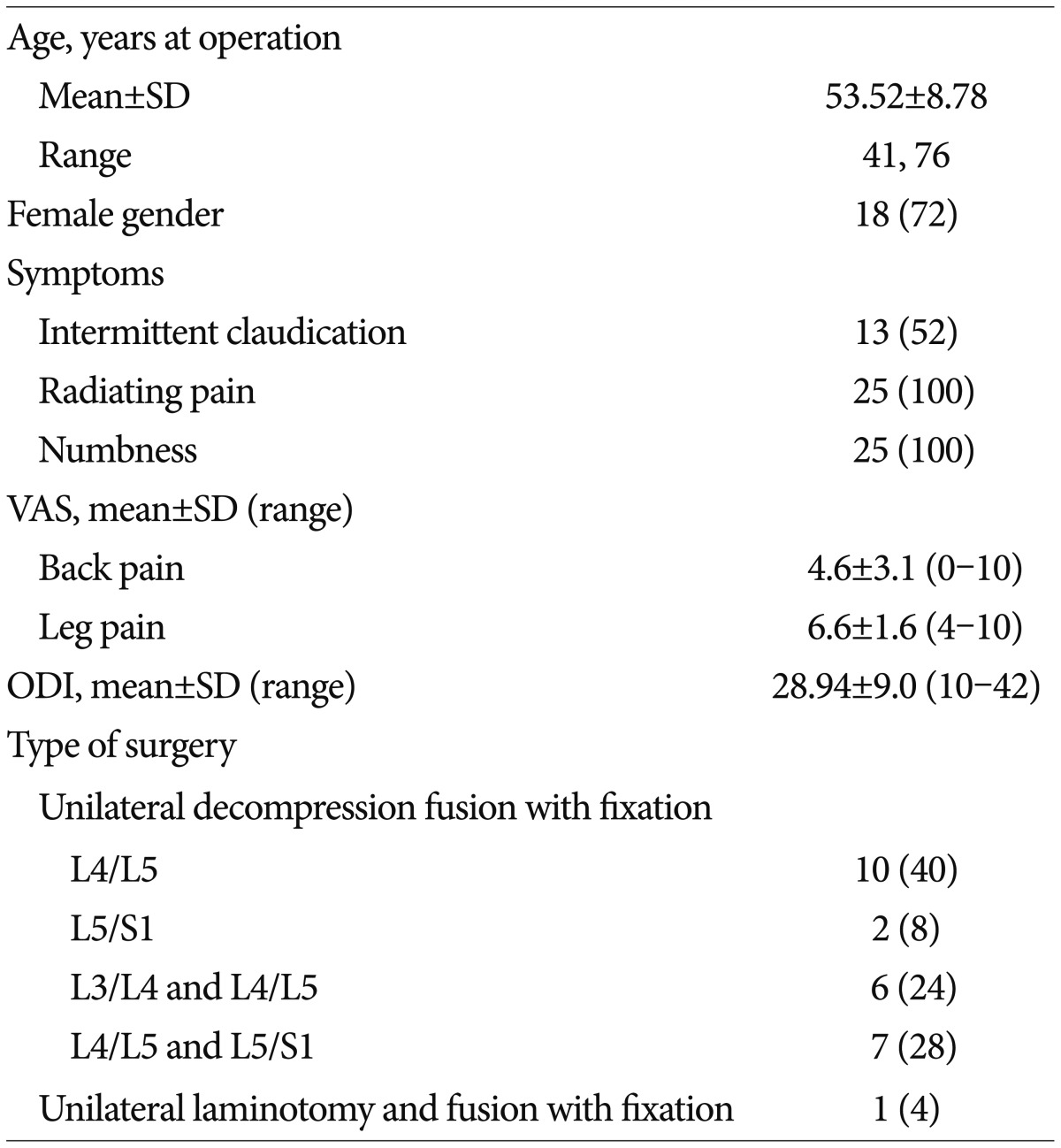
Twenty-five patients met the inclusion criteria and were included in the analysis. Patient demographic and baseline characteristics are shown in Table 1. The majority of the patients (72%, 18/25) were female, and the mean patient age was 53.52±8.78 years (range, 41 to 76 years). All patients had unilateral radiating leg pain and numbness of the lower extremity (mean duration, 12.14 months; range, 3 to 72 months) and 19 (76%) patients had back pain (mean duration, 75.9 months; range, 3 to 240 months). Thirteen (52%) patients had intermittent claudication. The mean preoperative VAS pain score was 6.6±1.6 (range, 4 to 10) for pain in the symptomatic lower extremity, and 4.6±3.1 (range, 0 to 10) for back pain. All patients had received a minimum of 3 months conservative treatment, and the average time of conservative management was approximately 12 months.
The thickness of the ligamentum flavum was measured in 39 segments and comparisons of ligamentum flavum thickness of the symptomatic side and asymptomatic side revealed no significant difference between the 2 sides (p=0.554).
Ten (40%) patients received unilateral decompression with bilateral fixation and fusion at L4/5; 2 (8%) received unilateral decompression with bilateral fixation and fusion at L5/S1; 6 (24%) underwent unilateral decompression with bilateral fixation and fusion at L3/4 and L4/5 (double segments); 7 (28%) underwent unilateral decompression with bilateral fixation and fusion at L4/5 and L5/S1 (double segments); and 1 (4%) received unilateral laminotomy at L3-5 and bilateral fixation and fusion at L3-S1 (Table 1). Twenty-two (88%) patients had transforaminal lumbar interbody fusion, 3 (12%) received simple posterolateral fusion, and 4 (16%) required the placement of an interspinous stabilization device (Wallis or Coflex) in the adjacent superior segment. There were no major complications. No obvious spinous process fracture was detected by plain X-ray. No patients experienced cerebrospinal fluid leakage after surgery. One patient developed a wound infection in the immediate postoperative period with full resolution within 6 months. No patients experienced numbness, pain, or weakness in the leg of the asymptomatic side.
The mean duration of follow-up was 29.2 months (range, 6.6 to 52.0 months). Pain in the symptomatic lower extremity (VAS pain score, 1.32±1.2) and the back (VAS pain score, 1.75±1.73) was significantly improved (p=0.000 vs. preoperative VAS scores for both). ODI scores also improved significantly postoperatively (6.60±6.5; p=0.000 vs. preoperative ODI score). According to the United States Food and Drug Administration criteria for significant functional improvement (increase of ≥15 points in ODI score), 88% (22/25) of our patients had a satisfactory outcome. Furthermore, significant improvement in the VAS and ODI scores were observed in patients receiving single or multi-segment decompression fusion with fixation (p<0.01) (Table 2).
A 42-year-old woman had back pain for 2 years accompanied by radiating pain in the left lower extremity for 1 year. No signs of radiculopathy of the lower extremity were observed. Preoperative MRI revealed bilateral ligamentum flavum thickening at L4/5 (thickness of the symptomatic (L)/asymptomatic (R) side of ligament=1.24) (Fig. 2A). Bilateral L4/5 pedicle screw with fixation was performed (Fig. 2B), and the left lamina and ligamentum flavum at L4/5 were partially excised followed by transforaminal lumbar interbody fusion. The right lamina and facet joint at L4/5 were grafted with morselized bone. At 14 months po-stoperatively her ODI score was 5 (baseline, 15), VAS pain score for left leg pain was 3 (baseline, 7), and VAS pain score for back pain was 2 (baseline, 6). No numbness of pain of the right lower extremity was reported. Follow-up MRI and CT scans revealed good decompression of the left side of the spinal canal at the space between L4 and L5, and the dura on the left side bulged well. Right ligamentum flavum thickening was not treated (Fig. 2C, D).
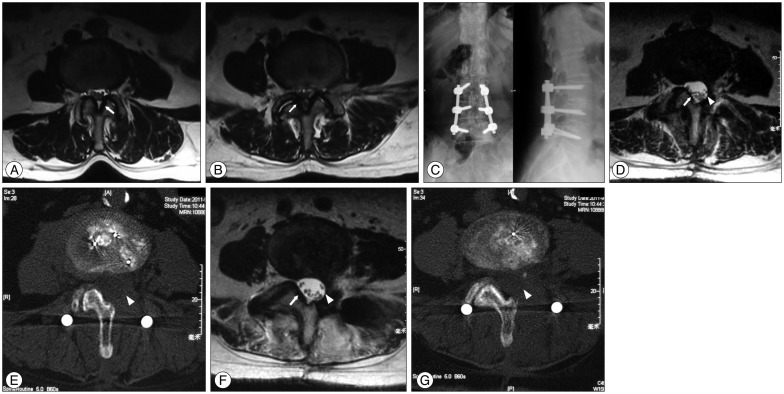
A 61-year-old female had intermittent back pain for more than 10 years, accompanied by posterolateral radiating pain of the left lower leg with intermittent claudication for more than 2 years. No signs of radiculopathy were found. MRI revealed L3/4 and L4/5 ligamentum flavum thickening [symptomatic (L)/asymptomatic (R) side ligament=1.19 at L3/4 and 0.68 at L4/5]. The left lamina and ligamentum flavum were partially excised (Fig. 3A, B), and transforaminal lumbar interbody fusion was performed. Bilateral pedicle screw fixation was done at L3 to L5, and the right laminae and facet joints at L3 to L5 were grafted with morselized bone (Fig. 3C). At 15 months postoperatively her ODI score was 14 (baseline, 24), VAS pain score for leg pain was 2 (baseline, 5), and VAS pain score for back pain was 1 (baseline, 3). No numbness or pain of the right lower extremity was reported. Follow-up MRI and CT scans revealed good decompression of the left side of the spinal canal at the space between L4 to S1, and the dura on the left side bulged well (Fig. 3D, E). Right ligamentum flavum thickening was not treated (Fig. 3F, G).
The results of the current study showed that limited unilateral lamina ligamentum flavum excision and limited unilateral spinal decompression followed by bilateral pedicle screw fixation with fusion achieved satisfactory outcomes in patients with spinal stenosis and unilateral radiculopathy. Extensive bilateral lamina decompression requires more extensive excision of the spinous process, the supraspinous ligament, and the interspinous ligament, which are important structures for maintaining posterior stability of the spine. The procedure described results in less damage to these important structures and reduces the risk of dural injury while providing good outcomes as reflected in improved VAS pain and ODI scores.
All of our patients only had unilateral lower extremity radiculopathy, Louis and Nazarian11) reported that of 350 cases of lumbar spinal stenosis, 67% had neurogenic intermittent claudication, slightly more than half (57%) had unilateral radiculopathy, and only 43% had bilateral radiculopathy of the lower extremity. Similar findings were reported by Amundsen et al.3) who observed that bilateral radiculopathy was seen in only 42% (42/100) of patients, and unilateral lower extremity radiculopathy in 58% with lumbar spinal stenosis.
We found no correlation between ligamentum flavum thickening and lower extremity radiculopathy, and patients with unilateral radiculopathy had a comparable ligamentum flavum thickness of the symptomatic side and the asymptomatic side. This indicates that the symptoms of radiculopathy occurred in the lower limb of either side were not correlated with the difference of ligamentum flavum thickness. Park et al.13) found a greater ligamentum flavum thickness in patients with spinal stenosis than in a control group, while other studies have shown normal thicknesses of the ligamentum flavum, ranging from 1.8 to 5 mm in healthy subjects41215). Lohman et al.10) reported correlation between the cross-sectional area of the spinal canal on CT and clinical symptoms in lumbar spinal stenosis patients. Sirvanci et al.17) also reported no correlation between stenosis of the spinal canal and ODI scores in patients with lumbar spinal stenosis. Haig et al.5) found that ligamentum flavum thickness at L4/5 correlated with age in healthy subjects, and was similar to that of lumbar spinal stenosis patients with lower extremity radiating pain and back pain. In addition, ligamentum flavum thickness in these patients showed no correlation with the degree of radiculopathy based on VAS pain and ODI scores.
Excessive mechanical stress in lumbar stenosis patients causes facet joint hypertrophy, ligamentum flavum thickening, and disc herniation due to segmental instability as a result of degenerative changes in the lumbar spine. Central canal stenosis and lateral recess stenosis ensue, with resultant radiating pain, numbness, and intermittent claudication in the lower extremity. In addition, back pain may develop as a result of facet joint hypertrophy and segment instability due to degenerative changes in the spine. Apart from ligamentum flavum thickening, disc herniation or bulging that impinges on the spinal canal, facet joint hypertrophy, and regional inflammation also contribute to radiculopathy. For these reasons, appropriate pedicle screw fixation and spinal fusion should be adopted for patients with lumbar spinal stenosis; the stability of the spine will be further damaged by extensive lumbar decompression, while the instability as a result of extensive decompression can be corrected by fixation and fusion.
Current surgery for lumbar spinal stenosis focuses on decompression of nerve impingement such as lamina and ligamentum flavum excision and spinal canal decompression. Extensive nerve decompression may inadvertently jeopardize lumbar vertebral stability, necessitating stabilization measures. As a result, decompression and pedicle screw instrumentation have emerged as the prevailing approach for lumbar spinal stenosis14). Extensive bilateral lamina decompression is complete decompression of all involved structures and requires more extensive excision of the spinous process, the supraspinous ligament and interspinous ligament, which are important structures for maintaining posterior stability of the spine in the early stage after pedicle screw instrumentation6). The supraspinous ligament and interspinous ligament oppose approximately 19% of extension stress, and full lamina decompression jeopardizes the ligament complexes in the posterior spine which predisposes to extension instability1). This may be offset by pedicle screw fixation with fusion. However, extensive decompression may cause excessive damage and lead to greater stress on the pedicle screws, which may lead to screw loosening and non-fusion. The situation becomes more important in elderly patients who are likely to have osteoporosis in whom loosening of screws and non-fusion are more common. In addition, extensive bilateral decompression, fixation, and bone grafting with fusion using the posterior approach are also associated with greater blood loss.
Hong et al.7) followed 53 lumbar stenosis patients who received unilateral or bilateral lamina decompression at L4/L5 for more than 3 years, and found that intraoperative blood loss and surgical time for unilateral decompression were less than that of bilateral lamina decompression, and unilateral laminotomy also yielded better long term stability. Studies by Kasai et al.8) and Yucesoy et al.18) reported that the mechanical strength of unilateral pedicle screw fixation is markedly inferior to that of bilateral pedicle screw fixation. A large proportion of lumbar stenosis patients are elderly and have osteoporosis of varying degrees, and it remains unclear whether unilateral pedicle screw fixation can provide reliable long-term fixation in these patients.
In lumbar stenosis, the lamina itself is not a direct cause of impingement while hypertrophied facet joints, thickened ligamentum flavum, and herniated discs cause stenosis and directly impinge on the nerve roots. Limited decompression thoroughly decompresses only the key components responsible for nerve root impingement including the hypertrophied facet joints, thickened ligamentum flavum, and herniated discs, thus avoiding extensive excision of the lamina. In our current series, we carried out limited unilateral laminotomy and decompression with bilateral pedicle screw fixation based on which side had lower extremity radiculopathy and clinical symptoms, but not based on ligamentum flavum thickening or facet joint hypertrophy as revealed by MRI. There does not appear to be a correlation between bilateral ligamentum flavum thickening and lower extremity radiculopathy. Surgical treatment of lumbar spinal stenosis is aimed at relieving patient symptoms and improving their quality of life. More emphasis should be placed on identifying the side with lower extremity radiating pain and decompression should be decided according to the side that has developed lower extremity radiculopathy, not solely by imaging findings of lumbar spinal canal stenosis.
In addition to ligamentum flavum hypertrophy and herniated disc, other causes of nerve damage in patients with lumbar stenosis include degenerative scoliosis and facet joints hyperplasia. Patients with a herniated disc protruding to only one side and those with degenerative scoliosis were excluded from this study.
There are limitations of this study that should be considered. The study was a retrospective review of medical records and the number of patients was relatively small. An argument could be made that the different fusion methods are too dissimilar to be included in the same treatment cohort. A similar argument could be made that patients having an interspinous spacer should be in a separate cohort. While there were some differences between the patients, the basic surgical principle of limited unilateral lamina ligamentum flavum excision and limited unilateral spinal canal decompression followed by bilateral pedicle screw fixation with fusion was used in all cases. Several surgical methods were used in the patients in this study; however, the results indicated that the unilateral decompression surgery was effective and adequate, and that bilateral decompression was not necessary. The postoperative bony fusion index was not reported, but the purpose of the surgery was to improve symptoms and this was reflected in the postoperative VAS and ODI scores. We did not evaluate how many patients with an initial diagnosis of stenosis had bilateral vs. unilateral symptoms, and we did we analyze the specific conservative treatments patients received. No control group was included; however, the comparison of the ligamentum flavum thicknesses showed that there was not a significant difference between the thickness on the symptomatic and non-symptomatic side. Lastly, further study is required to determine the contraindications of this surgical approach.
Limited unilateral lamina ligamentum flavum excision and limited unilateral spinal decompression followed by bilateral pedicle screw fixation with fusion achieves satisfactory outcomes in patients with spinal stenosis and unilateral radiculopathy. This procedure is less damaging to structures that are important for maintaining posterior stability of the spine, and reduces the risk of dural damage. Decompression should be decided according to the side of lower extremity radiculopathy, and not solely by imaging findings of lumbar spinal canal stenosis.
References
1. Adams MA, Hutton WC, Stott JR. The resistance to flexion of the lumbar intervertebral joint. Spine (Phila Pa 1976). 1980; 5:245–253. PMID: 7394664.

2. Altinkaya N, Yildirim T, Demir S, Alkan O, Sarica FB. Factors associated with the thickness of the ligamentum flavum : is ligamentum flavum thickening due to hypertrophy or buckling? Spine (Phila Pa 1976). 2011; 36:E1093–E1097. PMID: 21343862.
3. Amundsen T, Weber H, Lilleås F, Nordal HJ, Abdelnoor M, Magnaes B. Lumbar spinal stenosis. Clinical and radiologic features. Spine (Phila Pa 1976). 1995; 20:1178–1186. PMID: 7638662.
4. Capogna G, Celleno D, Simonetti C, Lupoi D. Anatomy of the lumbar epidural region using magnetic resonance imaging : a study of dimensions and a comparison of two postures. Int J Obstet Anesth. 1997; 6:97–100. PMID: 15321289.

5. Haig AJ, Adewole A, Yamakawa KS, Kelemen B, Aagesen AL. The ligamentum flavum at L4-5 : relationship with anthropomorphic factors and clinical findings in older persons with and without spinal disorders. PM R. 2012; 4:23–29. PMID: 22093441.

6. Hindle RJ, Pearcy MJ, Cross A. Mechanical function of the human lumbar interspinous and supraspinous ligaments. J Biomed Eng. 1990; 12:340–344. PMID: 2395361.

7. Hong SW, Choi KY, Ahn Y, Baek OK, Wang JC, Lee SH, et al. A comparison of unilateral and bilateral laminotomies for decompression of L4-L5 spinal stenosis. Spine (Phila Pa 1976). 2011; 36:E172–E178. PMID: 21192307.

8. Kasai Y, Inaba T, Kato T, Matsumura Y, Akeda K, Uchida A. Biomechanical study of the lumbar spine using a unilateral pedicle screw fixation system. J Clin Neurosci. 2010; 17:364–367. PMID: 20071182.

9. Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT, Toton JF, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J. 2013; 13:734–743. PMID: 23830297.

10. Lohman CM, Tallroth K, Kettunen JA, Lindgren KA. Comparison of radiologic signs and clinical symptoms of spinal stenosis. Spine (Phila Pa 1976). 2006; 31:1834–1840. PMID: 16845360.

11. Louis R, Nazarian S. Lumbar stenosis surgery : the experience of the orthopaedic surgeon. Chir Organi Mov. 1992; 77:23–29. PMID: 1587157.
12. Olszewski AD, Yaszemski MJ, White AA 3rd. The anatomy of the human lumbar ligamentum flavum. New observations and their surgical importance. Spine (Phila Pa 1976). 1996; 21:2307–2312. PMID: 8915063.
13. Park JB, Chang H, Lee JK. Quantitative analysis of transforming growth factor-beta 1 in ligamentum flavum of lumbar spinal stenosis and disc herniation. Spine (Phila Pa 1976). 2001; 26:E492–E495. PMID: 11679833.

14. Periasamy K, Shah K, Wheelwright EF. Posterior lumbar interbody fusion using cages, combined with instrumented posterolateral fusion : a study of 75 cases. Acta Orthop Belg. 2008; 74:240–248. PMID: 18564483.
15. Safak AA, Is M, Sevinc O, Barut C, Eryoruk N, Erdogmus B, et al. The thickness of the ligamentum flavum in relation to age and gender. Clin Anat. 2010; 23:79–83. PMID: 19941359.

16. Sengupta DK, Herkowitz HN. Lumbar spinal stenosis. Treatment strategies and indications for surgery. Orthop Clin North Am. 2003; 34:281–295. PMID: 12914268.
17. Sirvanci M, Bhatia M, Ganiyusufoglu KA, Duran C, Tezer M, Ozturk C, et al. Degenerative lumbar spinal stenosis : correlation with Oswestry Disability Index and MR imaging. Eur Spine J. 2008; 17:679–685. PMID: 18324426.

18. Yücesoy K, Yüksel KZ, Baek S, Sonntag VK, Crawford NR. Biomechanics of unilateral compared with bilateral lumbar pedicle screw fixation for stabilization of unilateral vertebral disease. J Neurosurg Spine. 2008; 8:44–51. PMID: 18173346.

Fig. 1
Schematic drawing of ligamentum flavum thickness measurement. Solid arrow indicates the ligamentum flavum and double white arrow indicates the thickest portion of the ligamentum flavum where measurement was made.
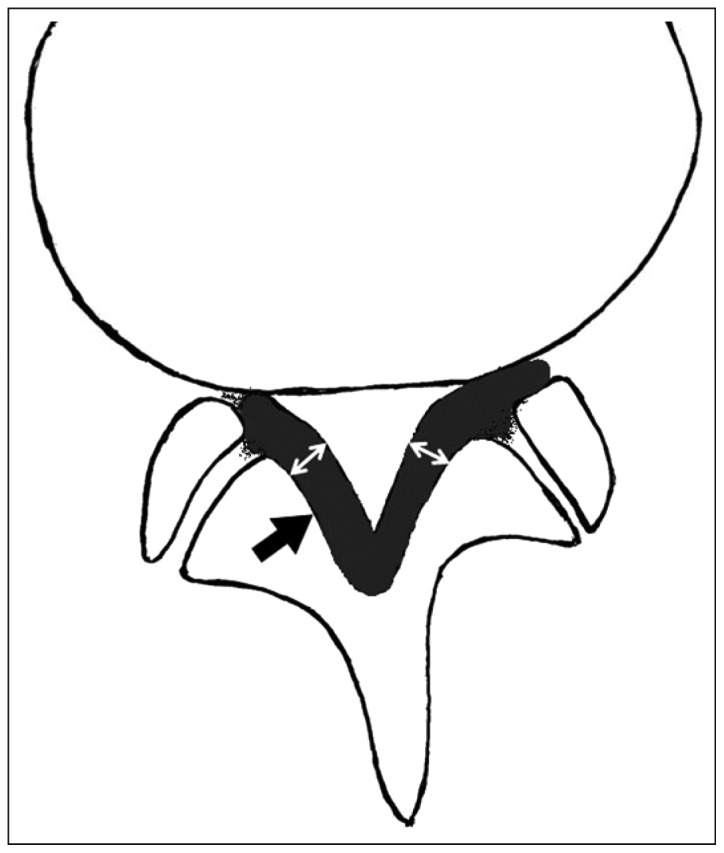
Fig. 2
A 42-year-old female with spinal stenosis accompanied by unilateral radiculopathy of the left lower extremity for 1 year. A : Preoperative MRI revealed thickening of the ligamentum flavum (by white arrow). The symptomatic (L)/asymptomatic (R) ratio of bilateral ligamentum thickness at L4/5=1.24. B : Bilateral L4/5 pedicle screw fixation, left decompression TLIF were performed. C : Postoperative MRI. The white triangle points to L4/L5 with left hemilaminectomy and excision of the ligamentum flavum. White arrow shows the intact right side. D : Postoperative CT showed left hemilaminectomy (arrow).
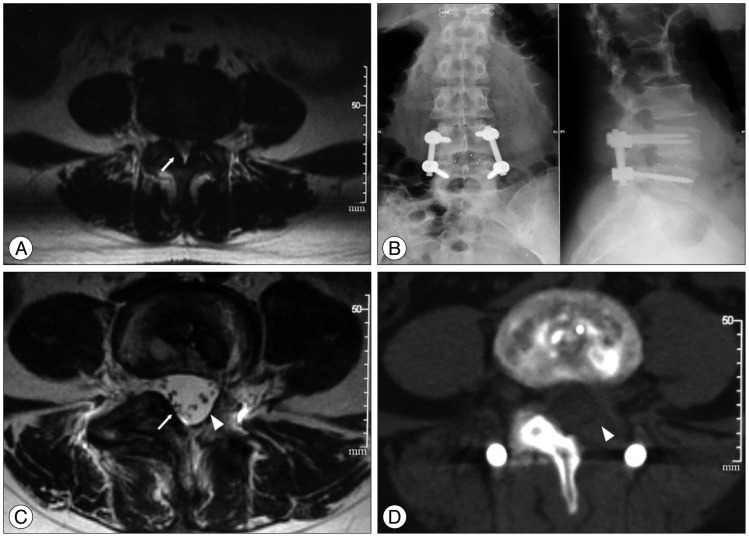
Fig. 3
A 61-year-old female with intermittent back pain for more than 10 years, accompanied by posterolateral radiating pain of the left lower leg with intermittent claudication for more than 2 years. A : Preoperative MRI revealed bilateral L3-4 ligamentum flavum thickening. White arrow indicates thickness on the left side was greater than the right side. B : Preoperative MRI revealed bilateral L4-5 ligamentum flavum thickening. White arrow indicates thickness on the right side was greater than on the left side. C : Bilateral pedicle screw fixation was performed at L3 to L5, and the right laminae and facet joints at L3 to L5 received morselized bone graft. L3-5 left lamina and ligamentum flavum were partially excised, and transforaminal lumbar interbody fusion was performed. D : Postoperative MRI. The white triangle points to L4/5 with left hemilaminectomy and excision of the ligamentum flavum. White arrow shows the normal right side. E : Postoperative MRI. The white triangle points to L3/4 with left hemilaminectomy and excision of the ligamentum flavum. F : Postoperative MRI of L4/5 intervertebral space. The pointed white triangle indicates the left (symptomatic) vertebral plate and the excised ligamentum flavum. Dural sac decompression and bulging are satisfactory. White arrow indicates the right (asymptomatic) vertebral plate and ligamentum flavum. G : Postoperative CT scan of L4/5 intervertebral space. The pointed white triangle indicates left (symptomatic) vertebral plate and the excised ligamentum flavum. Dural sac decompression and bulging are satisfactory.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download