Abstract
Intramuscular myxoma (IM) is a benign neoplasm of mesenchymal origin. We report a rare case of IM which was located in the lumbosacral paraspinal muscles. A 62-year-old female patient presented with progressive low back pain for 2 months, and the radiologic findings showed a large mass (4.0×3.5×6.5 cm) in the right lumbosacral paraspinal area. Total resection of the tumor was performed and the symptom was nearly resolved after surgery. Although the immuno-histopathological analysis was consistent with IM, there were some different findings from typical pathological characteristics of IM in this case. Firstly, the symptomatic change of the mass took relatively short time (less than 3 months), and this change was accompanied by partial calcification inside the mass. Moreover, iatrogenic interruption of paravertebral muscle by the other previous operation might be the promoting factor of the fibrous dysplasia, which can explain the pathogenesis of IM. To our knowledge, this is the eighth case of the lumbar paraspinal myxoma reported in the literatures and the first case in Asian population.
Myxoma is a benign neoplasm of mesenchymal origin composed of undifferentiated stellate cells in a myxoid stroma, which were differentiated into altered fibroblasts and lost their ability to produce normal collagen18). Myxoma can arise in a variety of locations; heart, subcutaneous and aponeurotic tissues, bone, genitourinary tract and skin, etc. The most frequent site for myxoma is the heart, and bony myxoma is almost exclusively limited to the jaws and palate, representing 40-50% of all head and neck myxomas216). The soft tissue myxoma is rare, and occurs mostly in the large skeletal muscles. The myxomas that arise in the skeletal muscles are generally called intramuscular myxomas (IMs). The most of IMs are detected in the fourth to sixth decades of life with slight female predominance16). IM accounts for about 3-17% of the all myxomas, and the incidence is about 1 case per million population per a year51823).
To our knowledge, we report the eighth case of a myxoma developed within the lumbosacral paraspinal muscle (including thoracolumbar paraspinal muscle), which had some different characteristics from the typical IM, and brief review of the literature will be followed.
A 62-year-old female was referred to our hospital for mass-like lesion detected on magnetic resonance imaging (MRI) of her spine. She presented with low-back pain just for 3 months without radiating leg pain, and the symptom was slowly progressive. She had a medical history for hypertension, and had no history of trauma. But, interestingly, she had the previous history of bone harvest on the right posterior superior iliac spine (PSIS) for the cervical fusion operation 15 years ago in the other hospital. Physical examination revealed a large palpable mass on the right paraspinal area in the lumbosacral region, but there was no associated tenderness in this region. Her neurologic examination at the time of admission was fully normal, and there was no abnormal finding on the laboratory tests and the electrophysiological studies such as electromyography (EMG) and somatosensory evoked potential (SSEP).
MRI demonstrated a multi-lobulated mass in the right lumbosacral paraspinal muscles in contact with the posterior elements of the L4 and L5 vertebra (Fig. 1). This well-circumscribed mass was measured approximately 4.0×3.5×6.5 cm in size, and the lesion was hypointense on T1-weighted image (T1WI) and hyperintense on T2-weighted image (T2WI). There were heterogenously enhancing foci inside the mass with peripheral and septal enhancement on the post-contrast T1WI.
On computed tomography (CT) scan of the lumbosacral region, this mass had low density and some calcification particularly on the inferior portion of the mass (Fig. 2A, B). There was no bony destruction or invasion around the mass. In the process of a full diagnostic workup, we found her previous abdominal CT images in picture archiving computer system (PACS), which had been performed for evaluation of her abdominal pain 4 months ago (Fig. 2C, D). In the previous abdominal CT, although it was slightly smaller than the mass of recent lumbar CT, the hypodense lesion was also seen at the same area. It was notable that calcification inside the mass was not detected on the previous abdominal CT.
We planned to conduct the complete excision, instead of simple biopsy (for example, CT-guided biopsy), because the tumor was not only symptomatic, but also the operation had fairly limited risk to the patient.
Surgical resection was accomplished through a paramedian longitudinal incision over the tumor site. The mass was easily dissected from the surrounding muscle and excised en bloc. The tumor was encapsulated and lobulated with grayish white surface, and there was no evidence of the infiltration or invasion into the surrounding bony structures. Grossly, the specimen contained gelatinous material and some calcified portion (Fig. 3).
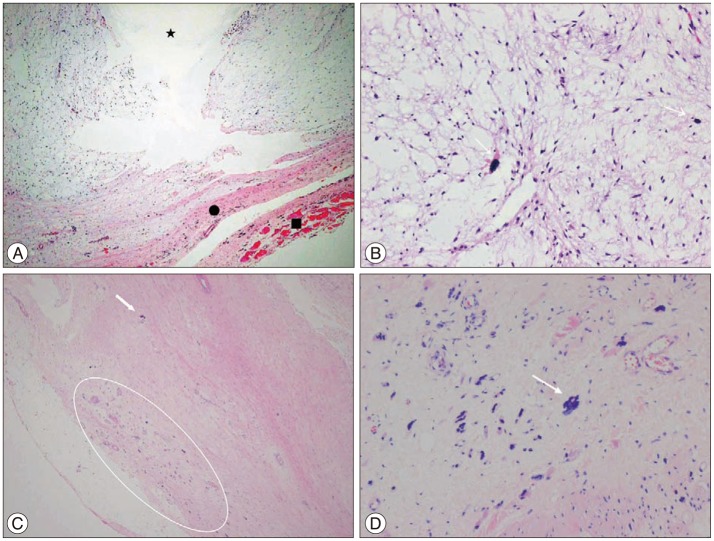
According to the frozen biopsy during the operation, the mass was revealed to myxoid tumor, and the final histopathological findings were consistent with intramuscular myxoma. This mass was composed of prominent myxoid stroma with a distinct presence of spindle and stellate cells, and while pyknotic nuclei and karyorrhectic nuclei were also seen (Fig. 4). Numerous micro-calcifications were also found, especially in the peripheral capsular area of the tumor. There was no evidence of mitotic activity, hemorrhage or necrosis.
The patient was neurologically free and experienced complete relief of her low-back pain postoperatively.
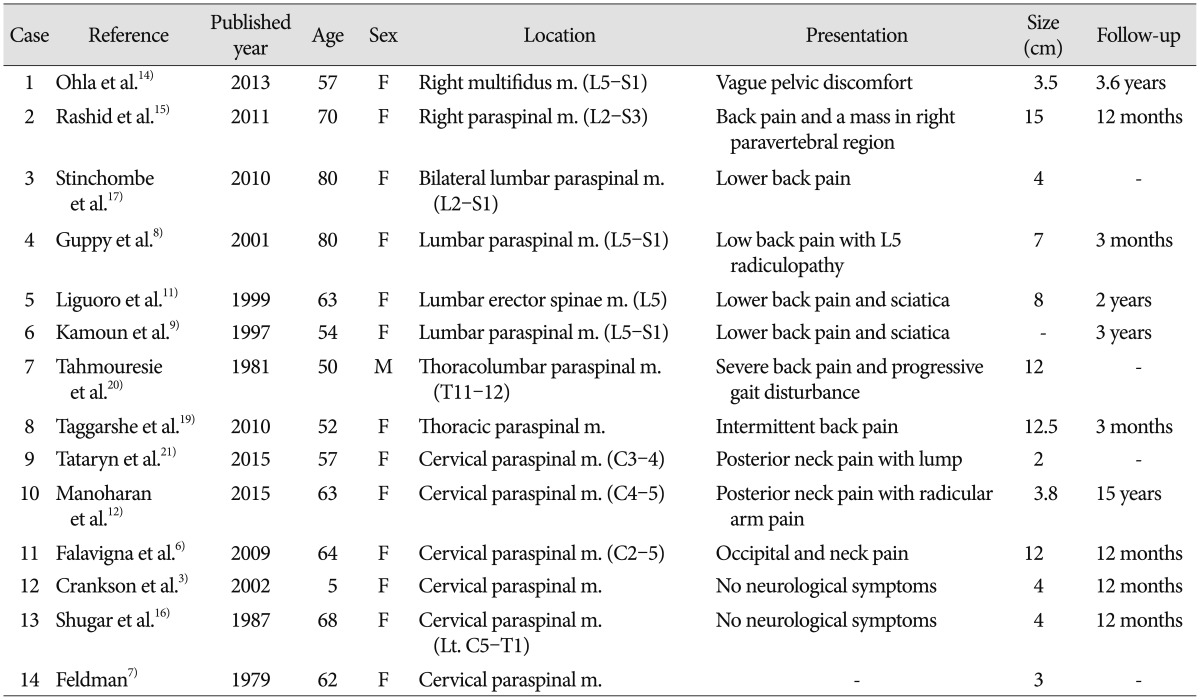
Since Stout et al18). outlined the diagnostic criteria and defined myxoma at 1948, the intramuscular myxoma has been known as the most rare sub-type in these tumor category. IMs have been reported at the various locations such as thighs, buttocks, upper limbs, shoulders, and paravertebral area. Of those IMs, paraspinal regions are the most uncommon site, and so far, only 14 cases of paraspinal IMs have been reported. And to the best of our knowledge, this report is just the eighth case of paraspinal IM in the lumbosacral area including one case of thoracolumbar lesion, and the first case in Asian population (Table 1)891114151720).
IMs usually appear as well-circumscribed homogeneous low-density lesions within the skeletal muscle on CT scan, and have low-signal intensity on T1WI and high-signal intensity on T2WI. Bancroft el al.1) described that the peri-tumoral fat rind on T1WI and increased signal in the adjacent muscle on T2WI are the most reliable radiologic features for distinguishing intramuscular myxoma from other myxoid tumor. But in this case, this finding was not definite on the MRI.
On gross inspection, the tumor has usually oval shape and shows well-circumscribed appearance, however its fibrous tissue often has incomplete pseudocapsule to result in infiltration of adjacent musculature510). And in general the tumor has a glistering gray-white appearance and contains gelatinous material and cyst filled with fluid inside the mass.
Histologically, IMs are composed of well-localized myxomatous connective tissue surrounded by a collagenous fibrous connective tissue22). IMs are often confused with other pathologic conditions such as ganglion or neurofibroma, and furthermore, with other mucoid sarcomas such as liposarcomas, chondrosarcomas, low-grade fibromyxoid sarcoma and malignant histiocytomas, because these sarcomas are also accompanied by the myxomatous degeneration. However, several critical clues had been presented, which help to distinguish IMs from other myxoid lesions. First, IMs have poor vascularization and a paucity of cells (lipoblasts or chondroblasts), in contrast to myxoid liposarcoma which has a rich, delicate, plexiform capillary vascular network. Secondly, IMs lack nuclear atypia, necrosis, and prominent mitotic activity. In addition, on the enhanced MRI, soft tissue sarcomas showed heterogeneity, intense enhancement, septation, ill-defined margins and invasion of adjacent structure against the IMs. Moreover, IMs often do not have a true capsule, and therefore could infiltrate to the adjacent striated muscle, resulting in muscle atrophy which appear as a peri-tumoral fat rind on T1WI. Additionally, Doyle et al.4) presented the MUC4 protein as a specific marker for distinguishing from low-grade fibromyxoid sarcroma.
IMs usually present as a solitary slow growing painless mass, however multiple myxomas can occur on rare specific condition, for example, Mazabraud's syndrome. The clinical manifestations of IMs generally are non-specific, but rather presenting symptoms depend on the affected locations. In our case, the patient also presented with ambiguous low back pain and this symptom was resolved after total resection of the tumor.
In general, IMs are known as slowly growing and painless tumors, whereas there are some differences from typical natures of IMs in this case. First, it had been just asymptomatic mass, but it developed to symptomatic lesion in a very short time (about 3 months). There was demonstrable difference in size of the tumor; width×length×height=3.0×3.0×5.4 cm to 4.0×3.5×6.5 cm. In addition, a new calcification inside the mass was accompanied with tumor growth, while there is no internal calcification in most cases of IM. Third, the location of IM was adjacent to the previous operation site (iliac bone harvest site). Although the pathogenesis of IMs remains obscure, there are several theories for explaining the pathogenesis. According to one of the theories, stellate cells may be altered fibroblasts that fail to produce mature collagen5). By Glazunov and Puckov, "viral origin" was proposed as the other pathogenesis23). Wirth et al.24) proposed the fibrous dysplasia as another theory for the pathogenesis of IMs, and fibrous dysplasia usually precedes the IMs by several years. We assumed that interruption of paraspinal muscles by previous operation could induce fibrous dysplasia to arise IM.
Though there was no report about the prevalence by race due to the rarity of the incidence of IMs, previous many reports were almost confined to the western population. Our case is the first case of IM in Asian people, which developed in the lumbosacral paraspinal musculature.
The clinical course of IMs is known to be nearly benign, and the treatment for IMs is the total surgical resection. There is no report of metastasis or malignant change, but occasionally local recurrence resulting from incomplete resection has been reported6913). Therefore, if possible, wide excision with clean margins is recommended to avoid local recurrence, since IMs have an infiltrative tendency to surrounding muscles.
We report the first case of the paraspinal intramuscular myxoma developed in the lumbosacral area in Asian population. Intramuscular myxomas are uncommon benign tumors, especially in the paraspinal area, and moreover it is difficult to make a diagnosis before operation because of the lack of characteristic clinical history and radiographic findings, however, neurosurgeons should be aware of this entity.
References
1. Bancroft LW, Kransdorf MJ, Menke DM, O'Connor MI, Foster WC. Intramuscular myxoma : characteristic MR imaging features. AJR Am J Roentgenol. 2002; 178:1255–1259. PMID: 11959742.
2. Canalis RF, Smith GA, Konrad HR. Myxomas of the head and neck. Arch Otolaryngol. 1976; 102:300–305. PMID: 1267724.

3. Crankson SJ, Al Namshan M, Al Mane K, Bamefleh H. Intramuscular myxoma : a rare neck mass in a child. Pediatr Radiol. 2002; 32:120–122. PMID: 11819080.
4. Doyle LA, Möller E, Dal Cin P, Fletcher CD, Mertens F, Hornick JL. MUC4 is a highly sensitive and specific marker for low-grade fibromyxoid sarcoma. Am J Surg Pathol. 2011; 35:733–741. PMID: 21415703.

5. Enzinger FM. Intramuscular myxoma; a review and follow-up study of 34 cases. Am J Clin Pathol. 1965; 43:104–113. PMID: 14253111.

6. Falavigna A, Righesso O, Volquind D, Teles AR. Intramuscular myxoma of the cervical paraspinal muscle. Eur Spine J. 2009; 18(Suppl 2):245–249. PMID: 19301043.

7. Feldman PS. A comparative study including ultrastructure of intramuscular myxoma and myxoid liposarcoma. Cancer. 1979; 43:512–525. PMID: 421179.

8. Guppy KH, Wagner F, Tawk R, Gallagher L. Intramuscular myxoma causing lumbar radiculopathy. Case report and review of the literature. J Neurosurg. 2001; 95(2 Suppl):260–263. PMID: 11599850.
9. Kamoun N, Zouari M, Siala M, Karray S, Douik M, Litaiem T, et al. [Intramuscular myxoma. Apropos of two cases]. Rev Chir Orthop Reparatrice Appar Mot. 1997; 83:278–282. PMID: 9255366.
10. Kindblom LG, Stener B, Angervall L. Intramuscular myxoma. Cancer. 1974; 34:1737–1744. PMID: 4426032.

11. Liguoro D, Viejo-Fuertes D, Vital A, San Galli F, Dautheribes M, Guerin J. [Intramuscular myxoma. A case of myxoma of the spinal erector muscle]. Neurochirurgie. 1999; 45:54–57. PMID: 10374236.
12. Manoharan SR, Shaw AB, Arnold CA, Farhadi HF. Infiltrative intramuscular myxoma of the cervical spine : a case report. Spine J. 2015; 15:e1–e4. PMID: 25264316.
13. Nielsen GP, O'Connell JX, Rosenberg AE. Intramuscular myxoma : a clinicopathologic study of 51 cases with emphasis on hypercellular and hypervascular variants. Am J Surg Pathol. 1998; 22:1222–1227. PMID: 9777984.
14. Ohla V, Ciarlini PD, Goldsmith JD, Kasper EM. Cellular myxoma of the lumbar spine. Surg Neurol Int. 2013; 4:82. PMID: 23869282.

15. Rashid A, Abdul-Jabar HB, Karmani S, Rezajooi K, Casey AT. Giant paravertebral myxoma. Eur Spine J. 2011; 20(Suppl 2):S138–S142. PMID: 20495934.

16. Shugar JM, Som PM, Meyers RJ, Schaeffer BT. Intramuscular head and neck myxoma : report of a case and review of the literature. Laryngoscope. 1987; 97:105–107. PMID: 3796168.
17. Stinchcombe S, Kochhar R, Malkan D. Intramuscular myxoma of the paraspinal musculature. J Med Cases. 2010; 1:42–46.

18. Stout AP. Myxoma, the tumor of primitive mesenchyme. Ann Surg. 1948; 127:706–719. PMID: 18917127.
19. Taggarshe D, Raheja S, Yoo S, Mittal V. Intramuscular myxoma : a rare back mass. Am Surg. 2010; 76:1303–1304. PMID: 21140704.
20. Tahmouresie A, Farmer PM, Stokes N. Paraspinal myxoma with spinal cord compression. Case report. J Neurosurg. 1981; 54:542–544. PMID: 7205357.
21. Tataryn Z, Tracy J, Tsang C, Wu J, Heilman CB, Wein RO. Intramuscular myxoma of the cervical paraspinal musculature : case report and review of the literature. Am J Otolaryngol. 2015; 36:273–276. PMID: 25481300.

22. Tomich CE. Oral focal mucinosis. A clinicopathologic and histochemical study of eight cases. Oral Surg Oral Med Oral Pathol. 1974; 38:714–724. PMID: 4140487.
23. Tse JJ, Vander S. The soft tissue myxoma of the head and neck region--report of a case and literature review. Head Neck Surg. 1985; 7:479–483. PMID: 4044268.

24. Wirth WA, Leavitt D, Enzinger FM. Multiple intramuscular myxomas. Another extraskeletal manifestation of fibrous dysplasia. Cancer. 1971; 27:1167–1173. PMID: 5581510.

Fig. 1
Preoperative magnetic resonance images. The multi-lobulated mass was located within the right lumbosacral paraspinal muscles in contact with the posterior elements of the lumbosacral vertebra. This large mass measured approximately 4.0×3.5×6.5 cm in size, and the lesion was hypointense on T1-weighted images (B) and hyperintense on T2-weighted images (A and D). On the post-contrast images (C and E), there was heterogenously enhancing foci inside the mass with peripheral and septal enhancement.
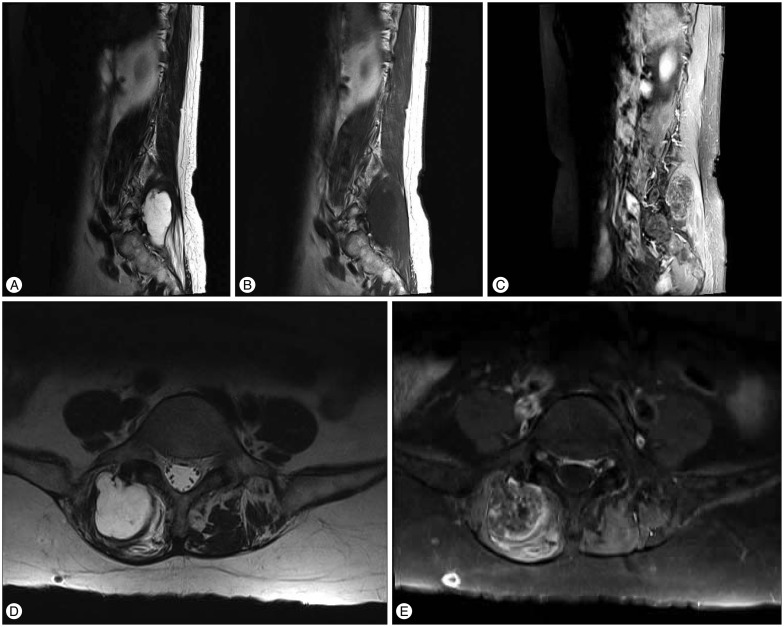
Fig. 2
Comparing the preoperative lumbar spine CT (A and B) with the previous abdominal CT (C and D). Note that the calcification in the inferior portion of the mass (A and B), which was not detected on the abdominal CT examined 4 months ago.
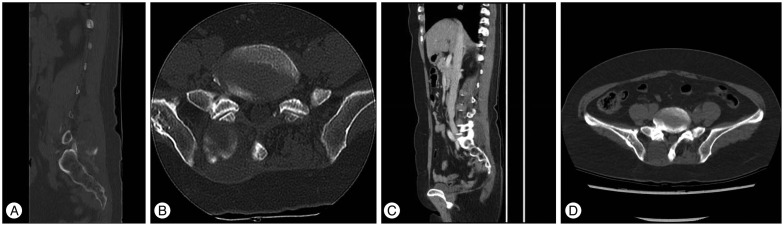
Fig. 3
Intraoperative photographs. The mass was identified through a paramedian longitudinal incision and was excised en bloc. Partial calcification was detected inside the tumor (asterisks).
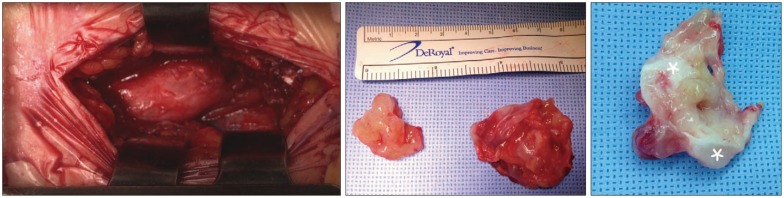
Fig. 4
Microscopic findings of the paraspinal myxomas. A : Myxoid hypocelluar lesion with fibrous capsule (circle). Note the microcystic change in mass (star). Degenerated skeletal muscle fiber (square) also identified (H&E, ×40). B : Bland-looking spindle to stellate cells in bluish myxoid stroma. Note the pyknotic nuclei and microcalcification (arrow) (H&E, ×200). C : Numerous karyorrhectic nuclei (circle) and microcalcification (arrow) in periphery-capsular area of tumor, which was seen in CT (H&E, ×40). D : Numerous karyorrhectic nuclei and microcalcification (arrow) in periphery-capsular area of tumor (H&E, ×200).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download