Abstract
Objective
To correct apical vertebral rotation for adolescent idiopathic scoliosis (AIS), direct vertebral derotation (DVD) or simple rod rotation (SRR) might be considered. The aim of the present study is to introduce the surgical experiences of AIS by a Korean neurosurgeon and to evaluate the effectiveness of SRR for apical vertebral rotation.
Methods
A total of 9 patients (1 male and 8 females) underwent scoliosis surgery by a neurosurgeon of our hospital. The Lenke classifications of the patients were 1 of 1B, 2 of 1C, 1 of 2A, 1 of 2C, 3 of 5C and 1 of 6C. Surgery was done by manner of simple rod rotation on the concave side and in situ coronal bending. Coronal Cobb's angles, vertebral rotation angles and SRS-22 were measured on a plain standing X-ray and CT before and after surgery.
Results
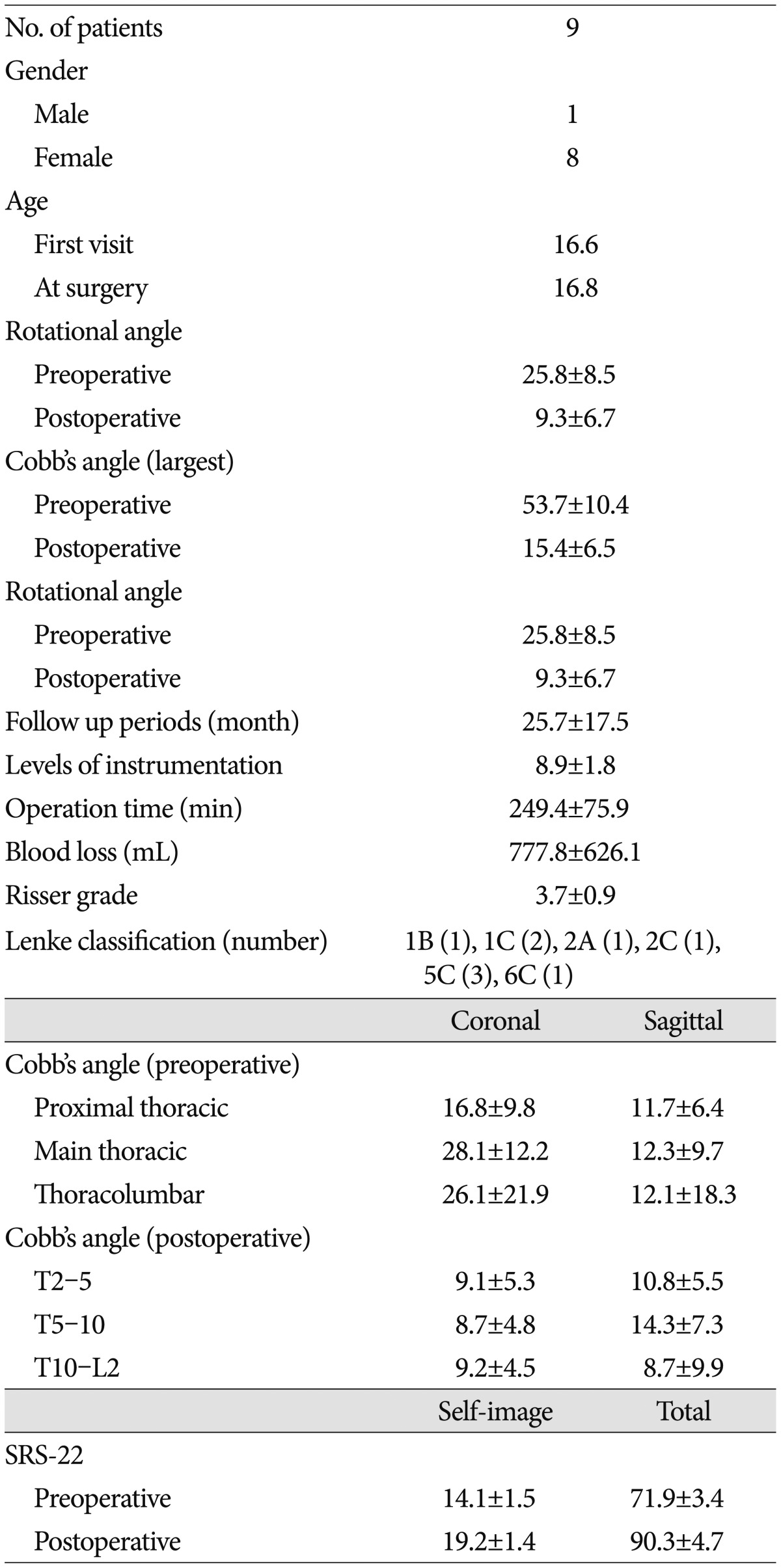
The mean follow up period was 25.7 months (range : 5–52). The mean number of screw positioning level was nine (6–12). The mean age was 16.4 years (range : 13–25) at surgery. The mean Risser grade was 3.7±0.9. The apical vertebral rotation measured from the CT scans was 25.8±8.5° vs. 9.3±6.7° (p<0.001) and the Coronal Cobb's angle was 53.7±10.4° vs. 15.4±6.5° (p<0.001) preoperatively and postoperative, respectively. The SRS-22 improved from 71.9 preoperatively to 90.3 postoperatively. There were no complications related with the operations.
Adolescent idiopathic scoliosis (AIS) is scoliosis in patients between 10 and 18 years of age which has originated from an unknown cause. Shoulder asymmetry, waistline asymmetry, body shift and rib prominence are prominent in AIS and these factors created patients dissatisfaction their body appearance and emotional stress. Mostly AIS is managed conservatively including brace utilization, and patient requiring surgical treatment is uncommon in Korea. A Surgical approach for AIS is unfamiliar for Korean neurosurgeons but surgical trials for deformity, including AIS, are mounting.
The surgical reduction method of AIS is recommended anteriorly or posteriorly such as via the direct vertebral derotation (DVD) and simple rod rotation (SRR) techniques. Direct vertebral derotation might acquire curve correction as well as vertebral body rotation but it is also technically demanding. SRR can correct the curve in a coronal view but it is a limited option to correct for vertebral body rotation.
The aims of this study are to introduce the surgical experiences and to evaluate the effectiveness of SRR to correct for curve and rotate of the vertebral bodies in AIS.
From 2010 to 2014, a total of 9 patients (1 male and 8 females) with AIS were treated surgically by a neurosurgeon of our hospital and were enrolled in this study. These patients, who completed our postoperative evaluations with tools including X-rays, CTs and clinical SRS-22 outcomes scoring, were selected for the study. The mean age was 16.2 years (range of 13–24) at first visit our hospital and 16.4 years (range of 13–25) at surgery. Two patients (Case 5 and 8) had been diagnosed AIS in other hospital previously and visited our hospital after several years and undergone surgery. This might make misunderstanding in AIS diagnosis. The majority of patients (40%) had visited clinics because of suggestions from their parents or friends. The mean period from first visit to surgery was 5.6 months (range of 1–12). Surgery was done by manner of simple rod rotation on the concave side and in situ coronal bending.
The Coronal Cobb's angles were measured on plain standing radiographs before and after surgery. The vertebral rotation angles were also measured on the apical vertebra on axial images of computed tomography (CT) before and after surgery. A questionnaire of the scoliosis research score (SRS-22) was surveyed preoperatively and postoperatively. Thoracic or thoracolumbar kyphosis, and bone maturation using a Risser grade were also checked.
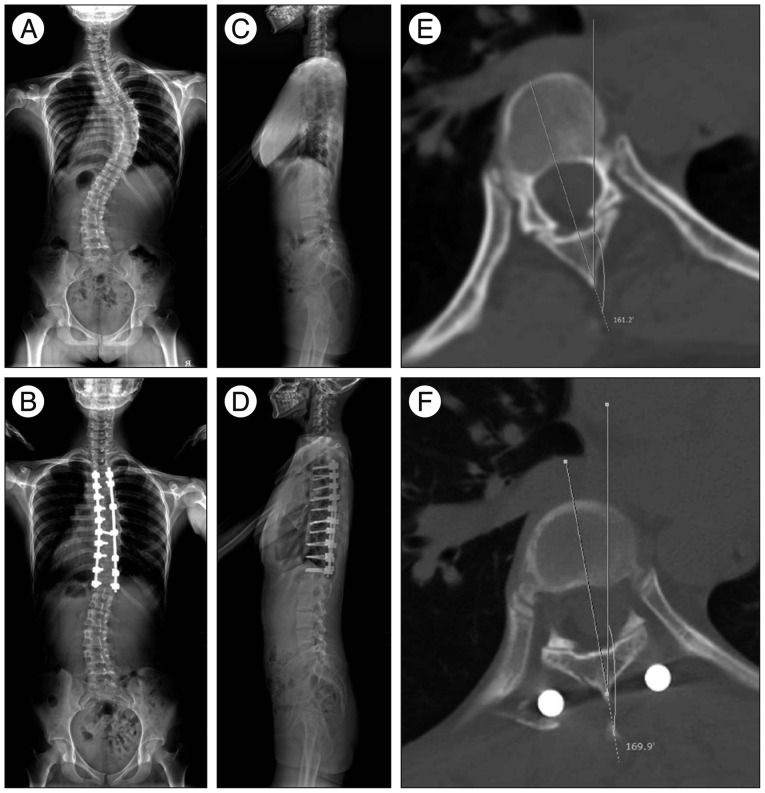
Vertebral body rotation is measured in the axial plane of computed tomography (CT)6). Vertebral rotation is an angle formed by two lines; one line joins the junction of the inner surfaces of two laminae and the midpoint of the posterior surface of the vertebral body, and the second line is the vertical plane of the computed tomographic image. In this study, the vertebral rotation angles of the patients were measured before and after surgery (Fig. 1). The correction rate of the rotation angles was calculated as the percentage between correction amount and preoperative angle. Operation time and blood loss were confirmed. All surgeries were conducted via monitoring of the electrophysiologic status, intraoperatively.
Statistical analysis was performed using the paired t-test, and a p<0.05 was considered statistically significant. R 3.0 was used for the statistical analysis.
The patient was prone positioned. The segmental and multi-level pedicle screws were inserted on both the concave and the convex sides of the vertebrae. We preferred to use polyaxial screws. A titanium alloy rod contoured to the normal sagittal contour of the instrumented segment was set in the concave side.
Following rod insertion, the caps were inserted loosely over the screws. Using rod holders, the correction rod was rotated 90° to transform the scoliosis into a kyphosis at the thoracic spine and a lordosis at the lumbar spine, restoring the sagittal profile in the corrected position. Correction of the deformity is performed solely by SRR with further additional compression or distraction. Straightening of the contoured rod occurs during the process of SRR. When a rod straightens, we remove it rebend it to an over bent shape, and then reinsert it. This is done until the desired sagittal curve is obtained. Two rods were finally fixed and the final adjustment was made via a portable X-ray with additional in situ bending and compression and distraction. As the rod is just supportive at the convex side in the thoracic and the concave side in the lumbar, the rod is bent conforming to the shape of the corrected curve and placed in situ without forceful manipulation. All patients were recommended to have active ambulation without a brace postoperatively on day 1. Standing posteroanteriorly, lateral radiographs were taken 1, 3, 6, and 12 months after surgery and a CT was checked to review proper screw position and the degree of rod rotation at 1 month postoperative periods.
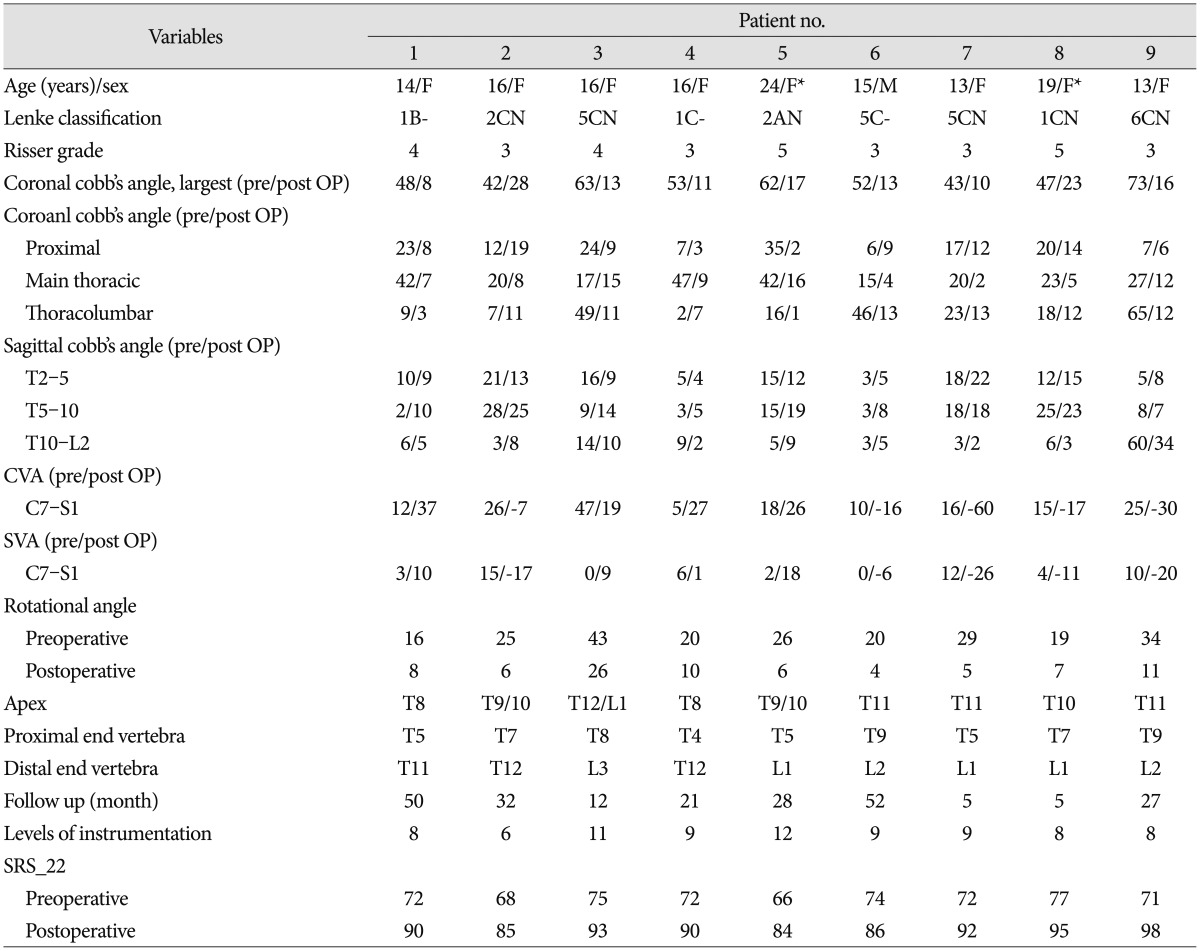
Demographic characteristics of all patients are summarized in Table 1.
The Lenke classifications of the patients were 1 of 1B, 2 of 1C, 1 of 2A, 1 of 2C, 3 of 5C and 1 of 6C. The proximal end vertebra was ranged from T4 to T9 and the distal end vertebra was ranged from T11 to L3. The mean follow up period was 25.7±17.5 (range of 5–52) months. The mean number of screw positioning levels was nine (range of 6–12). The mean operation time was 249.4 mins and the mean amount of blood loss was 777.8 mL. There were no complication perioperatively. Intraoperative electrophysiologic monitoring did not show any change during the operation. The mean Risser grade was 3.7±0.9.
The mean coronal Cobb's angle of the major curve was 53.7° before operation and 15.4° at the last follow-up after surgery, respectively. After surgery, the curve of spine had improved significantly (p=0.00) (Table 2). The preoperative and postoperative coronal Cobb's angles were 16.8±9.8° and 9.1±5.3° in the proximal thoracic, 28.1±12.2° and 8.7±4.8° in the main thoracic, and 26.1±21.9° and 9.2±4.5° in the thoracolumbar, respectively. The preoperative and postoperative sagittal Cobb's angle were 11.7±6.4° and 10.8±5.5° in T2–5, 12.3±9.7° and 14.3±7.3° in T5–10, 12.1±18.3° and 8.7±9.9° in T10-L2, respectively. The rotational angles were 25.8±8.5° before operation and 9.3±6.7° at the last follow-up after surgery, respectively (p=0.00) (Table 2, Fig. 1). The postoperative vertebral rotational angle also significantly differed compared preoperatively (p=0.00). The correction rate of the rotation was 64.5%.
AIS is the most common subtype of scoliosis and involves a complex three dimensional deformity in the coronal, sagittal and axial planes. In the coronal plane, the alignment of the vertebral bodies is laterally deviated. In the sagittal plane, a normal thoracic kyphosis can change to hyperkyphosis, hypokyphosis or lordosis. In the axial plane, vertebral bodies are rotated and chief of all, the apical vertebral is most rotated. Deformities in any one plane does not develop in isolation and seems to be coupled to the curvature, rotation, and translation in the other planes78).
Historically, Harrington instrumentation to distract along the concavity of the curve for correction of the deformity was introduced. However, this technique resulted in iatrogenic flat-back or disappearance of the thoracic kyphosis, and only the coronal curve was regarded in this technique9). A variety of segmental corrections for AIS has been introduced, such as hook instrumentation, wiring and hooks, and pedicle screws instrumentation for segmental rotation. Now, the pedicle screw instrumentation technique is generally accepted as the chosen method for curve correction31416). SRR is known to impose a three dimensional deformity correction in AIS1310111216). SRR is generally accepted these days for the curve correction method of AIS. However, the effect for rotation correction is controversial. Some reports shows that SRR can correct coronally and sagittally but cannot suffice rotationally910). Other reports suggested about 20% to 40% maximum rotational correction412).
DVD is based on pedicle screw instrumentation. It enables vertebral body rotation with screw rotation which is inserted into the vertebral body. Lee et al.9) reported that rotation correction was about 42.5% and coronal curve correction was about 80% after DVD. Thoracic kyphosis had also improved after surgery. Some researchers reported DVD showed better rotational and coronal correction than SRR. However, they also reported there are no differences in correction of clinical thoracic hump or patients' assessment between the two groups917). More correction of axial rotation does not mean better correction of one's body image. Even though DVD can lead to more correction of the rotational angle than SRR, body image including the thoracic hump or a patient's satisfaction after surgery does not differ significantly. Pushing down of the thoracic hump to correct sufficiently for the rotation angle or for thoracoplasty during DVD might be demanding of the to surgeon and patients. SRR is technically relatively easy compared to DVD and might serve as an option to correct for AIS.
In our study, we introduce screws into the vertebral body through pedicles and rotate the rod fixed in the screws. All patients have shown good curve correction in the coronal and sagittal planes after surgery. Axial rotation correction was also corrected well at about 50%. Previously reported rod derotation studies were conducted by the hooks or wire technique. Hooks or wires can not deliver the torque to the vertebral body efficiently so the rate of rotation correction might be relatively low and inconsistent.
Vertebral rotation in the axial plane might contribute to the thoracic hump, which is a major concern because this creates a distorted body image. The thoracic hump is frequently considered the second highest cause for surgical deformity correction, and is considered an important outcome factor after surgery13). However, the correlation between radiographic rotation correction and thoracic hump correction yields a lack of consensus. Some researchers suggest a strong correlation between the apical vertebral rotation preoperatively in the CT and the clinical thoracic hump2). Others insist there is no correlation between apical vertebral rotation and trunk rotation on a CT. Also, the most rotated vertebra is not necessarily related to the peak of rib deformity5). In our study, the mean major Cobb's angle before surgery was 53.7°, which included a relatively moderate deformity thus not requiring a thoracoplasty to correct for the hump. All patients answered questionnaires of SRS-22 and the scores were significantly different before and after surgery, especially in questionnaires about self-image.
This study has some limitations. One of the limitations is small number of patients who operated on via the SRR method. In the future, further data should be collected by additional surgeries for AIS. Second, the follow up period was relatively short and all of the patients did not undergo CTs. However, this report is characterized as a preliminary study that focuses on the surgical technique of a domestic Korean neurosurgeon. In the future, more attempts about scoliosis surgery will guarantee expanding the horizon in Korean neurosurgeons.
Deformity surgery is challenging to neurosurgeons and it might demand intense labor of surgeon. We suggest that simple rod rotation with pedicle screw instrumentation could correct successfully for axial rotation without complication. This is more convenient than direct vertebral rotation. Simple rod rotation might serve as a good option to correct the deformed curve of AIS.
References
1. Bridwell KH. Surgical treatment of adolescent idiopathic scoliosis : the basics and the controversies. Spine (Phila Pa 1976). 1994; 19:1095–1100. PMID: 8029750.
2. Carlson BB, Burton DC, Asher MA. Comparison of trunk and spine deformity in adolescent idiopathic scoliosis. Scoliosis. 2013; 8:2. PMID: 23351196.

3. Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988; 227:10–23. PMID: 3338200.

4. Ecker ML, Betz RR, Trent PS, Mahboubi S, Mesgarzadeh M, Bonakdapour A, et al. Computer tomography evaluation of Cotrel-Dubousset instrumentation in idiopathic scoliosis. Spine (Phila Pa 1976). 1988; 13:1141–1144. PMID: 3206272.

5. Erkula G, Sponseller PD, Kiter AE. Rib deformity in scoliosis. Eur Spine J. 2003; 12:281–287. PMID: 12800002.

6. Ho EK, Upadhyay SS, Chan FL, Hsu LC, Leong JC. New methods of measuring vertebral rotation from computed tomographic scans. An intraobserver and interobserver study on girls with scoliosis. Spine (Phila Pa 1976). 1993; 18:1173–1177. PMID: 8362322.

7. Kuklo TR, Potter BK, Lenke LG. Vertebral rotation and thoracic torsion in adolescent idiopathic scoliosis : what is the best radiographic correlate? J Spinal Disord Tech. 2005; 18:139–147. PMID: 15800431.

8. Lea Plaza CA, Karsaclian M, Rocca C. Segmental scoliosis correlation : use of the Lea Plaza Frame. Spine (Phila Pa 1976). 2004; 29:398–404. PMID: 15094536.
9. Lee SM, Suk SI, Chung ER. Direct vertebral rotation : a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004; 29:343–349. PMID: 14752361.

10. Lenke LG, Bridwell KH, Baldus C, Blanke K, Schoenecker PL. Cotrel-Dubousset instrumentation for adolescent idiopathic scoliosis. J Bone Joint Surg Am. 1992; 74:1056–1067. PMID: 1522092.

11. Muschik M, Schlenzka D, Robinson PN, Kupferschmidt C. Dorsal instrumentation for idiopathic adolescent thoracic scoliosis : rod rotation versus translation. Eur Spine J. 1999; 8:93–99. PMID: 10333147.

12. Pollock FE, Pollock FE Jr. Idiopathic scoliosis : correction of lateral and rotational deformities using the Cotrel-Dubousset spinal instrumentation system. South Med J. 1990; 83:161–165. PMID: 2305296.
13. Pratt RK, Burwell RG, Cole AA, Webb JK. Patient and parental perception of adolescent idiopathic scoliosis before and after surgery in comparison with surface and radiographic measurements. Spine (Phila Pa 1976). 2002; 27:1543–1550. discussion 1551-1552PMID: 12131715.

14. Schlenzka D, Poussa M, Muschik M. Operative treatment of adolescent idiopathic thoracic scoliosis. Harrington-DTT versus Cotrel-Dubousset instrumentation. Clin Orthop Relat Res. 1993; (297):155–160. PMID: 8242924.
15. Suk SI, Kim JH, Kim SS, Lim DJ. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur Spine J. 2012; 21:13–22. PMID: 21874625.

16. Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995; 20:1399–1405. PMID: 7676339.

17. Tang X, Zhao J, Zhang Y. Radiographic, clinical, and patient's assessment of segmental direct vertebral body derotation versus simple rod derotation in main thoracic adolescent idiopathic scoliosis : a prospective, comparative cohort study. Eur Spine J. 2015; 24:298–305. PMID: 25384992.

Fig. 1
Plain radiographs and CT images of a 16-year-old girl demonstrate the scoliotic curvature of the spine. A and C : Lenke classification is 1C. Coronal Cobb's angle between T4 of the proximal end of the vertebra and T12 of distal end of the vertebra were at 53 degrees. B and D : Scoliotic curvature had been corrected after surgery. E and F : Preoperative axial CT image demonstrated about a 20 degrees rotation angle, preoperatively. The rotation angle was corrected at about 10 degrees after surgery. The correction rate was about 50%.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download