Abstract
Objective
To report the learning curve of percutaneous endoscopic lumbar discectomy (PELD) for a surgeon who had not been previously exposed to this procedure based on the period and detailed technique with a retrospective matched comparative design.
Methods
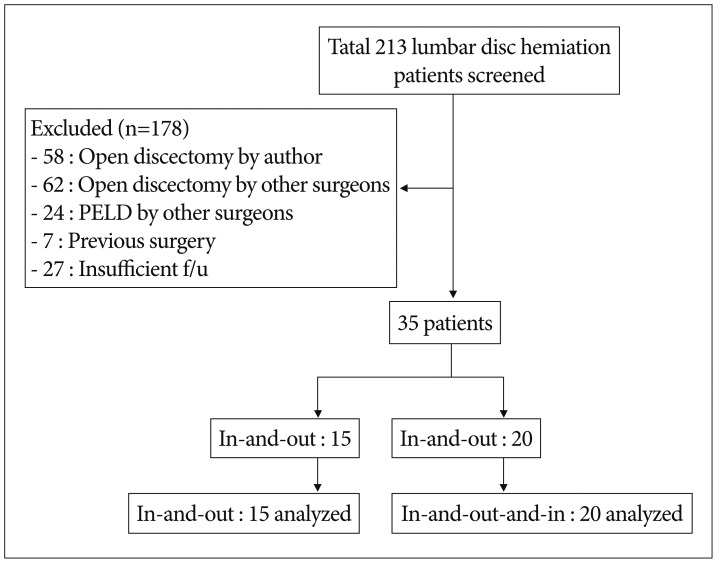
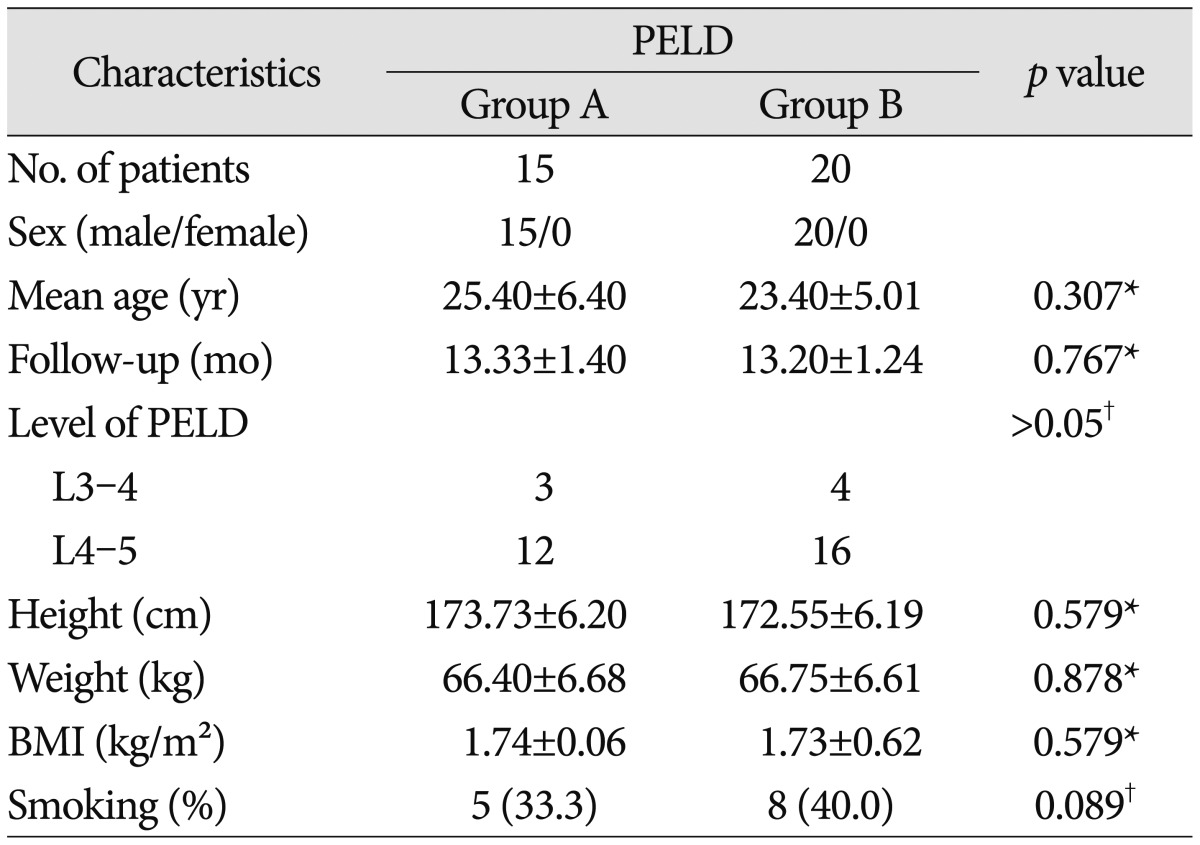
Of 213 patients with lumbar disc herniation encountered during the reference period, 35 patients who were followed up for 1 year after PELD were enrolled in this study. The patients were categorized by the period and technique of operation : group A, the first 15 cases, who underwent by the 'in-and-out' technique; group B, the next 20 cases, who underwent by the 'in-and-out-and-in' technique. The operation time, failure rate, blood loss, complication rate, re-herniation rate, the Visual Analogue Scale (VAS) for back and leg were checked. The alteration of dural sac cross-sectional area (DSCSA) between the preoperative and the postoperative MRI was checked.
Results
Operative time was rapidly reduced in the early phase, and then tapered to a steady state for the 35 cases receiving the PELD. After surgery, VAS scores for the back and leg were decreased significantly in both groups. Complications occurred in 2 patients in group A and 2 patients in group B. Between the two groups, there were significant differences in operative time, improvement of leg VAS, and expansion of DSCSA.
A microdiscectomy has been considered to be the gold standard procedure for symptomatic lumbar disc diseases148101415182023252627). However, open surgery requires laminectomies, muscle damages, removal of yellow ligament and nerve retraction. This can cause instability and scarring of the epidural space, which becomes clinically symptomatic in 10% or more of patients114).
Recently, percutaneous endoscopic lumbar discectomy (PELD) has been performed as an alternative to classic open discectomy with results that are comparable to those of open discectomy. Similar to other surgical technique, minimally invasive spinal techniques have become increasingly popular with both spine surgeons and patients undergoing surgery for symptomatic lumbar disc diseases. PELD has several advantages over open discectomy. PELD is usually performed under local anesthesia202127). Postoperative pain is minimal, normal paraspinal muscles are preserved, and the risk of postoperative epidural scar formation and instability can be minimized202127).
Although many studies have shown the efficacy of PELD with good clinical outcome, the percutaneous approach poses challenges to surgeons and the PELD learning curve is usually perceived to be steep. After the introduction of the PELD, many investigators have stated concerns about the technique as well as the clinical outcome of the endoscopic discectomy13456710111220212627). Major complications such as nerve root injury, dural tear, hematoma, visceral injury, and surgical site infection may occur, possibly resulting from lack of skilled surgical techniques during the learning period123456891517222527). However, few published studies have specifically addressed this aspect of the procedure. In addition, prior studies do not provide clear information on the learning curve of this procedure based on the detailed technique.
The purpose of this study was to report the learning curve of PELD for a single surgeon who had not been previously exposed to this procedure. We conducted a retrospective comparative study with a 1-year follow-up period after surgery to assess the learning curve of PELD based on the period and technique of operation.
After obtaining informed consent from each patient, this study was carried out. Patient enrollment began in August 2012 and continued until January 2014. All consecutive patients with lumbar disc herniation were considered for this study, and all patients who were interested and eligible were enrolled. All enrolled patients met the study inclusion and exclusion criteria. Inclusion criteria were as follows : 1) a single level intracanalicular soft lumbar disc herniation diagnosed with lumbar spine radiographs, computed tomography (CT), and magnetic resonance image (MRI) that corresponded to clinical symptoms; 2) conservative treatment failure after at least 8 weeks that included medication, physical therapy, and injection; and 3) follow-up of at least 1 year. Those who met any of the following criteria were excluded : 1) lateral recess stenosis, hard disc herniation, foraminal and extraforaminal disc herniations, sequestrated fragment and spinal instability; 2) follow-up less than 1 year; and 3) inability to accurately record results of pre and postoperative questionnaires due to medical or other problems. All of these patients were Korean military serviceman as ordinary soldiers or non-commissioned officers at the time of their operations. Before surgery, all patients were informed of the details of the PELD surgery, including the local anesthesia, potential complications, and benefits of the procedures. All surgical procedures were performed by 1 spine surgeon who had experienced about 70 cases of open microdiscectomy, but had no previous experience with PELD. Before starting this study, the surgeon observed 20 PELD performed by experienced surgeons and performed about 50 epidural block procedures via the same transforaminal route. He attended cadaveric endoscopic surgery workshop twice.
The Visual Analogue Scale (VAS) for back and leg were measured preoperatively, at 3, 6, and 12 months after the PELD. The alteration of VAS, the operating time, failure rate, blood loss, complication rate, and re-herniation rate were checked for assessment of the learning curve. All patients underwent MRI preoperatively and 6 months after PELD. The alteration of dural sac cross-sectional area (DSCSA) between the preoperative and the postoperative MRI was checked to demonstrate the extent of decompression and the learning curve during the different operative period. To evaluate the change of DSCSA, two radiologists separately measured the preoperative and postoperative DSCSA using a picture archiving communication system (PACS) feature (Marosis 5.0 PACS viewer, Marotech, Seoul, Korea). The space was drawn by an imaginary area at the narrowest lesion on the T2-weighted axial MRI (Fig. 1). Although this study was retrospective comparative design, we collected all data prospectively. The follow-up data was collected by medical record review and direct interviews at out-patient center. The patients were not allowed to review their previous study.
We used the conventional 'in-and-out' technique. All operations were performed under conventional way. The procedures were as follows : 1) The entry point was between the tip of the spinous process and the spino-laminar junction on the lateral view of the C-arm image; 2) an 18-gauge spinal needle was aimed at the lateral border of the superior articular facet targeting area. Once the bony contact was established, the needle was withdrawn and redirected towards the posterolateral annulus by hooking the ventral border of the facet (Fig. 2); 3) when introducing the obturator by twisting maneuver, the obturator should be directed towards posterolateral annulus by pushing the other end of the obturator down (Fig. 3). The ventrolateral border of the facet worked as a guiding lever; 4) according to the 'in-and-out' technique, the working sheath was moved to the epidural space, fragmentectomy was done; 5) after all these procedures, the circumference of the annular defect was coagulated by Ellman and a side firing holmium yttrium-aluminum-garnet (Ho : YAG) laser; and 6) most patients received intraoperative epidural steroid injection at the end of their surgery.
After performing the operation for 15 patients, the corresponding author altered technique to 'in-and-out-and-in', because he could remove posterior longitudinal ligament (PLL) and recheck the targeted lesion with adding the 'in' process from this time. Although the procedure was the same technique with the conventional 'in-and-out' technique, it had some differences : 1) after removal of central disc fragment, the working sheath was moved back to the epidural space, and the PLL was removed in half-and-half view (Fig. 4); 2) after removal of PLL, while confirming the pulsation of dura with direct vision, the posterolateral target fragment was rechecked by introducing the working sheath from lateral to medial area (Fig. 5).
All patients were typically discharged the 5 to 7 days after surgery. If the patient's symptoms had not improved, no heavy work was permitted for 8 weeks to prevent recurrence.
Statistical analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). The mean values±standard deviation or the median with the interquartile range were shown. Student t-tests were conducted to confirm intergroup differences in cases with normal distributions. The Mann-Whitney U tests were used to compare variables between two groups with non-normal distributions. For categorical variables, chi-square tests and the Fischer's exact tests were performed between independent two groups. Paired t-test was used to compare pre- and post-operative values. All p values less than 0.05 were considered statistically significant.
Of 213 patients with lumbar disc herniation encountered during the reference period, 35 patients were finally enrolled in this study. The patients were categorized by the period of operation : group A, the first 15 cases, who underwent by the 'in-and-out' technique; group B, the next 20 cases, who underwent by the 'in-and-out-and-in' technique (Fig. 6). Patient demographics including follow-up period, were not significantly different between the two groups (Table 1).
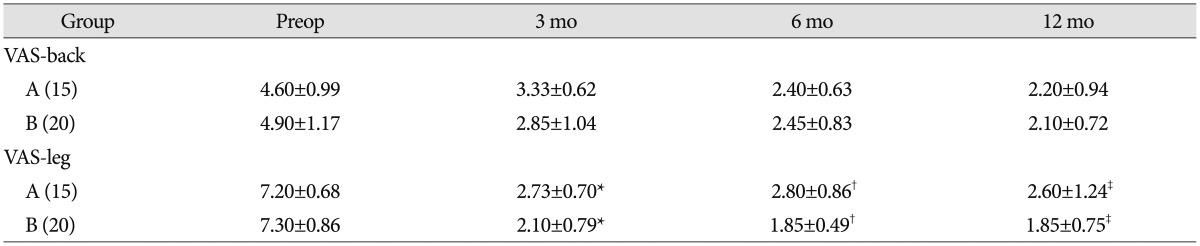
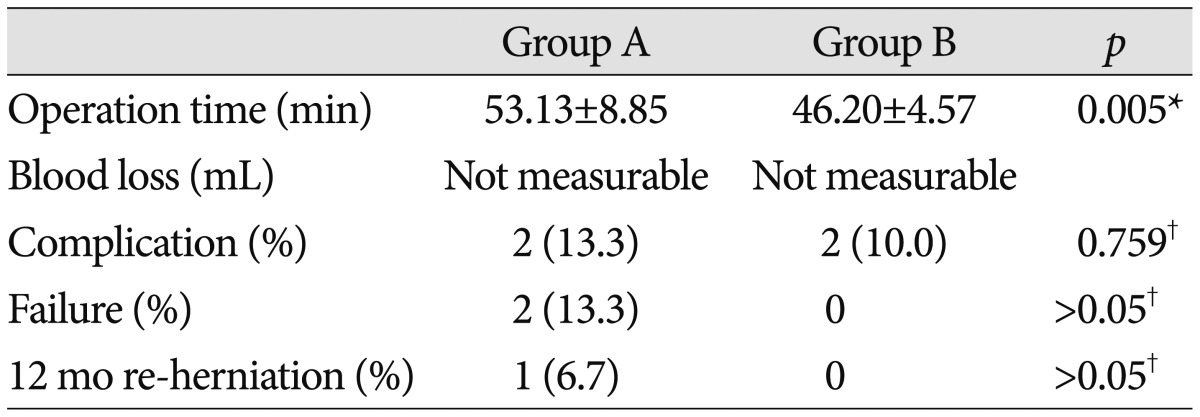
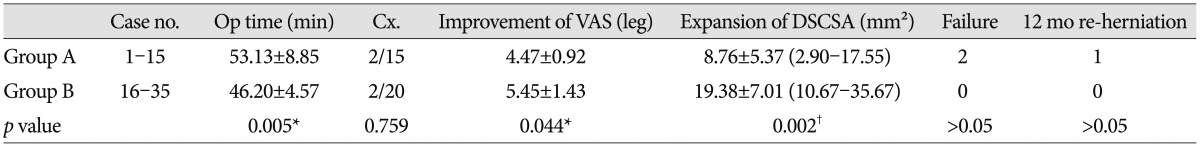
We measured the VAS scores of the back and leg before surgery, 3, 6, and 12 months after surgery. Preoperatively, the back and leg VAS scores were 4.60±0.99 and 7.20±0.68, respectively, in group A and, 4.90±1.17 and 7.30±0.86, respectively, in group B. These results revealed no significant differences. After surgery, VAS scores for the back and leg were decreased significantly in both groups. At 12 months after surgery, the back and leg VAS scores were 2.20±0.94 and 2.60±1.24, respectively, in group A and, 2.10±0.72 and 1.85±0.75, respectively, in group B. There were significant differences between the groups for the leg VAS scores at 3, 6, and 12 months after surgery (p=0.019, 0.001, 0.033, respectively). However, there was no significant difference between the groups for back VAS scores after surgery (Table 2, Fig. 7). The mean operation time was 53.13±8.85 minutes (range 42–75) for group A, and 46.20±4.57 minutes (range 38–55) for group B, showing a significant difference (p=0.005). Operative blood loss was not measurable. Incomplete removal of target fragment was done in 2 patients in group A, and, we regarded these cases as failure of the PELD. However, there was no significant difference between the two groups. The 12 months re-herniation occurred 1 patient in group A, however, there was no significant difference between the groups (Table 3).
Complications occurred in 2 patients in group A and 2 patients in group B. One patient complained of dysesthesia on the posterolateral thigh, which improved spontaneously two to three days after surgery. One patient who took the longest operation time (75 min), complained headache during surgery, especially at the end of the surgery, which improved spontaneously after absolute bed rest for one day. One patient showed pain shock during the procedure, especially just after performing discography. One patient presented with symptomatic pseudocyst 2 months after PELD, which improved slowly after epidural block. There were no significant complications, such as neurovascular injury, retroperitoneal hematoma, and surgical site infections, and there was no significant difference in the complication rate between the two groups.
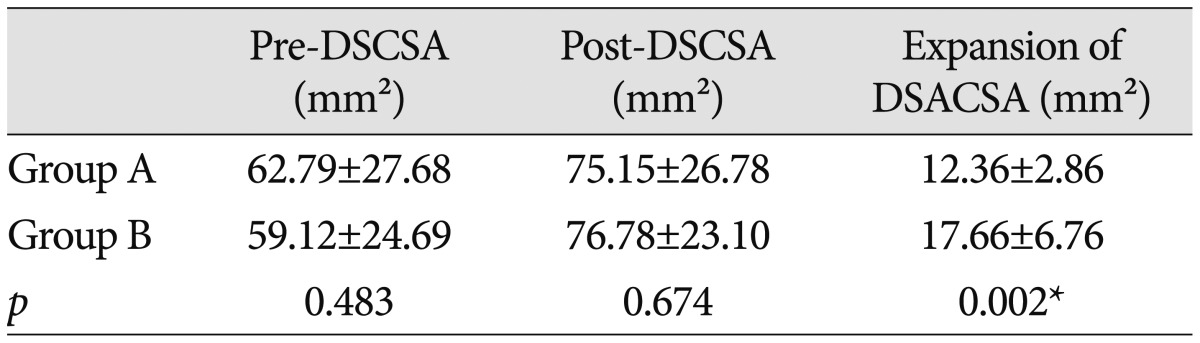
Preoperative DSCSA was 62.79±27.68 mm2 in group A, and 59.12±24.69 mm2 in group B. Postoperative DSCSA was 75.15±26.78 mm2 in group A, and 76.78±23.10 mm2 in group B. The expansion of DSCSA between the preoperative and the postoperative MRI was 12.36±2.86 mm2 in group A, and 17.66±6.76 mm2 in group B. There was significant difference between the groups (p=0.002) (Table 4, Fig. 8).
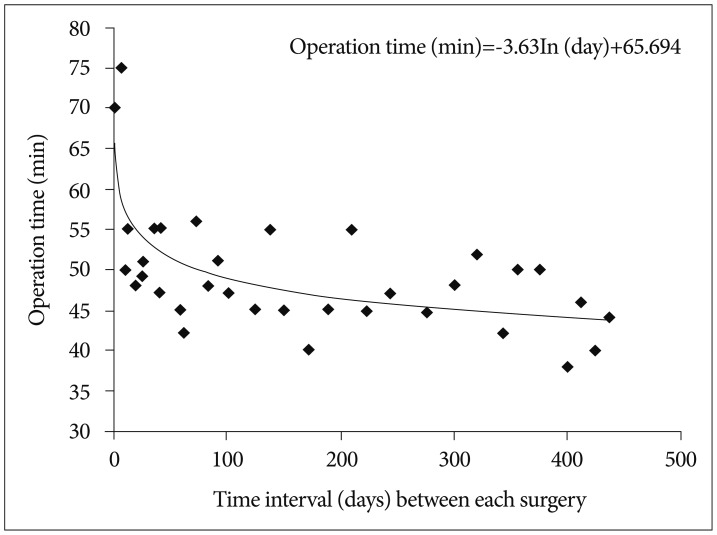
We assessed the learning curve for the PELD from the results. Operation time was rapidly reduced in the early phase, and then tapered to a steady state for the 35 cases receiving the PELD (Fig. 9). Between the two groups, there were significant differences in operation time, improvement of leg VAS, and expansion of DSCSA (p=0.005, 0.044, 0.002, respectively). A summary of the results was described to evaluate the learning curve of PELD (Table 5).
The PELD has not been generally adopted because the learning curve of the procedure seemed to be longer and steeper than that of conventional microsurgery18917). Hirano et al.8) described many difficulties before introducing this procedure : 1) the direction of approach is completely opposite; usual microsurgery is from the outside in, whereas PELD is from the inside out; 2) anatomical landmarks are absent; and 3) tissue differentiations between annulus fibrosus and PLL, or PLL and dura matter are vague. Kafadar et al.12) reported a high failure rate of 14/42, of whom 7 patients eventually underwent re-operation (open discectomy), and 6 of these 7 patients in the first 8 months. However, Lee and Lee17) reported that the PELD learning curve was acceptable, with relatively low failure, complication rate of 7.8% and 3.9%, respectively, and no major complications. Many authors recommended attending seminars, hands-on training, and learning procedures at advanced surgical centers when introducing this PELD891721). Before starting this study, the author had no previous experience with PELD. He performed about 20 epidural block procedures via the same transforaminal route and attended cadaveric endoscopic surgery workshop twice to develop high needle technique and surgical technique. Although minor complication rate of 11.4% was relatively higher than previous other study (we included mild dysesthesia as a complication), the present study indicated that the PELD learning curve is acceptable, with relatively low failure rate of 2.9%, respectively, and no significant major complications. We recommend practicing an epidural block via the same trajectory with the PELD route before introducing PELD, which enables beginners to develop the stable learning curve.
Most studies recommended that the needle should arrive at the medial or mid-pedicular line on the anteroposterior fluoroscopic image and posterior vertebral line on the lateral fluoroscopic image46789121720212326). However, it is not easy to predict the final destination of the needle since it is affected by multiple factors such as the entry point, and the width of the pedicle7). Han et al.7) reported the 'obturator guiding technique' to enhance the safety and reduce drawbacks associated with this needling process. Sairyo et al.21) described the 'walking technique', which the needle walks from pedicle to the disc to avoid injuring the nerve root. In the present study, we determined entry point between the tip of the spinous process and the spino-laminar junction on the lateral view. Once lateral border of facet was established, the needle was withdrawn and redirected towards the posterolateral annulus by hooking the ventral border of the facet. With this procedure, there were no major neural complications or abdominal organ damages. Since this procedure is really challengeable as a beginner, we recommend practicing epidural block via the same route and the technique that hooking the ventral border of the facet with the needle when introducing the needle.
The initial concept of PELD was central disc decompression, however, the surgical techniques have evolved into targeted fragmentectomy891721). Highly experienced surgeons have expanded the indications for PELD and have reported successful results even in cases with highly migrated disc herniation, foraminal/extraforaminal disc herniation, and disc herniation with spinal stenosis1410141826). However, this procedure is really challengeable for inexperienced surgeons, and, improper selection of patients often results in a poor surgical outcome and a failure of targeted fragmentectomy. In the present study, as a beginner, the author selected only a single level intracanalicular soft lumbar disc herniation. Patients with lateral recess stenosis, bony spurs, foraminal, extraforaminal disc and instability were not included. Despite most of studies showed no significant correlation of DSCSA obtained by conventional MRI with clinical symptoms of spinal stenosis1924), we experienced the better clinical outcomes (the improvement of leg VAS) and decompression rates (the expansion of DSCSA) in the group with 'in-and-out-and-in' technique. We could recheck not only the central disc fragment but also the targeted fragment using the 'in-and-out-and-in' technique. Unfortunately, there were no clinical data and evidences related this issue, further evaluation will be needed for reliable conclusions.
Lee and Lee17) reported a significant reduction in the operative time after the 17th patient was treated by PELD. In this study, as depicted in Fig. 9, the reduction of the operative time occurred around the 10th to 12th case, resulting in a steep learning curve, which represents the rapid acquisition of skills for a beginner. The factors for the longer operative time at early phase were as follows : 1) intraoperative bleeding which blurred the operative field; 2) loss of depth and directional sensation due to the 2-dimensional vision of the endoscope.
Since the approach is completely different from the conventional interlaminar technique, it is not difficult to assume that there would be special surgery-related complications in this technique. In the present study, we experienced one case of exiting nerve root injury among 35 cases, which occurred in the early phase. Choi et al.5) reported 20 cases having an exiting nerve injury among 233 cases. They analyzed the working sheath might compress the exiting root during the surgery, thus, prolonged operation time is one of the factors for the irritation. Clinical demonstration in the present one case was supported their hypothesis. Another important complication is intracranial hypertension, which may result in headache, neck pain, seizure, or even death. Choi et al.3) reported 4 cases of seizure among 16,725 cases of PELD and Sairyo et al.22) reported 2 cases of neck pain among 100 cases. Elevation of the intracranial pressure may occur if the irrigation pressure is too high or if the endoscopic maneuvers take too long322). Joh et al.11) concluded that the neck pain is induced by the high epidural pressure with continuous infusion. Among the present cases, one patient complained headache during surgery, who experienced the longest operative time (75 min) in our early phase. Clinical demonstration in this one case was supported their hypothesis. Pain shock can happen during PELD, especially during annulotomy or cannular insertion. Lee and Lee17) reported pain shock and prevented that by additional injecting of lidocaine on the surface of the annulus just before annulotomy. We experienced one such case during doing discography, which the pain relieved spontaneously after waiting. We experienced a symptomatic post-discectomy pseudocyst after PELD. Kang and Park13) reported that symptomatic post-discectomy pseudocyst was detected at two months' postoperative period in about 1% of cases. The present case was detected at two months' postoperative period, and improved slowly after performing epidural injection.
In the present study, 12-month disc re-herniation was observed in one case (2.9%), a rate comparable to that reported for the PELD (2.2%) in a previous study16), in which experienced senior surgeons performed all procedures. We experienced that case in the early phase using the 'in-and-out' technique. Lee and Lee17) hypothesized that the relatively high re-herniation rate of their study might be attributable to limited target fragmentectomy. We could remove not only the target fragment but also central fragment effectively using the 'in-and-out-and-in' technique at our late phase. We could recheck the target fragment through this technique while re-introducing working channel from lateral to medial area after removal of PLL. Although statistically not significant, this result suggests that increasing experience and technique with PELD might influence the 12-month disc re-herniation.
It is important to note that present study has several limitations. First, it was a retrospective comparative study with a small sample size (35 patients), short follow up period (1 year), limited operative level (L3–4 and L4–5), limited indication (soft, intracanalicular discherniation), and limited method of radiological measuring about the DSCSA. Second, the study participants were relatively young (mean age 23–26) and limited to males who were recruited from an armed forces hospital. Because this study was conducted on a limited population, this could make statistical analysis difficult because of non-normal distribution, and these conclusions might not be valid for general populations. However, because this study included a homogeneous population of young male patients from armed forces hospital, we could reduce selection bias and performance bias. Prospective randomized studies with longer follow-up time and larger sample sizes are necessary to provide more useful information.
The PELD for symptomatic lumbar disc herniation is a safe and effective minimally invasive operative technique. Although a learning curve is needed in order to become familiar with PELD, the PELD learning curve seems to be acceptable with sufficient preparation and pre-operative training such as demonstration teaching by experienced surgeon. Despite of acceptable learning curve, because of their high tendency to delayed operation time, operation failure, and re-herniation, caution should be exercised at the early phase of the procedure.
References
1. Chae KH, Ju CI, Lee SM, Kim BW, Kim SY, Kim HS. Strategies for noncontained lumbar disc herniation by an endoscopic approach : transforaminal suprapedicular approach, semi-rigid flexible curved probe, and 3-dimensional reconstruction CT with discogram. J Korean Neurosurg Soc. 2009; 46:312–316. PMID: 19893718.

2. Cho JY, Lee SH, Lee HY. Prevention of development of postoperative dysesthesia in transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar disc herniation : floating retraction technique. Minim Invasive Neurosurg. 2011; 54:214–218. PMID: 22287030.

3. Choi G, Kang HY, Modi HN, Prada N, Nicolau RJ, Joh JY, et al. Risk of developing seizure after percutaneous endoscopic lumbar discectomy. J Spinal Disord Tech. 2011; 24:83–92. PMID: 20625320.

4. Choi G, Modi HN, Prada N, Ahn TJ, Myung SH, Gang MS, et al. Clinical results of XMR-assisted percutaneous transforaminal endoscopic lumbar discectomy. J Orthop Surg Res. 2013; 8:14. PMID: 23705685.

5. Choi I, Ahn JO, So WS, Lee SJ, Choi IJ, Kim H. Exiting root injury in transforaminal endoscopic discectomy : preoperative image considerations for safety. Eur Spine J. 2013; 22:2481–2487. PMID: 23754603.

6. Choi KC, Kim JS, Ryu KS, Kang BU, Ahn Y, Lee SH. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation : transforaminal versus interlaminar approach. Pain Physician. 2013; 16:547–556. PMID: 24284840.
7. Han IH, Choi BK, Cho WH, Nam KH. The obturator guiding technique in percutaneous endoscopic lumbar discectomy. J Korean Neurosurg Soc. 2012; 51:182–186. PMID: 22639720.

8. Hirano Y, Mizuno J, Takeda M, Itoh Y, Matsuoka H, Watanabe K. Percutaneous endoscopic lumbar discectomy - early clinical experience. Neurol Med Chir (Tokyo). 2012; 52:625–630. PMID: 23006872.

9. Hsu HT, Chang SJ, Yang SS, Chai CL. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J. 2013; 22:727–733. PMID: 23076645.

10. Jasper GP, Francisco GM, Telfeian AE. Endoscopic transforaminal discectomy for an extruded lumbar disc herniation. Pain Physician. 2013; 16:E31–E35. PMID: 23340542.
11. Joh JY, Choi G, Kong BJ, Park HS, Lee SH, Chang SH. Comparative study of neck pain in relation to increase of cervical epidural pressure during percutaneous endoscopic lumbar discectomy. Spine (Phila Pa 1976). 2009; 34:2033–2038. PMID: 19675511.

12. Kafadar A, Kahraman S, Akbörü M. Percutaneous endoscopic transforaminal lumbar discectomy : a critical appraisal. Minim Invasive Neurosurg. 2006; 49:74–79. PMID: 16708335.

13. Kang SH, Park SW. Symptomatic post-discectomy pseudocyst after endoscopic lumbar discectomy. J Korean Neurosurg Soc. 2011; 49:31–36. PMID: 21494360.

14. Kim HS, Ju CI, Kim SW, Kim JG. Endoscopic transforaminal suprapedicular approach in high grade inferior migrated lumbar disc herniation. J Korean Neurosurg Soc. 2009; 45:67–73. PMID: 19274114.

15. Kim HS, Park JY. Comparative assessment of different percutaneous endoscopic interlaminar lumbar discectomy (PEID) techniques. Pain Physician. 2013; 16:359–367. PMID: 23877452.
16. Lee DY, Ahn Y, Lee SH. Percutaneous endoscopic lumbar discectomy for adolescent lumbar disc herniation : surgical outcomes in 46 consecutive patients. Mt Sinai J Med. 2006; 73:864–870. PMID: 17117312.
17. Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir (Tokyo). 2008; 48:383–388. discussion 388-389PMID: 18812679.

18. Lee S, Kim SK, Lee SH, Kim WJ, Choi WC, Choi G, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation : classification of disc migration and surgical approaches. Eur Spine J. 2007; 16:431–437. PMID: 16972067.

19. Lohman CM, Tallroth K, Kettunen JA, Lindgren KA. Comparison of radiologic signs and clinical symptoms of spinal stenosis. Spine (Phila Pa 1976). 2006; 31:1834–1840. PMID: 16845360.

20. Ruetten S, Komp M, Merk H, Godolias G. Use of newly developed instruments and endoscopes : full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine. 2007; 6:521–530. PMID: 17561740.

21. Sairyo K, Egawa H, Matsuura T, Takahashi M, Higashino K, Sakai T, et al. State of the art : transforaminal approach for percutaneous endoscopic lumbar discectomy under local anesthesia. J Med Invest. 2014; 61:217–225. PMID: 25264038.

22. Sairyo K, Matsuura T, Higashino K, Sakai T, Takata Y, Goda Y, et al. Surgery related complications in percutaneous endoscopic lumbar discectomy under local anesthesia. J Med Invest. 2014; 61:264–269. PMID: 25264043.

23. Sencer A, Yorukoglu AG, Akcakaya MO, Aras Y, Aydoseli A, Boyali O, et al. Fully endoscopic interlaminar and transforaminal lumbar discectomy : short-term clinical results of 163 surgically treated patients. World Neurosurg. 2014; 82:884–890. PMID: 24907438.

24. Sirvanci M, Bhatia M, Ganiyusufoglu KA, Duran C, Tezer M, Ozturk C, et al. Degenerative lumbar spinal stenosis : correlation with Oswestry Disability Index and MR imaging. Eur Spine J. 2008; 17:679–685. PMID: 18324426.

25. Wang H, Huang B, Zheng W, Li C, Zhang Z, Wang J, et al. Comparison of early and late percutaneous endoscopic lumbar discectomy for lumbar disc herniation. Acta Neurochir (Wien). 2013; 155:1931–1936. PMID: 23975645.

26. Xin G, Shi-Sheng H, Hai-Long Z. Morphometric analysis of the YESS and TESSYS techniques of percutaneous transforaminal endoscopic lumbar discectomy. Clin Anat. 2013; 26:728–734. PMID: 23824995.

27. Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation : surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976). 2002; 27:722–731. PMID: 11923665.
Fig. 1
Preoperative and postoperative dural sac cross-sectional area (DSCSA) (mm2) at the index level. The space was drawn by an imaginary area at the narrowest lesion on the T2-weighted axial MRI.
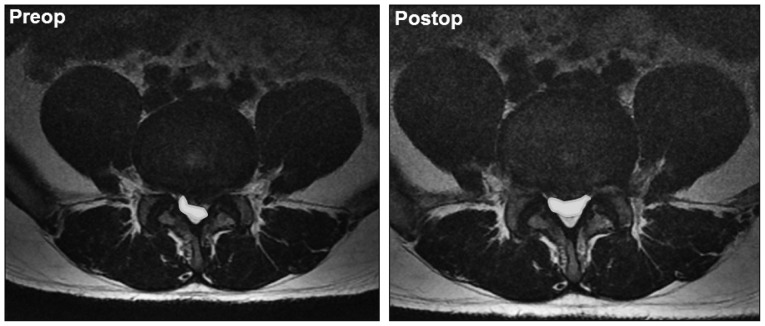
Fig. 2
The entry point is indicated between the tip of the spinous process and the spino-laminar junction. Once the facet contact was established (1), the needle was withdrawn and redirected (dotted arrows) towards the posterolateral annulus by hooking the ventral border of the facet (2). F : Facet joint.
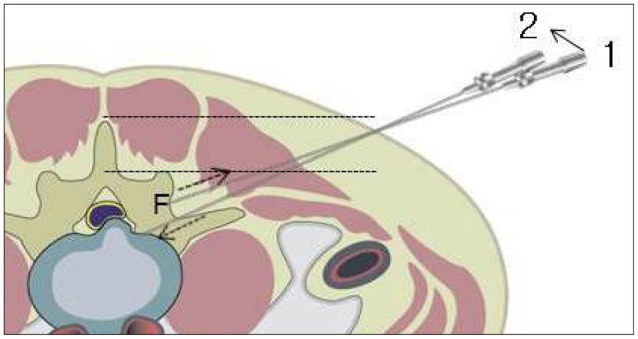
Fig. 3
The obturator should be directed towards posterolateral annulus by pushing the other end of the obturator down.
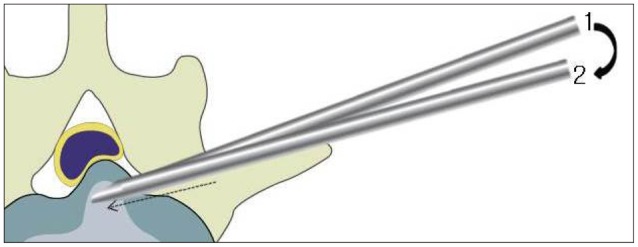
Fig. 4
After removal of central disc fragment, the working sheath was moved back to the epidural space (A), and the posterior longitudinal ligament (PLL) was removed in half-and-half view (B). D : herniated disc stained by indigocarmine, F : epidural fat, P : posterior longitudinal ligament.
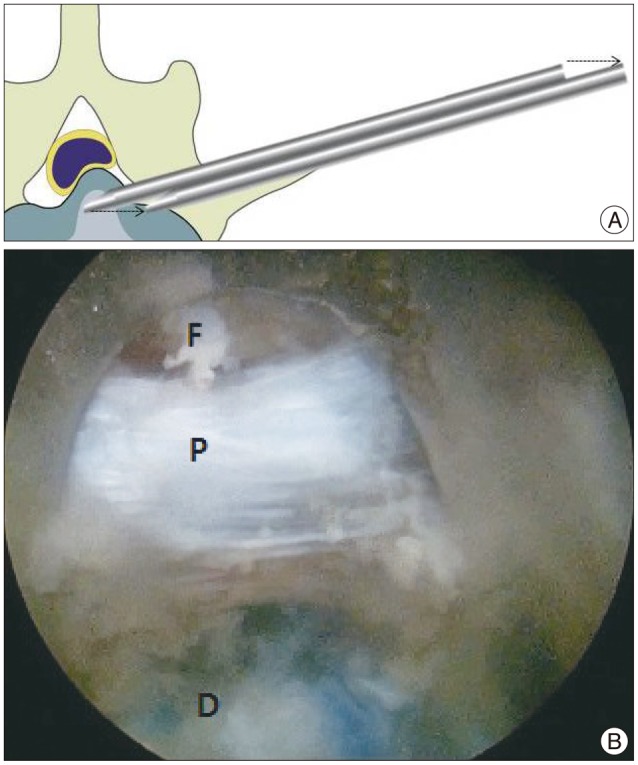
Fig. 5
After removal of PLL, the posterolateral target fragment (gray area) was removed by introducing the working sheath from lateral to medial area.
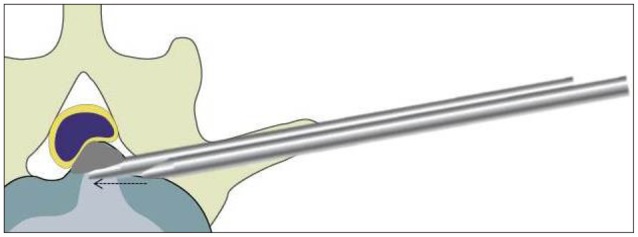
Fig. 7
Clinical outcomes using VAS scores. There were significant differences between the groups for the leg VAS at 3, 6, 12 months after surgery (p=*0.019, †0.001, ‡0.033, respectively). VAS : visual analogue scale.
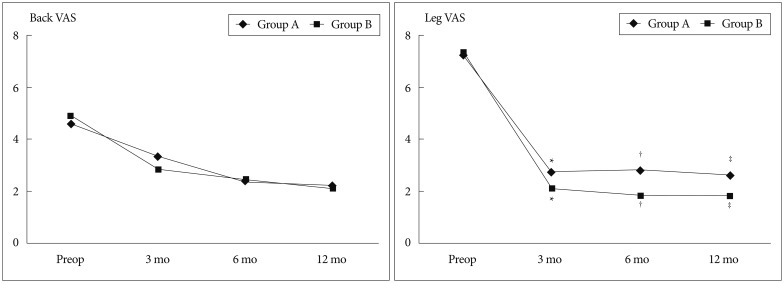
Fig. 8
Expansion of DSCSA. There was significant difference between the groups (*p=0.002). DSCSA : dural sac cross-sectional area.
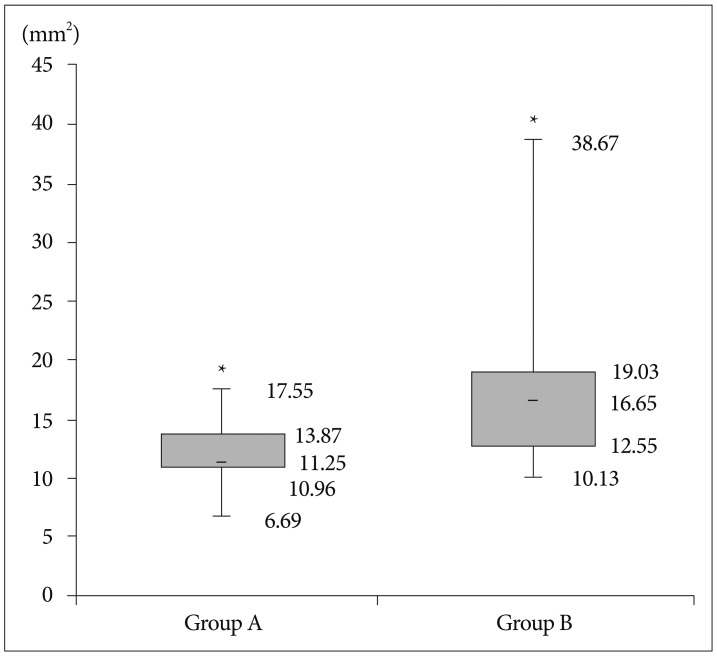
Fig. 9
Operation time was rapidly reduced in the early phase, and then tapered to a steady state for the 35 cases receiving the PELD. PELD : percutaneous endoscopic lumbar discetomy.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download