Abstract
Objective
Recently, the survival of patients with hepatocellular carcinoma (HCC) has been prolonged with improvements in various diagnostic tools and medical treatment modalities. Consequently, spine metastases from HCC are being diagnosed more frequently. The accurate prediction of prognosis plays a critical role in determining a patient's treatment plan, including surgery for patients with spinal metastases of HCC. We investigated the clinical features, surgical outcomes, and prognostic factors of HCC presenting with spine metastases, in patients who underwent surgery.
Methods
A retrospective review was conducted on 33 HCC patients who underwent 36 operations (three patients underwent surgical treatment twice) from February 2006 to December 2013. The median age of the patients was 56 years old (range, 28 to 71; male : female=30 : 3).
Results
Overall survival was not correlated with age, sex, level of metastases, preoperative Child-Pugh classification, preoperative ambulatory function, preoperative radiotherapy, type of operation, administration of Sorafenib, or the Tokuhashi scoring system. Only the Tomita scoring system was shown to be an independent prognostic factor for overall survival. Comparing the Child-Pugh classification and ambulatory ability, there were no statistically differences between patients pre- and post-operatively.
Conclusion
The Tomita scoring system represents a practicable and highly predictive prognostic tool. Even though surgical intervention may not restore ambulatory function, it should be considered to prevent deterioration of the patient's overall condition. Additionally, aggressive management may be needed if there is any ambulatory ability remaining.
Hepatocellular carcinoma (HCC) is a rare tumor in Western countries, accounting for less than 2% of all neoplasms in United States. In contrast, HCC is relatively common in Asian countries, where the hepatitis B virus is endemic27). The survival of patients with HCC has been prolonged with improvements in various diagnostic tools and treatment modalities1023). HCC has been also reported to metastasize frequently to the skeletal system-vertebrae, pelvis, ribs, etc.-with an incidence ranging from 2% to 16%122226). It is estimated that 40% of bone metastases are spinal metastases15). Consequently, spinal metastases from HCC are diagnosed more frequently.
The treatment of metastatic spine disease has evolved significantly in the past decade with the advancements in surgical and radiation techniques2). As surgical techniques and instruments improve, surgical treatment followed by adjuvant radiotherapy is affording a longer survival period and better quality of life than radiotherapy alone92128). Recently, a minimally invasive surgical technique, spine radiosurgery, and new targeted chemotherapy have been introduced. These treatment modalities are being applied clinically4813172435). If a patient experiences neurologic deterioration or loss of stability, surgical decompression and stabilization with instrumentation may be a better option than radiotherapy, considering the delayed response of solid tumors to radiotherapy692834).
The aim of the study was to determine the long-term surgical treatment outcomes associated with the systemic condition of HCC presenting with spine metastases, and to figure-out the survival-related factors.
Patients who underwent an operation for spinal HCC metastases from February 2005 to December 2013 in the Spine Center of the authors' institute were enrolled in this study. All patients complained of neck pain or back pain. Some patients had neurologic symptoms, including lower extremity weakness or urinary retention. Patients with susceptive instability, spinal instability neoplastic score (SINS) over score of 6, and/or patients who already received radiotherapy, or stereotactic radiosurgery, underwent operation. Patients who underwent a vertebroplasty or Kyphoplasty procedure were not included in this study
Patient demographics and clinical characteristics were obtained from the patients' electronic medical records. We evaluated the patients' predisposing factors for primary HCC. The general condition of patients, including liver function, was evaluated using the Child-Pugh classification29). To evaluate instability of tumor SINS was calculated11). To evaluate a condition of tumor the Tokuhashi scoring system (general condition, number of extraspinal bone metastases foci, number of metastases in the vertebral body, metaseses to the major internal organs, primary site of the cancer, and palsy)31), and the Tomita scoring system (primary site of the cancer, number of visceral metastases, and number of bone metastases)32) was calculated in all patients. Recently, the authors have proposed revisions, resulting in modified Tomita and Tokuhashi scoring systems for spinal metastasis20). We applied these scoring systems also. Instability was evaluated with SINS11). Ambulatory function was evaluated from medical records. A patient who could walk even with an ambulatory aid was considered as possible, and a patient who could not walk at the out-patient department after the operation was considered as not-possible. Chemotherapy regimen was retrospectively evaluated from prescription of medical records.
Patients with refractory pain, neurological deficit, or the potential for neurological deficit were indicated for surgery. Thirty-three patients with spinal HCC metastases underwent operations. Three patients had two spinal operations each, at different levels, so 36 operations were performed in all. The goals of the metastatic spinal tumor surgery were : to decompress a neural component and/or stabilize the spine to improve neurological deficits and alleviate pain. In most cases, instrumentation was performed for stabilization, by anterior, posterior, or circumferential means.
Preoperatively, conventional radiotherapy to the index spine was performed in 11 cases (total dose range, 20 Gy to 39 Gy). One patient received stereotactic radiosurgery with 20 Gy/1 Fr.
Statistical analyses of variables were carried out using commercial software (PASW Statistics, version 22; SPSS Inc., Chicago, IL, USA). The survival rate was estimated by the Kaplan-Meier method, and differences were analyzed by the log-rank test. Comparison between preoperative status and postoperative status was analyzed by a Wilcoxon signed rank test. The results were considered significant for probability values less than 0.05.
Thirty patients were male, and 3 patients were female. The patients' median age at the initial operation was 56 years (range, 28 years to 71 years). Four patients had been diagnosed with spinal metastases simultaneously (within one month) of their primary HCC diagnoses. In the other 29 patients, the spinal metastases occurred more than 6 months after the diagnosis of primary HCC (median interval, 18 months; range, 6-86 months). Twenty-nine patients were hepatitis B viral carriers, one was a hepatitis C viral carrier, and other three patients were non-hepatitis B, non-hepatitis C viral carriers. Among the three patients, one patient had a history of heavy alcoholic consumption. Preoperatively, 29 patients were Child-Pugh class A, 4 were class B, and no patient was class C. Preoperatively, 11 patients lost their ambulatory function, and 25 patients maintained their ambulatory function. Some required ambulatory aids. There was no statistically significant difference between the pre-and post-operative status of Child-Pugh classification and ambulatory function. Spinal metastases were located at the cervical level (n=10), thoracic level (n=15), and lumbar level (n=11). In terms of SINS, 2 patients were score of 6, 29 patients were between 7 and 12, 5 patients were between 13 and 18.
Among the subjects, there were several post-operative complications. One patient died during admission due to pneumonia. There was one case of cerebro-spinal fluid leakage after a dural tear. There was one case of operative site infection.
During the follow-up period, 27 patients died, three patients were lost to follow-up, and three patients survived. The median overall survival was 261 days (range, 22-1359 days) after the diagnosis of metastasis, and 180 days (range, 19-1351 days) after the initial operation. As determined by Kaplan-Meier survival analysis, the survival time was not related with age, sex, location of tumor, preoperative Child-Pugh classification, preoperative ambulatory function, preoperative radiotherapy status, type of operation, or the administration of Sorafenib (Table 1).
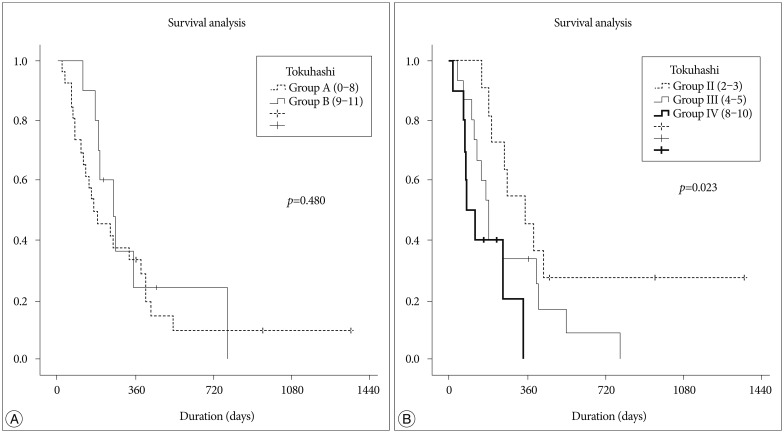
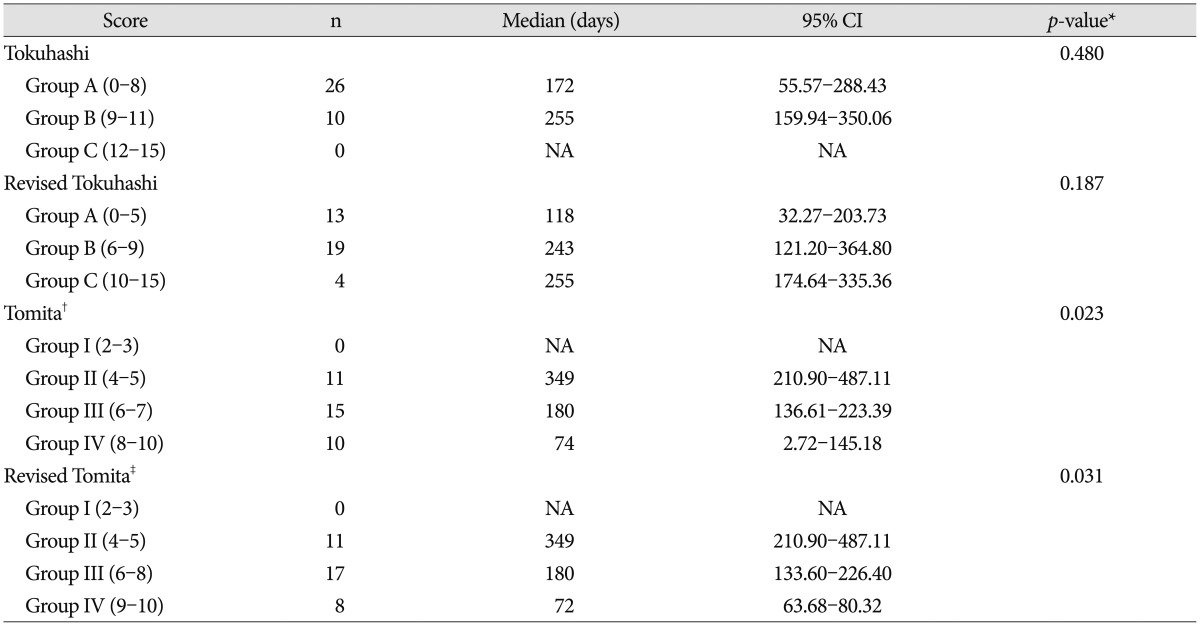
Patients were classified by Tokuhashi but the classifications showed no significant difference between groups. When patients were classified by Tomita score, there was a statistically significant difference between the groups (p=0.023). Applying the revised Tokuhashi and Tomita scoring systems, the results were quite similar (Table 2, Fig. 1).
The survival time of patients with HCC has increased to more than 2 years during the past decade33). Hence, it is more common to encounter a patient with spinal metastases. Spinal metastases can cause neurologic deficits with or without compression fractures, and back pain, both of which affect the patient's quality of life and result in poor outcomes1). Recent studies show poor overall survival after a diagnosis of spinal metastasis, usually around a year71936). Therefore, spinal metastasis from HCC is still devastating to patients.
There were several studies conducted to estimate prognosis of spinal metastases using different parameters. Chen et al.7) compared the existing preoperative scoring systems-the Tokuhashi scoring system, the Tomita scoring system, the van der Linden scoring system, and the Bauer and Wedin scoring system-to find useful prognostic factors. They found the Tokuhashi scoring system provided statistically significant results. In addition, serum albumin (≥37 g/L) and LDH (<200 U/L) were found to be better prognostic factors. However, our study and a study by Zhang et al.36), show the Tomita scoring system is an independent prognostic factor. These studies show the limitations of the existing preoperative scoring system, and suggest a need for a new prognostic scoring system. Due to advances in medical treatment and anesthesology, researchers have proposed a new prognostic scoring system by modifying the Tokuhashi and Tomita scoring systems20). The resulting systems seem to be more prognostic than previous scoring systems for patients with tumors of the entire spine. But, with the small number of patients, the validation was limited in this study. Kim et al.19) suggest that preoperative ambulatory status and hepatic function (Child-Pugh classification) were significantly correlated with survival time. But, Child-Pugh classification was not shown to predict the prognosis of HCC patients with spinal metastases in our study.
The current recommendation of high-grade spinal cord compression for solid spine metastases is surgical decompression and radiotherapy to achieve local tumor control. Patchell et al.28) in 2005 showed better outcomes for patients undergoing surgery and radiation therapy compared to patients undergoing radiation treatment alone. The optimal interval between surgery and radiotherapy was studied using a systemic review18). They suggested the time interval between treatment modalities should be at least 1 week to minimize wound complications.
Maranzano and Latini25) reported that radioresistant tumors, such as HCC, demonstrated only a 20% response rate in conventional radiotherapy; in contrast, radiosurgery for spine metastases has demonstrated better clinical responses. Yamada et al.35) published a prospective cohort study, regarding treatment with radiosurgery for radioresistant oligometastatic tumors. With dose-escalation from 18 Gy to 24 Gy, local control was 92%. Many other studies reported that radiosurgery for metastatic spine disease is safe and effective with durable symptomatic responses and local control for radioresistant histologies3451430). As confidence and experience with the use of radiosurgery as a postoperative adjuvant grow, surgical resection of metastatic disease has become less aggressive, with the expectation that radiosurgery will control the residual disease. We validated the effect of radiation therapy in our patient cohort. Preoperative radiation therapy was not shown to help prolong the overall survival of the patients. Upfront radiation therapy was also ineffective in prolonging the overall survival of the patients.
Recently, target agents have been suggested to be a promising treatment modality. Sorafenib is an orally active multi-kinase inhibitor that has proven to prolong overall survival and progression-free survival in advanced HCC824). But, the difference of survival time between the group who were prescribed Sorifenib and the group that did not receive it was not significant in the HCC with spinal metastasis patients.
The most important goal of surgical resection in patients with spinal metastases is to preserve or restore neurological function. Kim et al.19) reported a 29% (4/14) rate of restoration of ambulatory function. Preoperative ambulatory ability was significantly correlated with the postoperative ambulation period in their study16). Previously, Chen et al.7) reported a restoration rate of more than 50%. In contrast, our study shows an 18% (2/11) rate of restoration of ambulatory function. In fact, there was no difference of ambulatory ability status between pre- and post-operatively in the present study. Most patients had surgical decompression within a week after visiting the hospital. However, 6 patients visited the hospital more than one week after the symptom occurred, and some came after 20 days. The population of the other study underwent operations within 3 days. This difference might have affected the result.
As this result is based on a retrospective medical record review, the data is limited, and a prospective study should be conducted to further validate its findings.
For patients with spinal metastases from HCC, survival time was not correlated with age, sex, level, preoperative Child-Pugh classification, preoperative ambulatory function, preoperative radiotherapy, type of operation, administration of Sorafenib at any point, or the Tokuhashi scoring system. Only the Tomita scoring system was shown to provide practicable and highly predictive prognostic value in patients with spinal metastases from HCC. Considering the other reports, the existing scoring system has limitations for patients with spinal metastses. A new prognostic scoring system should be introduced. Still, surgical treatment is a prerequisite for the restoration of stability or immediate decompression. The technology and other advancements in chemotherapy and radiotherapy are rapidly improving, so target agents or radiosurgery are potentially very promising. With the advent of effective multimodality treatments, the patients' survival and quality of life will be improved.
References
1. Abrahm JL, Banffy MB, Harris MB. Spinal cord compression in patients with advanced metastatic cancer : "all I care about is walking and living my life". JAMA. 2008; 299:937–946. PMID: 18314436.

2. Bilsky MH, Laufer I, Burch S. Shifting paradigms in the treatment of metastatic spine disease. Spine (Phila Pa 1976). 2009; 34(22 Suppl):S101–S107. PMID: 19829269.

3. Chang EL, Shiu AS, Mendel E, Mathews LA, Mahajan A, Allen PK, et al. Phase I/II study of stereotactic body radiotherapy for spinal metastasis and its pattern of failure. J Neurosurg Spine. 2007; 7:151–160. PMID: 17688054.

4. Chang UK, Kim MS, Han CJ, Lee DH. Clinical result of stereotactic radiosurgery for spinal metastasis from hepatocellular carcinoma : comparison with conventional radiation therapy. J Neurooncol. 2014; 119:141–148. PMID: 24803002.

5. Chao ST, Koyfman SA, Woody N, Angelov L, Soeder SL, Reddy CA, et al. Recursive partitioning analysis index is predictive for overall survival in patients undergoing spine stereotactic body radiation therapy for spinal metastases. Int J Radiat Oncol Biol Phys. 2012; 82:1738–1743. PMID: 21489717.

6. Chataigner H, Onimus M. Surgery in spinal metastasis without spinal cord compression : indications and strategy related to the risk of recurrence. Eur Spine J. 2000; 9:523–527. PMID: 11189921.

7. Chen H, Xiao J, Yang X, Zhang F, Yuan W. Preoperative scoring systems and prognostic factors for patients with spinal metastases from hepatocellular carcinoma. Spine (Phila Pa 1976). 2010; 35:E1339–E1346. PMID: 20938387.

8. Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma : a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009; 10:25–34. PMID: 19095497.

9. Cole JS, Patchell RA. Metastatic epidural spinal cord compression. Lancet Neurol. 2008; 7:459–466. PMID: 18420159.

10. El-Serag HB, Marrero JA, Rudolph L, Reddy KR. Diagnosis and treatment of hepatocellular carcinoma. Gastroenterology. 2008; 134:1752–1763. PMID: 18471552.

11. Fourney DR, Frangou EM, Ryken TC, Dipaola CP, Shaffrey CI, Berven SH, et al. Spinal instability neoplastic score : an analysis of reliability and validity from the spine oncology study group. J Clin Oncol. 2011; 29:3072–3077. PMID: 21709187.

12. Fukutomi M, Yokota M, Chuman H, Harada H, Zaitsu Y, Funakoshi A, et al. Increased incidence of bone metastases in hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2001; 13:1083–1088. PMID: 11564960.

13. Gerszten PC, Burton SA, Ozhasoglu C, Welch WC. Radiosurgery for spinal metastases : clinical experience in 500 cases from a single institution. Spine (Phila Pa 1976). 2007; 32:193–199. PMID: 17224814.
14. Gerszten PC, Mendel E, Yamada Y. Radiotherapy and radiosurgery for metastatic spine disease : what are the options, indications, and outcomes? Spine (Phila Pa 1976). 2009; 34(22 Suppl):S78–S92. PMID: 19829280.
15. He J, Zeng ZC, Tang ZY, Fan J, Zhou J, Zeng MS, et al. Clinical features and prognostic factors in patients with bone metastases from hepatocellular carcinoma receiving external beam radiotherapy. Cancer. 2009; 115:2710–2720. PMID: 19382203.

16. Helweg-Larsen S, Sørensen PS, Kreiner S. Prognostic factors in metastatic spinal cord compression : a prospective study using multivariate analysis of variables influencing survival and gait function in 153 patients. Int J Radiat Oncol Biol Phys. 2000; 46:1163–1169. PMID: 10725627.

17. Horn EM, Henn JS, Lemole GM Jr, Hott JS, Dickman CA. Thoracoscopic placement of dual-rod instrumentation in thoracic spinal trauma. Neurosurgery. 2004; 54:1150–1153. discussion 1153-1154PMID: 15113470.

18. Itshayek E, Yamada J, Bilsky M, Schmidt M, Shaffrey C, Gerszten P, et al. Timing of surgery and radiotherapy in the management of metastatic spine disease : a systematic review. Int J Oncol. 2010; 36:533–544. PMID: 20126972.
19. Kim CH, Chung CK, Jahng TA, Kim HJ. Surgical outcome of spinal hepatocellular carcinoma metastases. Neurosurgery. 2011; 68:888–896. PMID: 21221023.

20. Kim J, Lee SH, Park SJ, Chung SS, Kim ES, Eoh W, et al. Analysis of the predictive role and new proposal for surgical strategies based on the modified Tomita and Tokuhashi scoring systems for spinal metastasis. World J Surg Oncol. 2014; 12:245. PMID: 25085251.

21. Klimo P Jr, Thompson CJ, Kestle JR, Schmidt MH. A meta-analysis of surgery versus conventional radiotherapy for the treatment of metastatic spinal epidural disease. Neuro Oncol. 2005; 7:64–76. PMID: 15701283.

22. Kuhlman JE, Fishman EK, Leichner PK, Magid D, Order SE, Siegelman SS. Skeletal metastases from hepatoma : frequency, distribution, and radiographic features. Radiology. 1986; 160:175–178. PMID: 3012630.

23. Llovet JM, Bruix J. Molecular targeted therapies in hepatocellular carcinoma. Hepatology. 2008; 48:1312–1327. PMID: 18821591.

24. Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008; 359:378–390. PMID: 18650514.

25. Maranzano E, Latini P. Effectiveness of radiation therapy without surgery in metastatic spinal cord compression : final results from a prospective trial. Int J Radiat Oncol Biol Phys. 1995; 32:959–967. PMID: 7607970.

26. Okazaki N, Yoshino M, Yoshida T, Hirohashi S, Kishi K, Shimosato Y. Bone metastasis in hepatocellular carcinoma. Cancer. 1985; 55:1991–1994. PMID: 2983871.

27. Park KW, Park JW, Choi JI, Kim TH, Kim SH, Park HS, et al. Survival analysis of 904 patients with hepatocellular carcinoma in a hepatitis B virus-endemic area. J Gastroenterol Hepatol. 2008; 23:467–473. PMID: 17764529.

28. Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer : a randomised trial. Lancet. 2005; 366:643–648. PMID: 16112300.

29. Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973; 60:646–649. PMID: 4541913.

30. Sohn S, Chung CK. The role of stereotactic radiosurgery in metastasis to the spine. J Korean Neurosurg Soc. 2012; 51:1–7. PMID: 22396835.

31. Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 2005; 30:2186–2191. PMID: 16205345.

32. Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001; 26:298–306. PMID: 11224867.

33. Tralhão JG, Dagher I, Lino T, Roudié J, Franco D. Treatment of tumour recurrence after resection of hepatocellular carcinoma. Analysis of 97 consecutive patients. Eur J Surg Oncol. 2007; 33:746–751. PMID: 17188454.

34. Witham TF, Khavkin YA, Gallia GL, Wolinsky JP, Gokaslan ZL. Surgery insight : current management of epidural spinal cord compression from metastatic spine disease. Nat Clin Pract Neurol. 2006; 2:87–94. quiz 116PMID: 16932530.

35. Yamada Y, Bilsky MH, Lovelock DM, Venkatraman ES, Toner S, Johnson J, et al. High-dose, single-fraction image-guided intensity-modulated radiotherapy for metastatic spinal lesions. Int J Radiat Oncol Biol Phys. 2008; 71:484–490. PMID: 18234445.

36. Zhang D, Xu W, Liu T, Yin H, Yang X, Wu Z, et al. Surgery and prognostic factors of patients with epidural spinal cord compression caused by hepatocellular carcinoma metastases : retrospective study of 36 patients in a single center. Spine (Phila Pa 1976). 2013; 38:E1090–E1095. PMID: 23632333.
Table 1
Survival analysis with risk factors
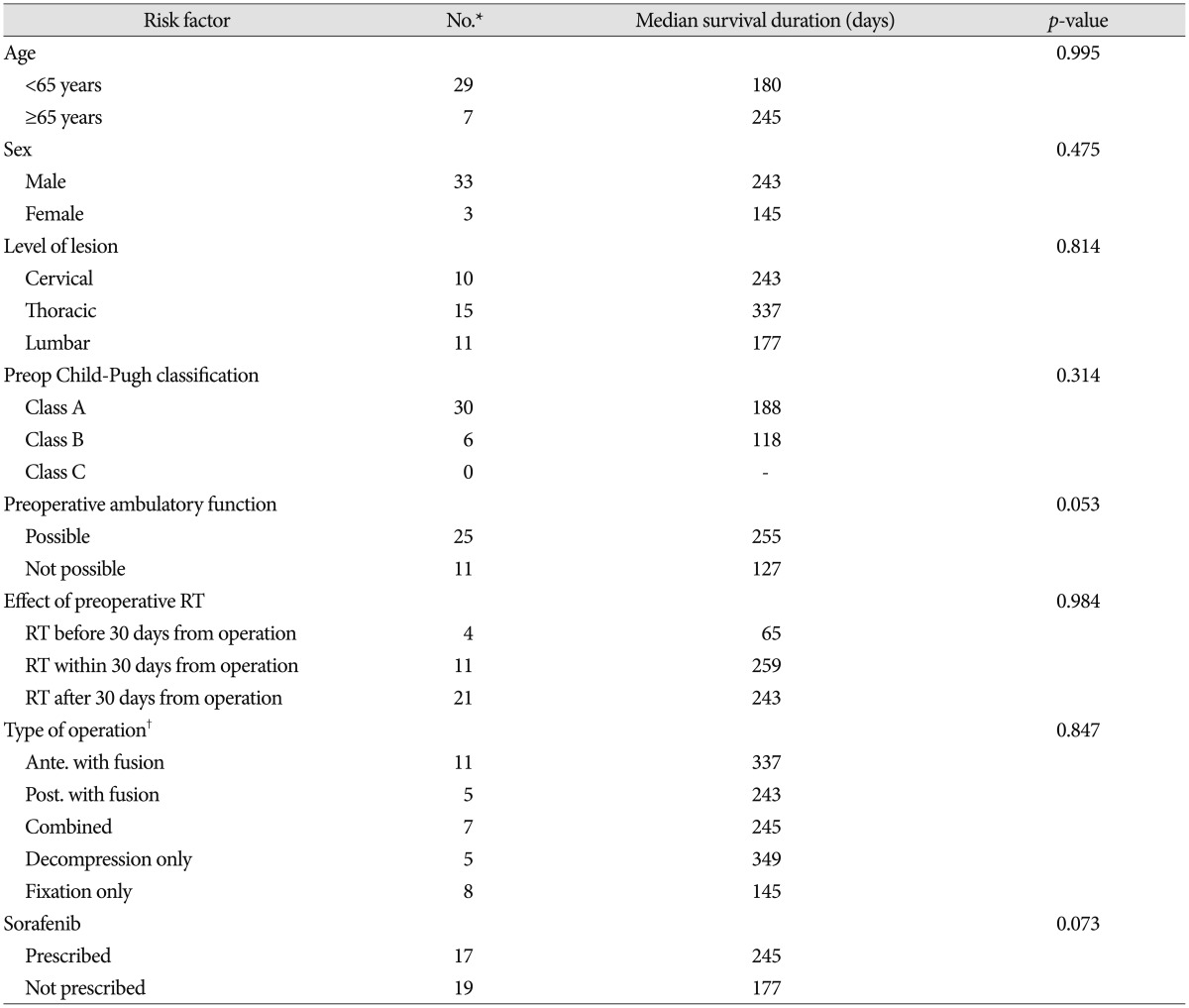
The survival rate was estimated by the Kaplan-Meier method, and differences were analyzed by the log-rank test. *Numbers are representative of surgical cases, †Type of operation is classified as anterior decompression with instrumentation (ante. with fusion); posterior decompression with instrumentation (post. with fusion); anterior and posterior decompression with circumferential instrumentation (combined); posterior decompression only (decompression only); and posterior percutaneous fixation only (fixation only). RT : radiotherapy




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download