Abstract
Objective
Dynesys® is one of the pedicle-based dynamic lumbar stabilization systems and good clinical outcome has been reported. However, the cylindrical spacer between the heads of the screws undergoes deformation during assembly of the system. The pre-strain probably change the angle of instrumented spine with time and oblique-shaped spacer may reduce the pre-strain. We analyzed patients with single-level stabilization with Dynesys® and simulated oblique-shaped spacer with finite element (FE) model analysis.
Methods
Consecutive 14 patients, who underwent surgery for single-level lumbar spinal stenosis and were followed-up more than 24 months (M : F=6 : 8; age, 58.7±8.0 years), were analyzed. Lumbar lordosis and segmental angle at the index level were compared between preoperation and postoperative month 24. The von Mises stresses on the obliquely-cut spacer (5°, 10°, 15°, 20°, 25°, and 30°) were calculated under the compressive force of 400 N and 10 Nm of moment with validated FE model of the L4-5 spinal motion segment with segmental angle of 16°.
Results
Lumbar lordosis was not changed, while segmental angle was changed significantly from -8.1±7.2° to -5.9±6.7° (p<0.01) at postoperative month 24. The maximum von Mises stresses were markedly decreased with increased angle of the spacer up to 20°. The stress on the spacer was uneven with cylindrical spacer but it became even with the 15° oblique spacer.
Dynamic stabilization has been introduced to address the problem of motion limitation and adjacent segment pathology with rigid fixation for degenerative lumbar spine disease222242628303233). Dynamic stabilization systems are largely divided into two groups based on the way in which they are attached to the spine : inter-spinous system and pedicle screw-based system. Dynesys® (Zimmer, Winterthur, Switzerland) is one of the pedicle screw-based dynamic stabilization systems and has been used to stabilize lumbar segments following spinal canal decompression323303134). The Dynesys system is composed of titanium alloy (Protasul-100) pedicle screws, polyethyleneterephthalate (Sulene-PET) cords, and polycarbonateurethane (Sulene-PCU) spacers9212432). The spacers and cord connect the upper and lower pedicle screws in the Dynesys system and allows motion between vertebras, on contrary to the metallic rod in the standard fusion system. During assembly of the Dynesys, the cord is pulled tight with 300 N force, approximating the two screw heads to the extent that the interposed cylindrical spacer allows4112024). The pre-tension on the cord is essential procedure for the stability of the system41120). We focused on the pre-strain of the system. The cylindrical spacer between the heads of the screws undergoes deformation during tightening of the cord, because the pedicle screws are usually inserted parallel to the endplates of each vertebrae, which are not parallel to each other. This probably causes reaction force on the pedicle screw and vertebrae, and the ongoing force may change the angle of instrumented vertebra with time in vivo911). We hypothesized that the reaction force may be reduced by cutting the bottom of the spacer obliquely. In the present study, we retrospectively analyzed sagittal alignment of lumbar spine for patients with single-level instrumentation with Dynesys. The hypothesis was simulated with a validated finite element (FE) model analysis27)
From 2005-2010, 22 patients underwent dynamic stabilization with Dynesys for single-level lumbar spinal stenosis. Among them, consecutive 14 patients who were followed-up more than 24 months (M : F=6 : 8; age, 58.7±8.0 years; range, 46-73) were included. Surgical indication was degenerative lumbar spinal stenosis with neurological intermittent claudication, which was intractable for non-surgical management at least for 6 months714). Spondylolistheis was present in 8/14 patients. If index level showed angle change of 10-15° between the cephalic and caudal vertebrae end plates on preoperative dynamic view or spondylolisthesis, this level was included in the level of stabilization728). Dynamic stabilization was not performed on patients with overt instability (>15 angle change and/or >3 mm translation), fixed coronal imbalance, previous lumbar spine surgery, spondylolisthesis more than grade II or an associated movement disorder (such as Parkinson's disease)1214). The operated levels were like followings; L2-3, 2; L3-4, 2; L4-5, 9; L5-S1, 1 patient(s) and low grade spondylolisthesis (≤10% slippage) was combined in 9 patients.
The surgical procedures were followed the manufacturer's guideline for the Dynesys® spinal system (Zimmer, Winterthur, Switzerland). After decompression with posterior midline incision with laminectomy or laminotomy, four pedicle screws were inserted parallel to the endplate of each vertebral body. The head of pedicle screws were connected with the cord, and cylindrical spacer was interposed after measuring the distance between the head of pedicle screw. The cord was tightened with 300 N compressive force. The patients were scheduled to follow-up at postoperative 1, 3, 6, 12 months and yearly thereafter. Plain X-ray was taken at 1, 6, 12 months and yearly thereafter. Follow-up period was 52.6±23.7 months (range, 24-85).
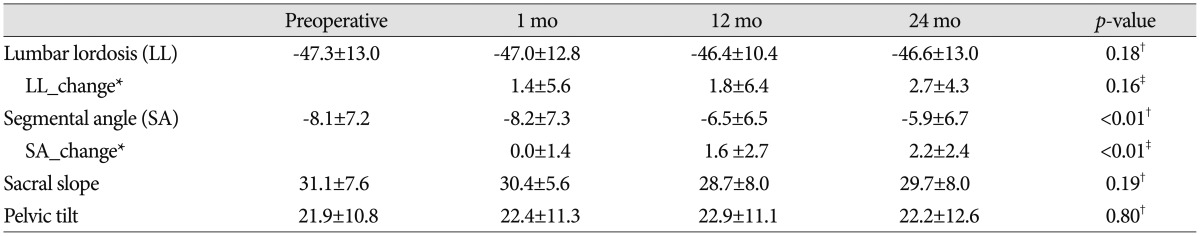
For clinical parameters, the visual analogue pain score (VAS, scale 0-10) and the Korean version of the Oswestry disability index (K-ODI, scale 0-45) scores15) were assessed at preoperatively and at each follow-up appointments (1, 3, 6, and 12 months and yearly thereafter). Pelvic parameters (pelvic incidence, pelvic tilt and sacral slope) were measured with functions found in the picture archiving and communication systems (Marosis, version 5483, Infinitt Healthcare, Seoul, Korea), which ran in a Microsoft Windows environment (Microsoft Corp., Redmond, WA, USA) as suggested before113). Lumbar lordosis angle (LL, T12-S1) and segmental angle between superior endplate and inferior endplate of instrumented cephalic and caudal vertebral body were measured with Cobb's method113). Negative angle denoted a lordosis. For patients with spondylolisthesis, percentages of slip (100×length of slip/length of superior endplate) were compared.
All continuous values were described as mean±standard deviation. Parameters obtained at postoperative month 24 were compared with preoperative ones. Continuous values were compared with either Mann-Whitney U test or Wilcoxon-Rank sum test. All statistical analyses were done using SPSS (version 17.0, SPSS Inc., Chicago, IL, USA), and statistical significance was defined as p<0.05 (two-sided).
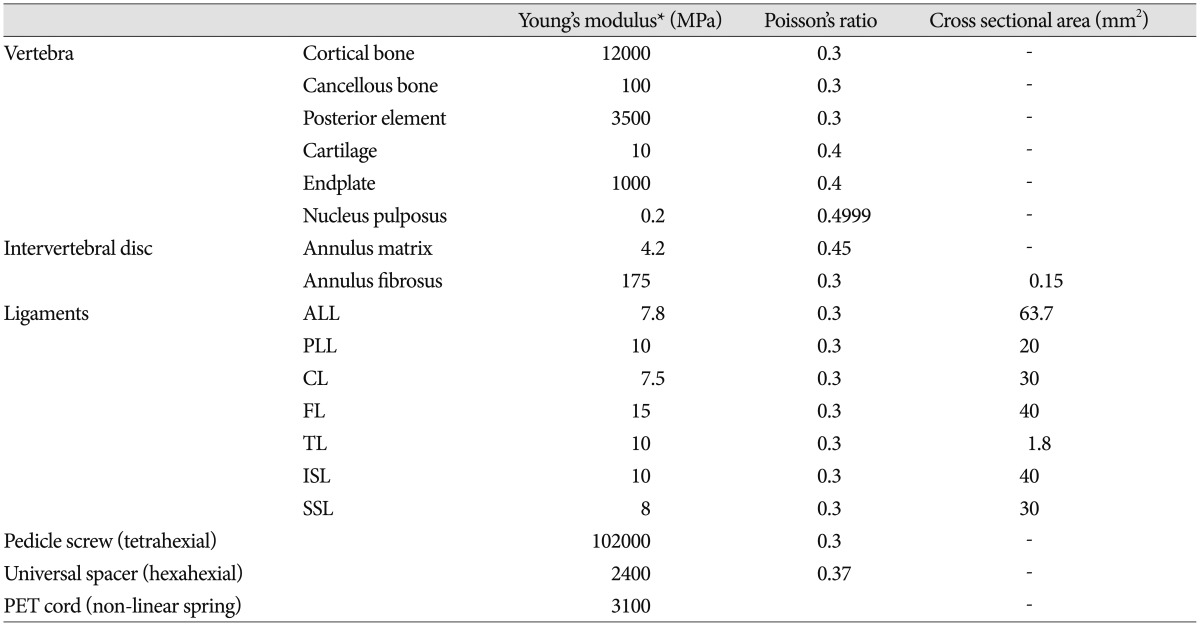
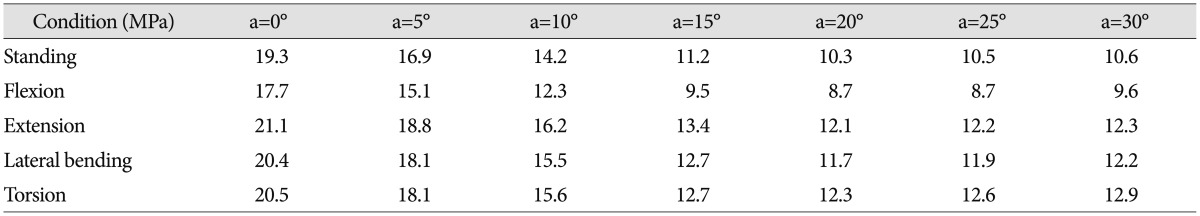
To simulate the effect of obliquely-cut spacer, seven different FE models with various slope of the inferior plane of the spacer (0°, 5°, 10°, 15°, 20°, 25°, and 30°) between the top and bottom planes were made by cutting the bottom of the spacer obliquely. Three-dimensional computer-aided design (CAD) models of pedicle screws, spacers, and cords for the Dynesys system were developed based on manufacturing drawings using SolidWorks® (SolidWorks Corp., Concord, MA, USA). The pedicle screw with a diameter of 6.4 mm and length of 35 mm was selected. The developed CAD models were transformed to the FE models with the software FEMAP v. 10 (UGS Inc., Plano, TX, USA)17). The material properties of the components used for the FE models were described in Table 1916212432). For the spinal segment with Dynesis implantation, the FE model of a L4-5 spinal motion segment with segmental angle of 16° was used16). Two pedicle screw models were inserted parallel to the endplate of each vertebral body6918293234). The distance between the head of upper and lower pedicle screws were 22 mm. The FE model of the spacer was modeled as a cylinder shape, which was 22 mm in length and 12 mm in diameter. It was inserted between the upper and lower pedicle screw heads as the upper plane of the spacer was fixed on the undersurface of the head of the cephalic pedicle screw, and the bottom of the spacer was to fit the superior plane of the lower pedicle screw head. Then, the FE model of the cord was inserted inside the spacer and the cord was fixed at the center of a pedicle screw head. The spacer was fixed under 300 N pretension of cord and it was deformed at dorsal side, because cylindrical spacer was implanted between the screws with a 16° angle (Fig. 1). We hypothesized that obliquely cutting spacer respecting the screw angle may reduce the reaction force due to the deformed spacer. For analysis, a compressive force of 400 N along the direction of the L4 vertebra center to the L5 vertebra center was applied on the L4-5 motion segment as body weight in a standing posture and a moment of 10 Nm was applied onto the superior plane of the L4 vertebra in flexion, extension, lateral bending, and torsion (counterclock-wise) loading condition, respectively (Fig. 1)225). Seven different FE models with various slope of the inferior plane of the spacer (0°, 5°, 10°, 15°, 20°, 25°, and 30°) between the top and bottom planes were made by cutting the bottom of the spacer obliquely (Fig. 2). In order to focus on the single effect of the spacer obliqueness, the clinical factors such as the degenerative spondylolisthesis grade, disc/facet degeneration, and bone mineral density were not considered in the present study. The von Mises stress on the spacer were investigated with the commercial FE analysis software ABAQUS 6.10 (SIMULIA, Providence, RI, USA). Because the von Mises stress is a mechanical parameter which is widely used to determine whether the material is will withstand a given complex load without failure in the mechanical engineering field, it could be considered related to the pre-strain of the spacer in this study.
Preoperative K-ODI, VAS-back, and VAS-neck were 17.7±6.4, 6.3±2.6, and 7.1±1.8, respectively. Postoperatively, pain and disability score were improved significantly; K-ODI, VAS-back, and VAS-neck were 10.6±5.2, 3.2±2.3, and 3.9±2.4 at postoperative month 24 (p=0.01, 0.03, and 0.01, respectively, Wilcoxon-Rank sum test). Excellent outcome was achieved in 3 patients, good outcome was in 8 and fair outcome was in 3 by Nacnab's criteria at postoperative months 24.
LL, sacral slope and pelvic tilt were not significantly changed at postoperative month 24 (Table 2). Preoperative LL was -47.3±13.0° and it was -46.6±13.0° at postoperative month 24 (p=0.18). Preoperative sacral slope and pelvic tilt were 31.1±7.6° and 21.9±10.8°, respectively. At postoperative month 24, sacral slope and pelvic tilt were 29.7±8.0° and 22.2±12.6°, respectively (p=0.19 and 0.80). However, segmental angle was changed significantly from -8.1±7.2° to -5.9±6.7° at postoperative month 24 (p<0.01). The difference of segmental angle between preoperation and postoperative month 24 was 2.2±2.4°. Loss of segmental lordosis was observed in 12/14 patients (7/8 patients with spondylolistheis). Preoperative spondylolisthesis was not a risk factor for the decrease of segmental lordosis (p=1.0). The percentage of slip was 13.0±5.8% at preoperation and 12.1±4.7% at postoperative month 24 (p=0.48). Progression of slip was observed in 1 patient.
A 72-year old female patient complained of neurogenic intermittent claudication and back pain for 1 year (Fig. 3A). Initially, segmental angle of L4-5 was -6.8° and spondylolisthesis was combined. K-ODI and VAS-back, and -leg were 21/45, 8/10 ,and 9/10. Decompressive laminectomy and stabilization of L4-5 was performed (Fig. 3B). The spondylolisthesis was re-aligned and segmental angle of instrumented vertebrae was -12.9° at postoperative month 1. At postoperative month 24, segmental angle was -4.6° (Fig. 3C). Clinical outcome at postoperative month 24 was poor and K-ODI and VAS-back and -leg were 20/45, 7/10, and 7/10.
The result of 14 patients showed that the segmental lordotic angle was significantly decreased during follow-up and we hypothesized that ongoing stress by the spacer without obliquity at the bottom may decrease segmental lordosis. The change of stress with obliquely cutting of the spacer was simulated with FE model. The maximum von Mises stresses on the spacer were markedly decreased in every movement with increasing angles up to 20° (Table 3). The stresses were decreased by 47% in the standing position, by 51% in the flexion position, by 43% in the extension position, by 43% for lateral bending, and by 40% for torsion with a 20° cutting angle. The stresses were similar to each other or slightly increased as the angle increased further.
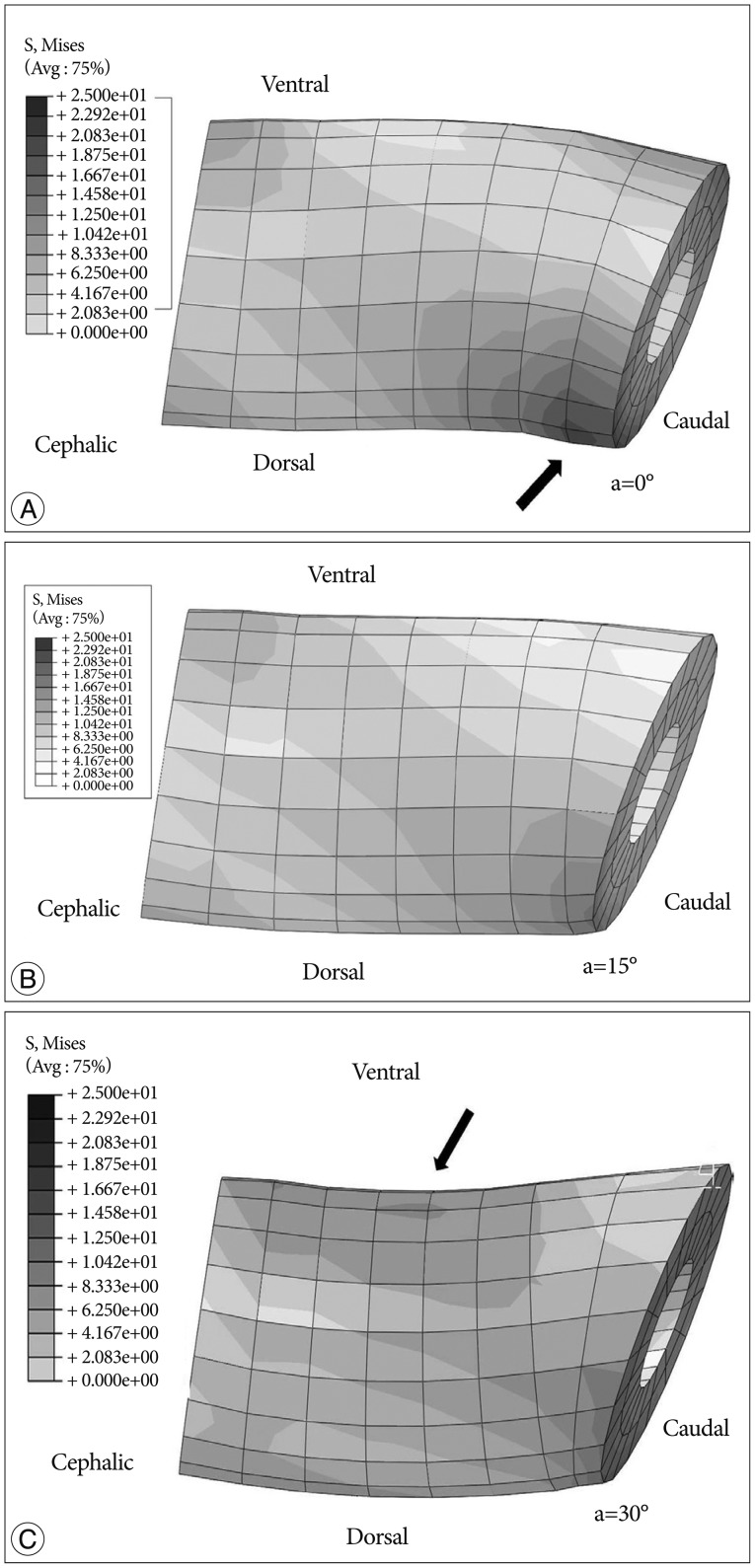
The von Mises stresses on the whole spacer were illustrated in Fig. 4. The von Mises stresses were concentrated at the deformed side of the spacer with a 0° cutting angle (Fig. 4A). The spacer had a pretty even stresses distribution with the cutting angle of 15° (Fig. 4B). Although maximum stresses were nearly similar with further oblique cutting (Table 3), the stresses were converged on the ventral side when the cutting angle was over 20° and the deformation occurred on the ventral side with 30° cutting angle (Fig. 4C). The pre-strain that may change the angle of instrumented screw was reduced with oblique cutting of spacer.
The range of motion (ROM) was simulated. The ROM was 8° in the intact spine and approximately 2° after Dynesys instrumentation. Flexion movement was restricted as the cutting angle increased while extension movement was increased up to 2° with 30° cutting angle. By oblique cutting of 20°, flexion was limited and extension was increased with about 1 degree. However, the effect of oblique cutting on motion during lateral bending and torsion was minimal. The foramen height depends on the length of the spacer. The distance between the centers of the upper and lower planes of the spacer did not change in standing, since the cutting plane was rotated along the center of the lower plane (Fig. 2). The measured distance between the screws decreased by 0.1, 0.4, and 0.6 mm with 10°, 20°, and 30° cutting angles, respectively.
Since the introduction of Dynesys, many authors have presented good surgical results for degenerative spine diseases22242528303233). Although, Dynesys system is a kind of dynamic stabilization instrument, the stiffness is much higher than that of intact spine20). The provided motion at the index level was less than 4 degrees and the problem of rigid fixation was not completely resolved714). Moreover, recent studies showed substantial rate of mechanical failure. The most common mechanical failure was screw loosening, which occurred up to 20% of patients357918192934). In addition to those issues, decrease of segmental lordosis was observed in the present study, although it was obtained from a small group (Table 2). Although the use of Dynesys was not a single factor for the decrease of segmental angle, we speculated that the pre-strain of Dynesys may partially influence on segmental angle. Chien et al.4) showed that the cord pretension (300 N) of Dynesys system can significantly affect both screw-spacer force and bone-screw stress. Recent study showed that spacer deformation was found in most of retrieved spacers, which meant that the spacer was under stress11). The deformed rectangle spacer may tend to parallelize vertebral body due to conjoined pedicle screws, and this tendency may be one of cause of changed segmental angle. However, the deformation of cylindrical spacer was inevitable due to the obliquely angled pedicle screws358). If we reduce the deformation of spacer, such mechanical problems may be reduced. We hypothesized that those issue was probably caused by the unequal distribution of stress on the cylindrical spacer and may be addressed by oblique cutting of the spacer and performed a FE analysis.
The present study was a pilot study to analyze the effect of oblique spacer on the system. In the present model, the lordotic angle between the cranial (L4) and caudal (L5) screw was 16°, which is in agreement with the reported mean angle of 13.1±5.18° in the elderly10). The maximum von Mises stresses on the spacer under compressive force and four bending moments were markedly decreased by 20° cutting angle of spacer and the stresses were slightly changed in further increased angle of the slope (Table 3). The stresses decreased by approximately 40% with a 15-20° cutting angle in every loading condition. Further sloping seems to be detrimental considering uneven distribution of stress on the spacer (Fig. 4C). Considering a pretty even distribution of stresses (Fig. 4B), oblique cutting of the spacer may be effective in reducing mechanical problems, and cutting according to the angle formed between the cephalic and caudal pedicle screws seems to be optimal.
However, there may be a concern about the limitation of flexion motion with an oblique spacer. By oblique cutting of 20°, flexion was limited and extension was increased with about 1 degree. Considering that the reported ROM at the operated segment in patients was about 4°, such a limitation may be acceptable31). Nonetheless, decreasing stress without affecting motion would be better, which should be emphasized in the development of future systems. There may be another concern on the narrowing of the neural foramen with an oblique spacer due to the decreased posterior length of the spacer and increased extension motion. However, the decrease of foraminal height was 0.6 mm in FE model even with 30° oblique spacer, because the distance between the centers of the upper and lower planes of the spacer did not change (Fig. 2). Even though extension motion was increased, the height of the neural foramen could be maintained by the same center height of the spacer irrespective of the obliquity of the cutting angles.
The clinical and radiological outcome was obtained from a small number of patients in a single institute and lacks an external validity. In addition, there was no control group and the follow-up period was too short to make any clinical significance. The effect of reduced lordosis at a single-segment may take a longer time, probably more than decades. The present result is not a conclusive one and we need a long-term follow-up study with data from many institutes to get a conclusive result.
Second, there are many clinical factors that can affect the intersegmental rotation and the stress on the spacer such as the degenerative spondylolisthesis grade, disc/facet degeneration, and bone mineral density. The FE analysis technology was used to investigate the influences of change of design such as the space obliqueness on the stress of the spacer due to difficulties in biomechanical cadaveric experiments as a pilot study, but those clinical factors were not reflected in the present study. Moreover, the action of oblique-shaped spacer with time may be different in a human body. Therefore, direct causal relation-ship with the FE analysis and the clinical result was not clear. Additional biomechanical cadaveric study to reflect the shear force and facet wear inherent in clinical parameters including degenerative spondylolisthesis can be helpful to improve the present study. In addition, durability of the spacer should be tested again because of the re-distribution of stress.
Third, only one-segment geometry and one set of material properties were assumed in the present study. The effect of Dynesys system on the instrumented level may be balanced by un-instrumented levels. Moreover, the change may be minimal considering elasticity of vertebral body and the effect of oblique spacer may be negligible.
Finally, many factors were associated with the changed segmental angle and use of Dynesys was not a single risk factor. Although we showed that the pre-strain of Dynesys may be reduced with change of design, it was a speculative hypothesis and further biomechanical cadaveric study is necessary.
Although there are quite a few limitations, the present pilot study was meaningful in providing an insight into the biomechanics of the Dynesys system. Decrease of segmental lordosis was not a focused issue in the previous studies and further attention is required for the relevant use and refinement of system.
Segmental lordotic angle was decreased after Dynesys stabilization. We hypothesized that the pre-strain generated by the deformed cylindrical spacer between the heads of the screws may change the angle of instrumented spine with time and the oblique-shaped spacer may reduce the pre-strain. The FE model analysis showed that the oblique spacer respecting the angle of instrumented segment (15° or 20° cut) reduced the stress and the refinement may address the issue of decreased segmental lordosis. Further clinical and biomechanical researches are required for relevant use and refinement of the system.
Acknowledgements
This work was supported by the Global Frontier R&D Program on <Human-centered Interaction for Coexistence> funded by the National Research Foundation of Korea grant funded by the Korean Government (MEST) (NRF-2012M3A6A3055889) (Chung CK) and was partially sponsored by GS Medical Co., Korea (Kim YH). The authors clarify that there was no conflict of interest with the instrument used in this manuscript. This study was approved by Institutional Review Board at the Seoul National University Hospital (H-0812-018-265).
References
1. Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007; 16:1459–1467. PMID: 17211522.

2. Bellini CM, Galbusera F, Raimondi MT, Mineo GV, Brayda-Bruno M. Biomechanics of the lumbar spine after dynamic stabilization. J Spinal Disord Tech. 2007; 20:423–429. PMID: 17970182.

3. Bothmann M, Kast E, Boldt GJ, Oberle J. Dynesys fixation for lumbar spine degeneration. Neurosurg Rev. 2008; 31:189–196. PMID: 17906883.

4. Chien CY, Tan CH, Lu TH, Lin SC, Chuang WH, Chiang MC, et al. Pretension effects of the Dynesys cord on the tissue responses and screw-spacer behaviors of the lumbosacral construct with hybrid fixation. Spine (Phila Pa 1976). 2013; 38:E775–E782. PMID: 23486410.

5. Cunningham BW, Dawson JM, Hu N, Kim SW, McAfee PC, Griffith SL. Preclinical evaluation of the Dynesys posterior spinal stabilization system : a nonhuman primate model. Spine J. 2010; 10:775–783. PMID: 20494624.

6. Dakhil-Jerew F, Jadeja H, Cohen A, Shepperd JA. Inter-observer reliability of detecting Dynesys pedicle screw using plain X-rays : a study on 50 post-operative patients. Eur Spine J. 2009; 18:1486–1493. PMID: 19533178.

7. Fay LY, Wu JC, Tsai TY, Wu CL, Huang WC, Cheng H. Dynamic stabilization for degenerative spondylolisthesis : evaluation of radiographic and clinical outcomes. Clin Neurol Neurosurg. 2013; 115:535–541. PMID: 22727211.

8. Gédet P, Haschtmann D, Thistlethwaite PA, Ferguson SJ. Comparative biomechanical investigation of a modular dynamic lumbar stabilization system and the Dynesys system. Eur Spine J. 2009; 18:1504–1511. PMID: 19565278.

9. Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine : surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine (Phila Pa 1976). 2005; 30:324–331. PMID: 15682014.

10. Hammerberg EM, Wood KB. Sagittal profile of the elderly. J Spinal Disord Tech. 2003; 16:44–50. PMID: 12571484.

11. Ianuzzi A, Kurtz SM, Kane W, Shah P, Siskey R, van Ooij A, et al. In vivo deformation, surface damage, and biostability of retrieved Dynesys systems. Spine (Phila Pa 1976). 2010; 35:E1310–E1316. PMID: 20975485.

12. Iguchi T, Ozaki T, Chin T, Tsumura N, Kanemura A, Kasahara K, et al. Intimate relationship between instability and degenerative signs at L4/5 segment examined by flexion-extension radiography. Eur Spine J. 2011; 20:1349–1354. PMID: 21509654.

13. Kim CH, Chung CK, Hong HS, Kim EH, Kim MJ, Park BJ. Validation of a simple computerized tool for measuring spinal and pelvic parameters. J Neurosurg Spine. 2012; 16:154–162. PMID: 22136391.

14. Kim CH, Chung CK, Jahng TA. Comparisons of outcomes after single or multilevel dynamic stabilization : effects on adjacent segment. J Spinal Disord Tech. 2011; 24:60–67. PMID: 21270627.

15. Kim DY, Lee SH, Lee HY, Lee HJ, Chang SB, Chung SK, et al. Validation of the Korean version of the oswestry disability index. Spine (Phila Pa 1976). 2005; 30:E123–E127. PMID: 15738775.

16. Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO. Biomechanical changes of the lumbar segment after total disc replacement : chariter, prodiscr and maverickr using finite element model study. J Korean Neurosurg Soc. 2010; 47:446–453. PMID: 20617091.

17. Kim SM, Yang IC, Lee SY, Cho SY. Dynamic simulation of universal spacer in Dynesys dynamic stabilization system for human vertebra. T Nonferr Metal Soc. 2009; 19:S238–S242.

18. Ko CC, Tsai HW, Huang WC, Wu JC, Chen YC, Shih YH, et al. Screw loosening in the Dynesys stabilization system : radiographic evidence and effect on outcomes. Neurosurg Focus. 2010; 28:E10. PMID: 20568916.
19. Kocak T, Cakir B, Reichel H, Mattes T. Screw loosening after posterior dynamic stabilization--review of the literature. Acta Chir Orthop Traumatol Cech. 2010; 77:134–139. PMID: 20447357.
20. Liu CL, Zhong ZC, Hsu HW, Shih SL, Wang ST, Hung C, et al. Effect of the cord pretension of the Dynesys dynamic stabilisation system on the biomechanics of the lumbar spine : a finite element analysis. Eur Spine J. 2011; 20:1850–1858. PMID: 21523456.

21. Liu CL, Zhong ZC, Shih SL, Hung C, Lee YE, Chen CS. Influence of Dynesys system screw profile on adjacent segment and screw. J Spinal Disord Tech. 2010; 23:410–417. PMID: 20683426.

22. Markwalder TM, Wenger M. Dynamic stabilization of lumbar motion segments by use of Graf’s ligaments : results with an average follow-up of 7.4 years in 39 highly selected, consecutive patients. Acta Neurochir (Wien). 2003; 145:209–214. discussion 214. PMID: 12632117.

23. Meyers K, Tauber M, Sudin Y, Fleischer S, Arnin U, Girardi F, et al. Use of instrumented pedicle screws to evaluate load sharing in posterior dynamic stabilization systems. Spine J. 2008; 8:926–932. PMID: 18037350.

24. Mulholland RC, Sengupta DK. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J. 2002; (11 Suppl 2):S198–S205. PMID: 12384745.

25. Nockels RP. Dynamic stabilization in the surgical management of painful lumbar spinal disorders. Spine (Phila Pa 1976). 2005; 30(16 Suppl):S68–S72. PMID: 16103836.

26. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion : review of the literature. Spine (Phila Pa 1976). 2004; 29:1938–1944. PMID: 15534420.

27. Park WM, Kim K, Kim YH. Effects of degenerated intervertebral discs on intersegmental rotations, intradiscal pressures, and facet joint forces of the whole lumbar spine. Comput Biol Med. 2013; 43:1234–1240. PMID: 23930818.

28. Sapkas GS, Themistocleous GS, Mavrogenis AF, Benetos IS, Metaxas N, Papagelopoulos PJ. Stabilization of the lumbar spine using the dynamic neutralization system. Orthopedics. 2007; 30:859–865. PMID: 17990413.

29. Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976). 2008; 33:E636–E642. PMID: 18708915.

30. Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine (Phila Pa 1976). 2006; 31:442–429. PMID: 16481955.

31. Schulte TL, Hurschler C, Haversath M, Liljenqvist U, Bullmann V, Filler TJ, et al. The effect of dynamic, semi-rigid implants on the range of motion of lumbar motion segments after decompression. Eur Spine J. 2008; 17:1057–1065. PMID: 18493802.

32. Schwarzenbach O, Berlemann U, Stoll TM, Dubois G. Posterior dynamic stabilization systems : Dynesys. Orthop Clin North Am. 2005; 36:363–372. PMID: 15950696.
33. Sengupta DK. Dynamic stabilization devices in the treatment of low back pain. Neurol India. 2005; 53:466–474. PMID: 16565539.

34. Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine : a multi-center study of a novel non-fusion system. Eur Spine J. 11(Suppl 2):2002; S170–S178. PMID: 12384741.
Fig. 1
Three-dimensional finite element model of the Dynesys spinal system implanted L4-5 spinal motion segment with three loading conditions. For analysis, a compressive force of 400 N along the direction of the L4 vertebra center to the L5 vertebra center (vertical thick arrow) is applied onto the L4-5 motion segment as body weight in a standing posture and 10 Nm of moment is applied onto the superior plane of the L4 vertebra in the flexion and extension positions, and for lateral bending (left) and torsion (counterclockwise), respectively. Note deformation of the spacer caused by the implantation of a cylindrical spacer between the screws with a 16° angle.
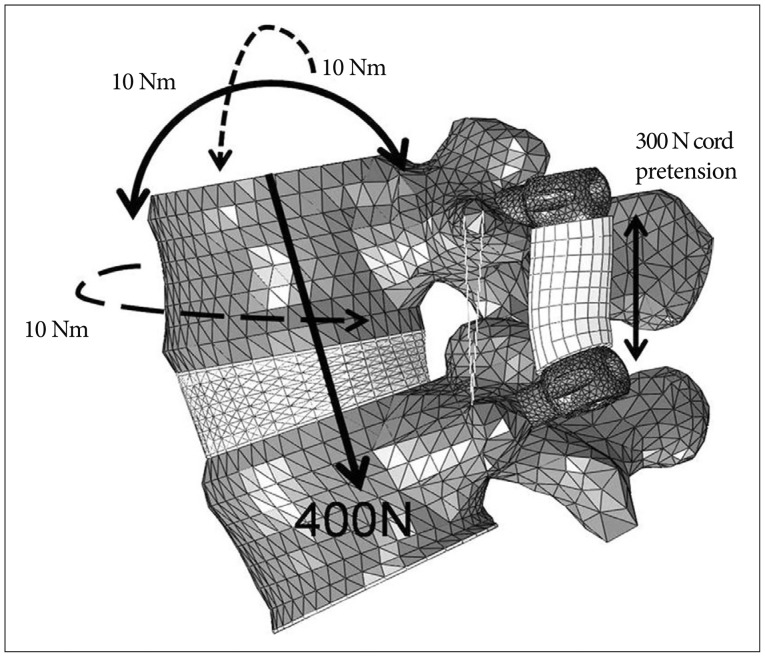
Fig. 2
The method of sloping cylindrical spacer. The inferior border of the spacer is cut with angles (a) of 0°, 5°, 10°, 15°, 20°, 25°, and 30°.
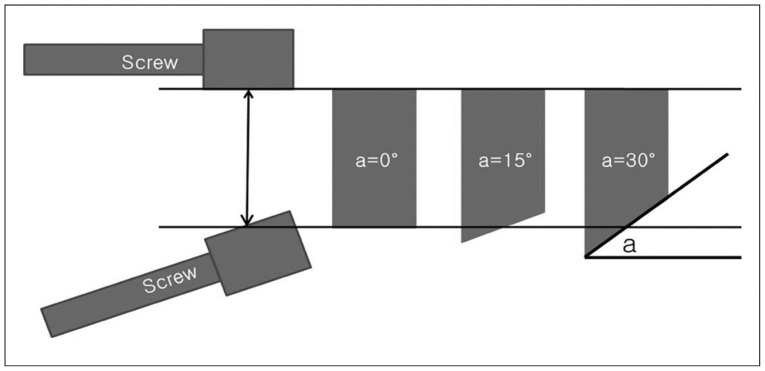
Fig. 3
Decreased segmental angle due to reaction force. A : The preoperative Cobb's angle between L4-5 was -6.8°. B : At postoperative month 1, the angle was -12.9°. C : At postoperative month 24, segmental angle was -4.6°. Note parallelized cephalic and caudal pedicle screw during follow-up.
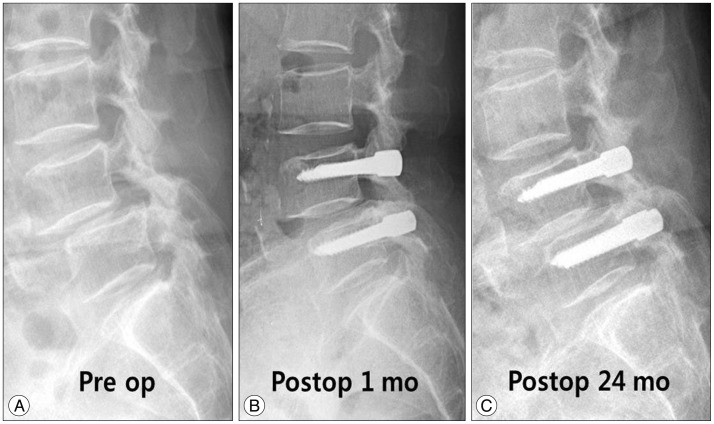
Fig. 4
The maximum von Mises stresses on the spacer. The distribution of von Mises stresses on the spacer was depicted from A-C. Darker color represents higher stress in the figure. A : Initially, the von Mises stresses are concentrated at the dorsal caudal edge (arrow) of the spacer with a 0° cutting angle. B : The spacer has a pretty even distribution of stresses with the cutting angle of 15°. C : The stresses are converged on the ventral side (arrow) with a cutting angle of 30°.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download