Abstract
Objective
The purpose of this study was to evaluate the clinical utility and validity of using a pupillometer to assess patients with acute brain lesions.
Methods
Pupillary examinations using an automated pupillometer (NeurOptics®NPi™-100 Pupillometer) were performed every 4 hours and were simultaneously assessed using the Glasgow Coma Scale (GCS) and for intracranial pressure (ICP), from admission to discharge or expire in neuro-intensive care unit (NICU). Manual pupillary examinations were also recorded for comparison. By comparing these data, we evaluated the validity of using automated pupillometers to predict clinical outcomes.
Results
The mean values of the Neurologic Pupillary index (NPi) were different in the groups examined manually. The GCS correlated well with NPi values, especially in severe brain injury patients (GCS below 9). However, the NPi values were weakly correlated with intracranial pressure (ICP) when the ICP was lower than 30 cm H2O. The NPi value was not affected by age or intensity of illumination. In patients with a "poor" prognosis who had a Glasgow Outcome Scale (GOS) of 1 or 2, the mean initial NPi score was 0.88±1.68, whereas the value was 3.89±0.97 in patients with a "favorable" prognosis who had a GOS greater than 2 (p<0.001). For predicting clinical outcomes, the initial NPi value of 3.4 had the highest sensitivity and specificity.
For the management and prognosis of patients with acute brain injuries, the pupillary light reflex (PLR) is an important factor, in conjunction with other clinical information, such as age, mode of injury and Glasgow Coma Scale (GCS)1214). Terminology generally used to describe the PLR includes "fixed", "sluggish" and "prompt" pupils. These subjective descriptions are often applied without a standard clinical protocol or definition. A more precise evaluation of the PLR and pupil size is problematic because manual pupillary examination is prone to being confounded by inaccuracies and inconsistencies related to large inter-examiner variability and inter-observer disagreement41019). In contrast, automated pupillometer provide objective and quantitative information about the PLR in the form of the Neurologic Pupil index (NPi) value, which is derived from an algorithm that includes pupil size, latency, constriction velocity, and dilation velocity4).
The present study aims to evaluate the validity of automated pupillometer use in a prospective cohort of 117 patients with acute brain lesions.
Data were collected prospectively from 121 consecutive patients who were admitted to the neuro-intensive care unit (NICU) with an acute brain injury between March 2014 and October 2014. Patients admitted to NICU after regular surgical intervention were excluded from this study. Four patients were excluded from this study because three of them received binocular surgical procedures and the other had glial tumor infiltration in the midbrain. Thus, a total of 117 patients were finally enrolled in this study.
The study group was composed of 69 men and 48 women with a median age of 56 years from 16 to 90 years. The radiologic diagnoses in our study group were as follows : aneurysmal subarachnoid hemorrhage in 41 patients, spontaneous intracerebral hemorrhage in 44 patients, traumatic brain injury in 28 patients and cerebral infarction in 4 patients. The initial neurologic status of our cohort was assessed by the GCS. Ninety-one patients had a mild to moderate brain injury, which is represented by a GCS score of 9 or more, and 26 patients had a severe brain injury with a GCS of 8 or less.
Pupillary examinations using an automated pupillometer (NeurOptics®NPi™-100 Pupillometer, Neuroptics Inc., Irvine, CA, USA) were performed every 4 hours. A pupillometer is a handheld optical scanner that stimulates the eye with a flash of light and captures and analyzes a rapid sequence of digital images to obtain a temporal measurement of the diameter of a human pupil (Fig. 1). It analyzes the captured image data and displays a summary of the measurements on the screen. The NPi algorithm was developed to quantify pupillary reactivity and to remove subjectivity from this assessment3). Each variable from an individual pupil measurement taken by the pupillometer is compared against the mean of a reference distribution of healthy subjects for the same variable. Finally, the set of all the standardized differences (or z-scores) were combined to fall into a scale set between 0 and 5. An NPi value closer to 5 is considered more "prompt" and an NPi value closer to zero denotes a more abnormal PLR. Both eyes were tested in all patients, and inspection time was less than 30 seconds per person.
A GCS estimation and a manual pupillary examination were simultaneously performed with each exam by pupillometer. Intracranial pressure (ICP) was also evaluated in available patients. The results of the manual pupillary examination were classified as "fixed", "sluggish" and "prompt" and the mean NPi value in each group were calculated. We used the lower NPi value of both eyes to assess the relationship of the NPi value with GCS, ICP or clinical outcome. To view the relationship between NPi value and GCS, the patients were divided into four groups (GCS 3 to 5, GCS 6 to 8, GCS 9 to 12, and GCS 13 to 15), and the average NPi value was calculated. Twenty-seven patients were available for the measurement of ICP. Seventeen patients had indwelling extra-ventricular drainage catheters, and 10 patients had ICP monitoring catheters. Classification by ICP grouped patients into 3 categories (lower than 15 cm H2O, 15 cm H2O to 30 cm H2O, and higher than 30 cm H2O), and the relationship between NPi value and each category was analyzed.
We also evaluated the influence of illumination and age on NPi as an aspect of the validity analysis. We compared the mean NPi value measured during the daytime (8 a.m. to 20 p.m.) with the value measured at night. We analyzed the difference in NPi between an older patient group (65 years old or older) and a younger group (below 65 years old). These two analyses were performed in patients with a GCS of 9 or higher.
To determine the predictive value of NPi in terms of clinical outcomes, we used the Glasgow Outcome Scale (GOS) at 1 month after the onset of event. The clinical outcome was classified as "favorable" if the GOS 1 month after the event was equal to or greater than 3 and "poor" if the GOS was below 3. We compared initial NPi values in these two groups. The area under the receiver operating characteristic (ROC) curve was used to assess the cut-off value for predicting clinical outcomes. True positive was defined as a group with an NPi lower than the cut-off value and a "poor" outcome. False positive was defined as a group having an NPi lower than the cut-off value and a "favorable" outcome.
Statistical analysis was performed using the SPSS 20 (IBM, Armonk, NY, USA). The relationships between NPi and other parameters (GCS, ICP, manual exam, illumination and age) were examined by comparing the mean value of each group. The differences between two groups were verified by t-test, and differences between more than three groups were verified by one-way ANOVA.
The area under the curve (AUC) was used to assess the ability of the pupillometer to predict a patient's outcome. This curve was plotted by MedCalc for Windows, version 11.6.0 (MedCalc Software, Mariakerke, Belgium).
The NPi was measured 1522 times on 117 patients using a pupillometer. The characteristics of patient group according to prognosis (poor or favorable) is shown in Table 1. The mean values of NPi in "fixed", "sluggish", and "prompt" pupils were 0.21±0.85, 1.79±1.58, and 3.86±1.10, respectively. The mean values of NPi in the groups categorized by GCS 3 to 5, 6 to 8, 9 to 12, and 13 to 15 were 1.36±1.78, 2.68±1.64, 3.65±1.27, and 4.06± 1.76, respectively (p<0.001). The GCS can be said to have a directly proportional relationship with the NPi (Fig. 2). The mean NPi in the group with ICP higher than 30 cm H2O was 1.02±1.35, which was lower than that in the group with ICP lower than 30 cm H2O (3.26±0.64) (Fig. 3). In the one-way ANOVA analysis, NPi and ICP showed less of a relationship when ICP was lower than 30 cm H2O, but when ICP was higher than 30 cm H2O, NPi was significantly decreased.
The mean NPi value during the daytime was 4.03±1.02, whereas the value was 3.83±1.17 at night (p=0.123). The mean NPi value in the young age group was 3.92±1.10, whereas in the older age group it was 4.09±0.96 (p=0.078). These values were not statistically different, and it can be said that the NPi value was not influenced by age or the intensity of illumination.
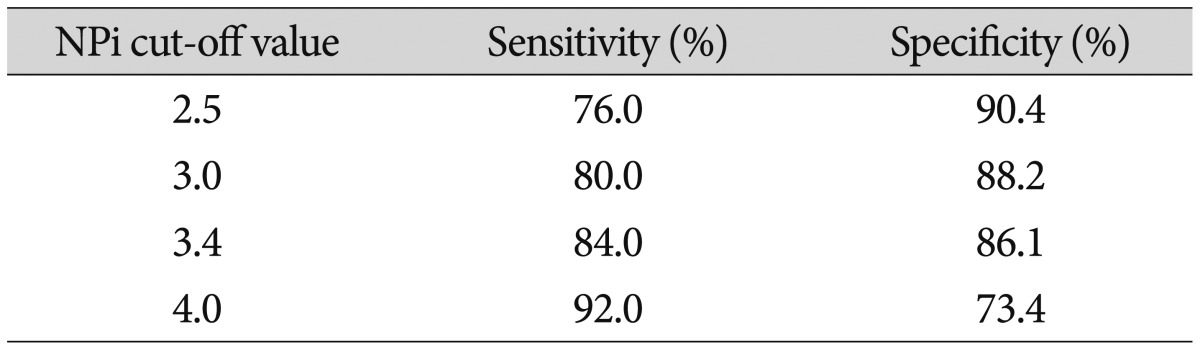
The mean initial NPi value of the "poor" prognosis group was 0.88±1.68, whereas that of the "favorable" prognosis group was 3.89±0.97. This difference was statistically significant (p=0.001). To evaluate the cut-off value of the NPi in terms of predicting clinical outcomes, we used the ROC curve (Fig. 4) and made a cross-division table by changing the presumed cut-off value from 2.5 to 4.0 (Table 2). In our study, an NPi value showed the AUC of 0.92, and the initial NPi value of the automated pupillometer had a sensitivity of 86.0% and a specificity of 84.6% in predicting the clinical outcome at 1 month after the event when cut-off value was 3.4.
PLR, estimated manually by inspectors using a light source, is used for the evaluation of patients in various clinical situations. However, results from this procedure include a number of inconsistencies and inaccuracies due to its inherently subjective nature419). According to Larson and Muhiudeen11), a routine clinical examination, performed with a traditional penlight, is unable to detect the PLR when the amplitude is less than 0.3 mm11). In several reports comparing manual exams to the use of automated pupilometers, automated pupillometers have been reported to reduce these inaccuracies81319). Meeker et al.12) reported that inter-examiner disagreement regarding the pupillary reaction was 39% for manual examinations compared with 1% for automated pupillometers. Hence, studies to define the relationship between clinical manifestations and PLR determined by automated pupillometer have been conducted in various fields125679151718) .
In the field of ophthalmology, the automated pupillometer has been applied to evaluate the feasibility of differentiating diabetic neuropathies, optic neuritis, relative afferent pupillary defects or glaucoma25915). Some studies have shown that pupillometers detect decreased optic nerve function in experimental optic neuritis, even in the absence of histological detection.15) In emergency medicine, research revealed that the presence of PLR, determined by automated pupillometer in patients with "fixed" pupils according to manual examinations, could be associated with early survival and a favorable neurological status in the recovery period11). Automated pupillometers were also used to assess the prognosis of patients receiving a liver transplantation18). Some anesthesiologists and pharmacologists have shown that automated pupillometers could be used to quantify the PLR, which can be affected by drugs and hence can provide proper information about the responses to these drugs6917). Some reported that there was an association between total opioid dose (expressed as morphine equivalents) and pupil diameter. These previous studies in various fields confirm that the automated pupillometer has the advantages of being non-invasive and objective compared to manual pupillary examinations.
PLR is a very important factor that is used to assess neurosurgical patients. Because pupillomotor fibers and parasympathetic oculomotor nuclei in the midbrain are sensitive to brainstem compression by mass-occupying lesions or ischemia, changes in the PLR can indicate an expanding supra-tentorial mass lesion with transmission of the associated pressure and subsequent onset of herniation. Previous reports have provide a large amount of evidence showing that alterations in the pupil light reflex, the size of the pupil, or anisocoria are all closely correlated with outcomes following an acute brain injury316). Therefore, PLR may serve as a guide for neurosurgeons in deciding the need for a further, aggressive work-up or a prompt surgical intervention3416). This was observed in patients with dilated pupils and is of clinical importance because most urgent decisions regarding the management of patients with abnormal pupils are made when the pupils are dilated and are therefore the most susceptible to error in a manual examination1113). Many reports have shown that automated pupillometers can detect PLR in pupils that were regarded as "fixed" in a manual exam10111319). In particular, some studies using pupillometers present NPi as an objective index that reflects the pupillary light reflex49). Some dynamic studies have reported that changes in the NPi reflect increases in intracranial pressure approximately 16 hours in advance. Decreased PLR velocity was recovered after surgical intervention in these patients3416).
In our study, the GCS correlated well with the NPi value, especially in severe brain injury patients with a GCS 8 or lower. Low NPi values represented increased ICP when ICP was higher than 30 cm H2O, but NPi values did not correlate with ICP values lower than 30 cm H2O. These results are in agreement with a previous study that showed that constriction velocities in the pupil did not fall until ICP increased above 30 mmHg16). Pupils assessed as "fixed" or "sluggish" in a manual pupillary exam showed variable NPi values, whereas a "prompt" assessment in a manual pupillary exam almost always had an NPi value above 3. This suggests that slight reflexes may have been ignored in manual pupillary exams.
This is the first study to evaluate the utility of automated pupillometers in predicting clinical outcomes in patients with acute brain lesions. Our results confirmed a definite difference in the initial NPi values between "poor" and "favorable" groups and indicated that an initial NPi value of 3.4, which has a specificity of 84.2% and a sensitivity of 86.0%, could be used as a cut-off value when predicting clinical outcomes.
Our study has some limitations. First, we did not consider dynamic factors such as delayed clinical deteriorations or neuro-surgical interventions in the evaluation of outcome prediction. These dynamic factors could be postulated to be the cause of less than 90 percent of the sensitivity and specificity of the automated pupillometers used in our study. Future studies will be required to ascertain how dynamic changes in NPi correlate with alterations in clinical conditions. Second, the effects of drug interactions, such as sedatives and other confounding drugs, have not been taken into consideration. However, we observed a tendency towards a slower drop in the NPi value in the pupils of these patients compared to the manual pupillary examination results, which were already recorded as "sluggish" or "fixed" after coma therapy. This suggests that well-designed future studies could reveal a role for NPi values in monitoring patients under sedation or coma therapy.
References
1. Behrends M, Niemann CU, Larson MD. Infrared pupillometry to detect the light reflex during cardiopulmonary resuscitation : a case series. Resuscitation. 2012; 83:1223–1228. PMID: 22659054.

2. Chang DS, Arora KS, Boland MV, Supakontanasan W, Friedman DS. Development and validation of an associative model for the detection of glaucoma using pupillography. Am J Ophthalmol. 2013; 156:1285–1296.e2. PMID: 24011523.

3. Chen JW, Gombart ZJ, Rogers S, Gardiner SK, Cecil S, Bullock RM. Pupillary reactivity as an early indicator of increased intracranial pressure : the introduction of the Neurological Pupil index. Surg Neurol Int. 2011; 2:82. PMID: 21748035.

4. Chen JW, Vakil-Gilani K, Williamson KL, Cecil S. Infrared pupillometry, the Neurological Pupil index and unilateral pupillary dilation after traumatic brain injury : implications for treatment paradigms. Springerplus. 2014; 3:548. PMID: 25332854.
5. Cohen LM, Rosenberg MA, Tanna AP, Volpe NJ. A novel computerized portable pupillometer detects and quantifies relative afferent pupillary defects. Curr Eye Res. 2015; 40:1120–1127. PMID: 25658805.

6. Connelly MA, Brown JT, Kearns GL, Anderson RA, St Peter SD, Neville KA. Pupillometry : a non-invasive technique for pain assessment in paediatric patients. Arch Dis Child. 2014; 99:1125–1131. PMID: 25187497.

7. Fletcher GC, Asbury AJ, Brown JH. Pupil changes during cardiopulmonary bypass. Br J Anaesth. 1996; 76:20–22. PMID: 8672373.

8. Hults KN, Knowlton SL, Oliver JW, Wolfson T, Gamst A. A study of pupillary assessment in outpatient neurosurgical clinics. J Neurosci Nurs. 2006; 38:447–452. PMID: 17233516.

9. Kim J, Heo J, Ji D, Kim MS. Quantitative assessment of pupillary light reflex in normal and anesthetized dogs : a preliminary study. J Vet Med Sci. 2015; 77:475–478. PMID: 25648149.

10. Kramer CL, Rabinstein AA, Wijdicks EF, Hocker SE. Neurologist versus machine : is the pupillometer better than the naked eye in detecting pupillary reactivity. Neurocrit Care. 2014; 21:309–311. PMID: 24865269.

11. Larson MD, Muhiudeen I. Pupillometric analysis of the 'absent light reflex'. Arch Neurol. 1995; 52:369–372. PMID: 7710372.

12. Marmarou A, Lu J, Butcher I, McHugh GS, Murray GD, Steyerberg EW, et al. Prognostic value of the Glasgow Coma Scale and pupil reactivity in traumatic brain injury assessed pre-hospital and on enrollment : an IMPACT analysis. J Neurotrauma. 2007; 24:270–280. PMID: 17375991.

13. Meeker M, Du R, Bacchetti P, Privitera CM, Larson MD, Holland MC, et al. Pupil examination : validity and clinical utility of an automated pupillometer. J Neurosci Nurs. 2005; 37:34–40. PMID: 15794443.
14. Narayan RK, Greenberg RP, Miller JD, Enas GG, Choi SC, Kishore PR, et al. Improved confidence of outcome prediction in severe head injury. A comparative analysis of the clinical examination, multimodality evoked potentials, CT scanning, and intracranial pressure. J Neurosurg. 1981; 54:751–762. PMID: 7241184.
15. Shindler KS, Revere K, Dutt M, Ying GS, Chung DC. In vivo detection of experimental optic neuritis by pupillometry. Exp Eye Res. 2012; 100:1–6. PMID: 22561341.
16. Taylor WR, Chen JW, Meltzer H, Gennarelli TA, Kelbch C, Knowlton S, et al. Quantitative pupillometry, a new technology : normative data and preliminary observations in patients with acute head injury. Technical note. J Neurosurg. 2003; 98:205–213. PMID: 12546375.

17. Theodossiadis PG, Achtsidis V, Theodoropoulou S, Tentolouris N, Komninos C, Fountas KN. The effect of alpha antagonists on pupil dynamics : implications for the diagnosis of intraoperative floppy iris syndrome. Am J Ophthalmol. 2012; 153:620–626. PMID: 22265152.

18. Yan S, Tu Z, Lu W, Zhang Q, He J, Li Z, et al. Clinical utility of an automated pupillometer for assessing and monitoring recipients of liver transplantation. Liver Transpl. 2009; 15:1718–1727. PMID: 19938127.

19. Yoon MK, Schmidt G, Lietman T, McLeod SD. Inter- and intraobserver reliability of pupil diameter measurement during 24 hours using the Colvard pupillometer. J Refract Surg. 2007; 23:266–271. PMID: 17385292.

Fig. 1
A : The shape of portable pupillometer. B : The display of pupillometer. MAX means the maximum pupil diameter before constriction. MIN means the pupil diameter at the peak of constriction. %CH means the percent of the change (MAX-MIN)/MAX. LAT means the latency and it represents the time of the onset of the constriction. CV, MCV means the average and the maximum constriction velocity. DV means the dilation velocity. The graph below the table depicts change of size of pupil according to change of time.

Fig. 2
The graph presents the mean value of the Neurologic Pupillary index (NPi) in four groups divided according to the Glasgow Coma Scale (GCS). The NPi value tends to decrease as the GCS decreases, especially in the "poor" clinical group with a GCS of 3 to 5.
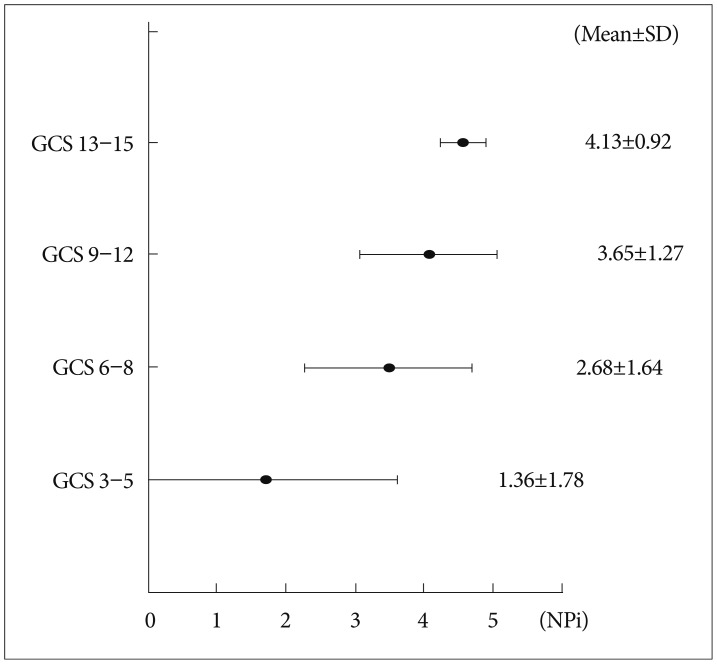
Fig. 3
There is no relationship between NPi and ICP when ICP is lower than 30 cm H2O. However, the NPi value significantly decreased when ICP was higher than 30 cm H2O. NPi : Neurologic Pupillary index, ICP : intracranial pressure.

Fig. 4
The closer the curve to the left upper angular point, the more reliable the test becomes. This ROC curve shows the AUC of 0.92, and both sensitivity and specificity are optimal when the NPi cut-off value is 3.4 (starred dot). ROC : receiver operating characteristic, AUC : area under the curve, NPi : Neurologic Pupillary index.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download