Abstract
Objective
To measure the orientation of the facet joints of cervical spine (C-spine) segments in the sagittal plane, known as the pedicle-facet (P-F) angle, and to use these measurements to evaluate the relationship between the P-F angle and the amount of vertebral anterolisthesis in patients with degenerative cervical spondylolisthesis (DCS).
Methods
A retrospective case-control study was performed including 30 age- and sex-matched patients with DCS and 30 control participants. Anterior-posterior and lateral view radiographs of the C-spine were obtained in a standing position. The P-F angle at all cervical levels and the amount of anterolisthesis at C4-5 were measured from lateral view plain radiographs.
Results
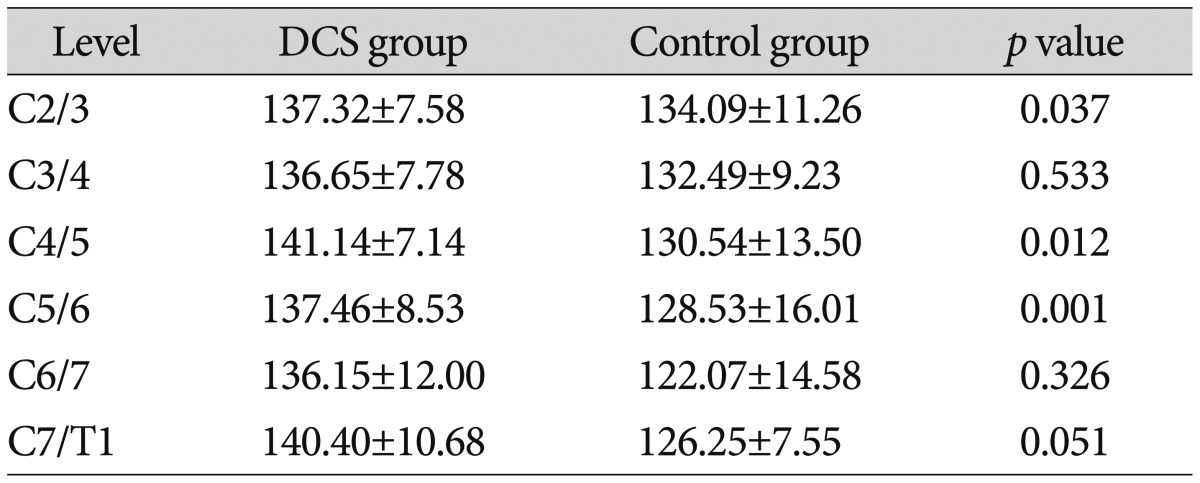
The P-F angles at C4-5 were 141.14±7.14° for the DCS group and 130.53±13.50° (p=0.012) for the control group, and at C5-6 were 137.46±8.53° for the DCS group and 128.53±16.01° for the control group (p=0.001). The mean P-F angle at C4-5 did not correlate with the amount of anterolisthesis (p=0.483). The amount of anterior slippage did correlate with age (p<0.001).
Conclusion
The P-F angle was intrinsically higher at C4-5, compared to C5-6, in both the DCS and control groups, which might explain the increased likelihood for anterolisthesis of C4. Higher P-F angles in the DCS group may be a predisposing factor to slippage. The P-F angle may interact with age to increase incidence of anterolisthesis with increasing age.
Degenerative cervical spondylolisthesis (DCS) is a pathological condition defined by anterolisthesis or anterior slippage of the cervical spine (C-spine) vertebrae. Underlying causes of this slippage include application of a shear force on the vertebra, disc degeneration, and/or hypertrophic arthropathy of the facet joint311172123). While DCS is less prevalent than spondylolisthesis at the lumbar spine, it still has an estimated prevalence of 5.2% to 11%, most commonly involving the C3-4 and C4-5 levels of the C-spine 111721). In contrast to the abundant literature on degenerative lumbar spondylolisthesis, DCS has been evaluated in only a few studies. Several predisposing factors have been reported to contribute to the development of spondylolisthesis at the lumbar spine, among which facet joint orientation is thought to play an important role181920). Gao et al.6) reported the orientation of the facet joint along the sagittal plane, known as the pedicle-facet (P-F) angle, which they measured on lateral view computed tomography (CT) scans, to be the highest intrinsically at L4-5, both in patients with lumbar spondylolisthesis and in participants in their control group. They hypothesized that a more horizontal orientation of the L4-5 facet joint (i.e., a higher sagittal plane angle) may be a predisposing anatomical factor for spondylolisthesis. However, the characteristic changes in P-F angle at the C-spine have not been well described to date.
The balance of the C-spine along the sagittal plane, in relation to the sagittal plane position of the pelvis, is increasingly being recognized as an important predisposing factor for spondylolisthesis. This sagittal plane balance is captured by the slope of the first thoracic vertebra (T1)1016). Jun et al.8) reported a greater T1 slope in patients with DCS. Therefore, we hypothesized that a high T1 slope, indicative of a loss of alignment of the spine in the sagittal plane, may be a predisposing factor for the development of DCS, increasing the magnitude of anterior shear force along the gravitational vector22). Furthermore, this chronic anterior shear force could concurrently lead to arthrotic changes of the posterior facets, which would accelerate disc degeneration and disc collapse. To the best of our knowledge, differences in P-F angle between patients with DCS and normal controls have not been specifically addressed in research. Therefore, the main objectives of this study were to compare the P-F angles, measured on simple radiographs, between patients with DCS and a control group matched on sex and age, and to evaluate the relationship between the P-F angle and the amount of vertebral anterolisthesis in patients with DCS.
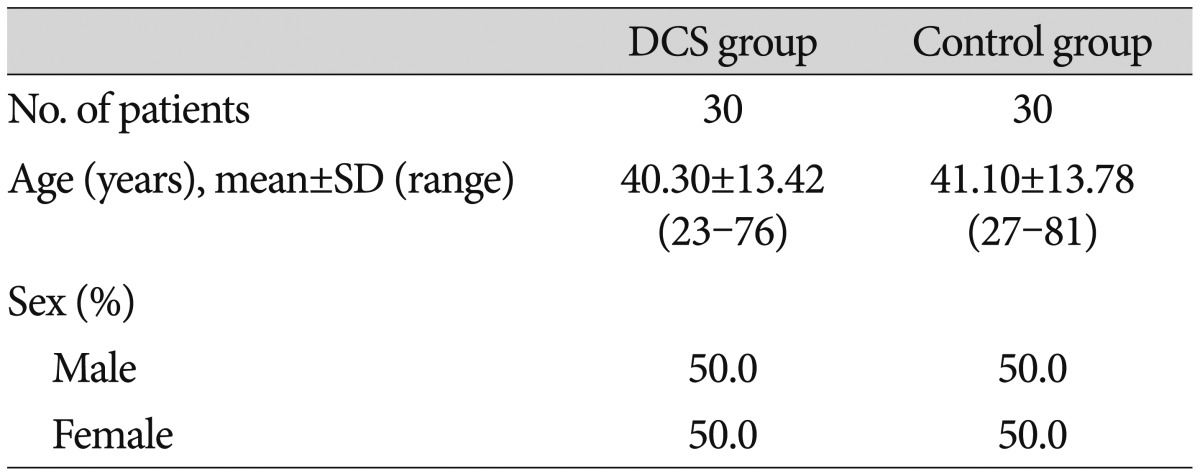
Patients with DCS were identified retrospectively from the total group of patients who attended the spine center in our institution between June 2002 and December 2012. During this period, 983 patients received plain radiographs to inform various diagnoses, such as neck pain and cervical radiculopathy. Patients with non-degenerative cervical disease-trauma, infection, tumor, deformity, and inflammatory diseases-or prior cervical spine surgery were excluded. Plain anterior-posterior and lateral view radiographs had been obtained with patients in a relaxed standing position, with the upper extremities positioned naturally at the side of the body and the head maintained in a neutral position, with horizontal gaze parallel to the Frankfurt horizontal plane. The radiographs were used to confirm a 7-segmental cervical spine and to rule-out developmental anomalies of the C-spine, signs of lytic lesions, and scoliotic deformity of >10°. Following screening for exclusion criteria, 30 adult patients with a diagnosis of DCS at C4-5, without evidence of DCS at any other level, consisting of 15 men and 15 women, with an average age of 40.30 years (range, 23-76 years), were included in the study.
The control group consisted of 30 adults, matched on sex and age with patients in the DCS group, identified by retrospective analysis of patients who had attended the ear, nose, throat out-patient department of our institution between January 2008 and September 2012, and who had received plain radiographs of the C-spine as part of their medical care. Patients in the control group had never been diagnosed with or treated for a spinal problem. The group included 15 men and 15 women, with an average age of 41.10 years (range, 27-81 years).
DCS was defined, using previously defined criteria, as an anterolisthesis (i.e., slip) of the vertebra of more than 2 mm 2112324). The extent of anterior slip of the vertebra was measured as the distance from the postero-inferior corner of the cranial (i.e., superior) vertebral body to the tangential line along the posterior border of caudal (i.e., lower) vertebral body (Fig. 1A). The P-F angle, calculated on lateral view radiographs, was formed by the intersection between a straight line connecting the midpoints of the anterior and posterior cortices of the vertebrae and a straight line positioned parallel to the facet joint (Fig. 1B).
Plain radiographs were saved in the Picture Archiving and Communication System (PView; INFINITT, Seoul, Korea) for analysis. The quality of radiographs for measurements of P-F angles and amount of anterolisthesis was ascertained by two independent observers. After agreement, the outcome variables were independently measured twice, by two spinal surgeons from the neurosurgery department. The Pearson's correlation coefficient between the two measures was calculated as an indicator of agreement. The association of P-F angles to group characteristics, namely age and sex, was evaluated using Pearson's correlation. Between-group differences in P-F angles were evaluated using independent-samples t-test. All statistical analyses were performed in SPSS, version 19.0 (IBM SPSS, Armonk, NY, USA), with p<0.05 considered to be significant.
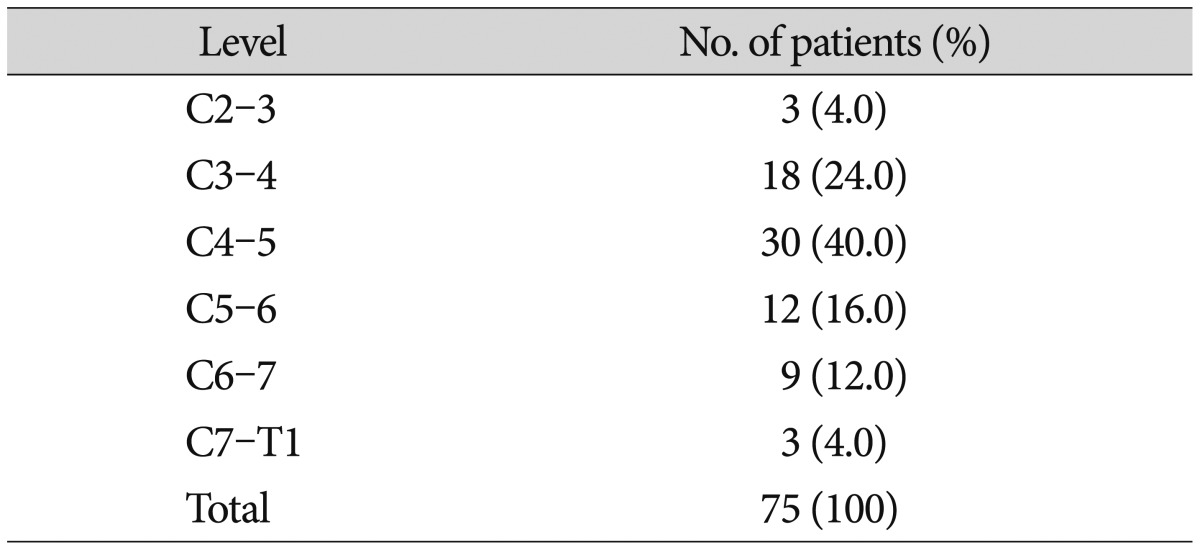
Of our prospective group of 983 patients, 30 patients were diagnosed with anterolisthesis of the C-spine (3.05%). The descriptive characteristics of these patients are summarized in Table 1. The distribution of DCS by level is reported in Table 2.
The mean P-F angle values and amount of anterolisthesis, for the DCS and control groups, are reported in Table 3. The P-F angles at C4-5 were 141.14±7.14° for the DCS group and 130.54±13.50° for the control group (p=0.012). In comparison, at C5-6, the P-F angles were 137.46±8.53° and 128.53±16.01°, respectively (p=0.001). At C2-3, the P-F angles were 137.32±7.58° and 134.09±11.26°, respectively (p=0.037). However, there were no significant between-group differences in P-F angles at C3-4, C6-7, or C7-T1 levels (p≥0.051).
The mean amount of anterolisthesis in the DCS group was 2.81±0.15 mm. Age was significantly correlated with the amount of vertebral slipping in the DCS group (r=0.649, p<0.001). No significant correlation was found between any other parameters. With a linear regression analysis, statistically significant linear regression models were established by using the following formula :
The incidence of lumbar degenerative spondylolisthesis is reported to be 19.7%9). Degenerative spondylolisthesis is more rarely seen in the cervical spine. Since Lee et al.13) first reported differences in radiological findings between traumatic and degenerative listhesis of the C-spine in 1986, an overall prevalence of DCS of 5.2% to 11% has been reported. The incidence rate in our study was comparable, with DCS diagnosed in 30 of the 983 prospective participants, a prevalence of 7.64%. DCS has been reported to be most common at the C3-4 and C4-5 levels of the C-spine5711). The distribution was comparable in our study group, with evidence of DCS at C3-4 level in 18 patients (24.0%) and at C4-5 in 30 patients (40.0%).
The main cause of degenerative lumbar spondylolisthesis is disc degeneration and facet joint arthrosis. However, at the C-spine, trauma may be the most common cause of an anterior displacement of one vertebral body relative to the subjacent one. Injuries that lead to this deformity include traumatic spondylolisthesis of the axis, facet dislocation, and facet fracture/subluxation14). This anterior displacement causes progressive hypertrophic arthropathy of the facet joints, which results in joint erosions, marginal osteophyte formation, and subluxation. The secondary loss of motion, or ankylosis, between vertebral segments diminishes the mobility of the C-spine, thus increasing the stress on the adjacent discs and facets, especially during flexion and extension motions of the C-spine. The increased stress may stretch the disc and ligaments, allowing slippage to occur12).
Dean et al.5) described two types of DCS. The first type, which is more common, occurs adjacent to a relatively stiffer spondylotic segment, which is in the transition zone from stiff to more mobile segments of the spine. Considering this possible underlying pathomechanism, 'compensatory subluxation' could be a more accurate term for this type of DCS. Although disc degeneration is present in this compensatory type of anterolisthesis to some extent, the disc degeneration is radiographically and pathologically less in magnitude than in the adjacent levels with more advanced spondylosis. However, this type of spondylolisthesis is associated with osteoarthritic changes of the facet joints, including erosion, joint remodeling, and subluxation. The second type of spondylolisthesis occurs within spondylotic segments of the C-spine because of advanced disc degeneration. In comparison to Dean et al.5) classification, Woiciechowsky et al.24) classified DCS into three types : spondylolisthesis with degeneration of the facet joints; spondylolisthesis with degeneration of the facet joints and vertebral bodies; and spondylolisthesis with severe C-spine deformity. Woiciechowsky et al.24) classification is oriented toward clinical practice, being based on the assumption that degeneration of the disc and the facet joints occurs first and leads to the associated segmental instability and neck pain characteristic of DCS. However, the pathomechanism of DCS remains yet to be fully clarified.
In our study, we specifically evaluated C4-5 based on reports of the highest prevalence of DCS at this level. The highest incidence of DCS in our study group was found at the C3-4 and C4-5 levels, which is comparable to findings from several other studies2571117). Several hypotheses have been advanced to explain the higher likelihood for the development of DCS at C4-5. A number of studies have related the incidence of DCS to the relative hypermobility of the C4-5 vertebral segment, with repeated movements leading to relaxation of surrounding ligaments and, progressively, to degenerative articular changes 14610). At the lumbar spine, Nagaosa et al.15) argued that an increase in the P-F angle is a pathoanatomical risk factor for the development of degenerative spondylolisthesis. Supporting this argument, Gao et al.6) confirmed that the P-F angle was significantly larger at L4-5 in patients with degenerative spondylolisthesis compared to a control group, and that the P-F angle of the slipped vertebra was more horizontally inclined6). Our results confirmed similar findings for the C-spine, with the P-F angle being significantly larger at C4-5 in the DCS group compared to the control group. However, the mean P-F angle at the C4-5 level did not correlate with the amount of anterior slipping of the C4 vertebra; only patients' age was statistically correlated to the amount of vertebral slipping (r=0.649, p<0.001).
The limitations of our study must be acknowledged in the interpretation of results. Due to our small sample size, the characteristics of the DCS patients, and the fact that all patients were recruited from a single institution, our study group is not representative of the entire population of patients with DCS. As an example, our study did not include patients with DCS who were symptom-free. There is evidence that neck pain may in fact be the main presenting symptom of DCS7). Although we did not specifically assess neck pain in our study, more than half of the patients in our DCS group reported neck or occipital pain7). We did not consider the degree of intervertebral disc degeneration, the muscles involved in the cervical spine kinematics, or the vertebral body height in our population. In addition, we did not evaluate the relationships between the P-F angle and the amount of anterolisthesis or other factors, such as clinical manifestations, disc degeneration, and body mass index, in patients with DCS. Therefore, further research using larger patient populations may help to more comprehensively explain the risk factors for DCS. We do acknowledge, as well, that the guiding hypothesis for our research is based on previous research of the lumbar spine, which itself presents unresolved issues regarding the interaction between anatomical features, or tropism, of facet joints and the degenerative process of spondylolisthesis. Dai4) suggested that facet joint tropism was a predisposing factor to the development of disc degeneration and subsequent spondylolisthesis; however, Berlemann et al.1) argued against this functional relationship4). In our study, we used simple radiographs, which did not allow us to evaluate the relationship between facet joint tropism and the degenerative process of spondylolisthesis at the C-spine. The influence of anterolisthesis on clinical symptoms was also not specifically evaluated, and therefore we cannot comment on the relationship between the amount of slippage and symptomology.
The P-F angle was the largest at the C4-5 level in the DCS group, which might explain the predisposition of C4 to slip forward. The mean P-F angle at the C4-5 level did not correlate to the amount of vertebral slipping of C4 in DCS patients. Only age was statistically correlated with the amount of vertebral slipping.
References
1. Berlemann U, Jeszenszky DJ, Bühler DW, Harms J. Facet joint remodeling in degenerative spondylolisthesis : an investigation of joint orientation and tropism. Eur Spine J. 1998; 7:376–380. PMID: 9840470.

2. Boulos AS, Lovely TJ. Degenerative cervical spondylolisthesis : diagnosis and management in five cases. J Spinal Disord. 1996; 9:241–245. PMID: 8854280.
3. Chen J, Solinger AB, Poncet JF, Lantz CA. Meta-analysis of normative cervical motion. Spine (Phila Pa 1976). 1999; 24:1571–1578. PMID: 10457577.

4. Dai LY. Orientation and tropism of lumbar facet joints in degenerative spondylolisthesis. Int Orthop. 2001; 25:40–42. PMID: 11374266.

5. Dean CL, Gabriel JP, Cassinelli EH, Bolesta MJ, Bohlman HH. Degenerative spondylolisthesis of the cervical spine : analysis of 58 patients treated with anterior cervical decompression and fusion. Spine J. 2009; 9:439–446. PMID: 19111509.

6. Gao F, Hou D, Zhao B, Sun X, Sun H, Li N, et al. The pedicle-facet angle and tropism in the sagittal plane in degenerative spondylolisthesis : a computed tomography study using multiplanar reformations techniques. J Spinal Disord Tech. 2012; 25:E18–E22. PMID: 22052206.
7. Jiang SD, Jiang LS, Dai LY. Degenerative cervical spondylolisthesis : a systematic review. Int Orthop. 2011; 35:869–875. PMID: 21264670.
8. Jun HS, Chang IB, Song JH, Kim TH, Park MS, Kim SW, et al. Is it possible to evaluate the parameters of cervical sagittal alignment on cervical computed tomographic scans? Spine (Phila Pa 1976). 2014; 39:E630–E636. PMID: 24776700.

9. Kauppila LI, Eustace S, Kiel DP, Felson DT, Wright AM. Degenerative displacement of lumbar vertebrae A 25-year follow-up study in Framingham. Spine (Phila Pa 1976). 1998; 23:1868–1873. discussion 1873-1874PMID: 9762744.
10. Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010; 10:994–998. PMID: 20970739.

11. Kopacz KJ, Connolly PJ. The prevalence of cervical spondylolisthesis. Orthopedics. 1999; 22:677–679. PMID: 10418863.
12. Lee C, Woodring JH, Rogers LF, Kim KS. The radiographic distinction of degenerative slippage (spondylolisthesis and retrolisthesis) from traumatic slippage of the cervical spine. Skeletal Radiol. 1986; 15:439–443. PMID: 3764470.

13. Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012; 25:E41–E47. PMID: 22037167.

14. Li XF, Dai LY, Lu H, Chen XD. A systematic review of the management of hangman's fractures. Eur Spine J. 2006; 15:257–269. PMID: 16235100.

15. Nagaosa Y, Kikuchi S, Hasue M, Sato S. Pathoanatomic mechanisms of degenerative spondylolisthesis A radiographic study. Spine (Phila Pa 1976). 1998; 23:1447–1451. PMID: 9670395.
16. Park JH, Cho CB, Song JH, Kim SW, Ha Y, Oh JK. T1 slope and cervical sagittal alignment on cervical CT radiographs of asymptomatic persons. J Korean Neurosurg Soc. 2013; 53:356–359. PMID: 24003370.

17. Park MS, Moon SH, Lee HM, Kim SW, Kim TH, Suh BK, et al. The natural history of degenerative spondylolisthesis of the cervical spine with 2- to 7-year follow-up. Spine (Phila Pa 1976). 2013; 38:E205–E210. PMID: 23169076.

18. Rosenberg NJ. Degenerative spondylolisthesis. Predisposing factors. J Bone Joint Surg Am. 1975; 57:467–474. PMID: 1141255.

19. Sanderson PL, Fraser RD. The influence of pregnancy on the development of degenerative spondylolisthesis. J Bone Joint Surg Br. 1996; 78:951–954. PMID: 8951013.

20. Sato K, Wakamatsu E, Yoshizumi A, Watanabe N, Irei O. The configuration of the laminas and facet joints in degenerative spondylolisthesis A clinicoradiologic study. Spine (Phila Pa 1976). 1989; 14:1265–1271. PMID: 2603062.

21. Shigematsu H, Ueda Y, Takeshima T, Koizumi M, Satoh N, Matsumori H, et al. Degenerative spondylolisthesis does not influence surgical results of laminoplasty in elderly cervical spondylotic myelopathy patients. Eur Spine J. 2010; 19:720–725. PMID: 20191294.

22. Suzuki A, Daubs MD, Inoue H, Hayashi T, Aghdasi B, Montgomery SR, et al. Prevalence and motion characteristics of degenerative cervical spondylolisthesis in the symptomatic adult. Spine (Phila Pa 1976). 2013; 38:E1115–E1120. PMID: 23680839.

23. Tani T, Kawasaki M, Taniguchi S, Ushida T. Functional importance of degenerative spondylolisthesis in cervical spondylotic myelopathy in the elderly. Spine (Phila Pa 1976). 2003; 28:1128–1134. PMID: 12782980.

24. Woiciechowsky C, Thomale UW, Kroppenstedt SN. Degenerative spondylolisthesis of the cervical spine--symptoms and surgical strategies depending on disease progress. Eur Spine J. 2004; 13:680–684. PMID: 15221569.

Fig. 1
A : Lateral radiograph of the cervical spine shows spondylolisthesis at C4-5; horizontal displacement between C4 and C5. B : The pedicle-facet (P-F) angle was defined by the intersection of a straight line connecting the midpoints of the anterior and posterior vertebral cortices and a straight line positioned parallel to the facet joint in the lateral view radiograph (α : the P-F angle).





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download