Abstract
Tentorial dural arteriovenous fistula (DAVF) is a rare vascular disease, which has high risk of intracranial hemorrhage. We present two cases of tentorial DAVF which were successfully treated with single trial of transarterial embolization using Onyx. We briefly reviewed the types of the tentorial DAVF and strategies of treatment.
Intracranial dural arteriovenous fistula (DAVF) is abnormal arteriovenous shunts that occur within the leaflets of the dura mater and comprised 10-15% of intracranial arteriovenous malformation8). In a meta-analysis of 377 patients with DAVF reported before 1989, tentorial DAVF was only 8% (32/ 377) of all intracranial DAVF, but tentorial DAVF had the most aggressive neurological behavior, with 97% (31/32) causing hemorrhage or progressive focal neurological deficits110). Unlike the less aggressive DAVFs of the lateral and cavernous sinuses that drain into venous sinuses, tentorial DAVF drains into pial veins11). These characteristics cause tentorial DAVF prone to hemorrhage. We report two cases of tentorial DAVF treated by transarterial embolization using Onyx.
A 59-year-old man presented with sudden onset of dizziness and gait disturbance. He complains of right hemiparesis and diplopia. He also showed spontaneous vertical nystagmus. He was diagnosed diabetes and hypertension for the first time after admission. CT and MR imaging revealed an acute hemorrhage at left tectum of mid brain and fourth ventricle (Fig. 1A, B, C). Cerebral angiography showed a DAVF around torcular fed by meningeal branch of ascending pharyngeal artery, transosseus branch of the right occipital artery and drained into cortical vein of left occiput and basal vein of Rosenthal (Fig. 1D, E). Transarterial embolization was performed under general anesthesia. An intravenous bolus of 3000 IU of heparin was administered after placement of a 6-Fr guiding sheath in the right femoral artery. A 6-Fr guiding catheter (Envoy, Cordis Endovascular, Miami Lakes, FL, USA) was placed at external carotid artery. We planned to superselective catheterization of meningeal branch of ascending pharyngeal artery but failed due to tortous curve at cranial base. We could access to fistula point through transosseus branch of occipital artery using microcatheter (Apollo, ev3 Inc., Plymouth, MN, USA). The volume of 0.7 mL Onyx-18 (ethyl vinyl alcohol, ev3 Inc., Irvine, CA, USA) was injected within DAVF with biplanar simultaneous subtracted fluoroscopy. Post-embolization angiogram demonstrated Onyx occupying the retrograde drainage of cortical vein and obliteration of DAVF (Fig. 1F, G, H). Microcatheter was gently removed. The patient was discharged 7 days later and his postoperative course was uneventful.
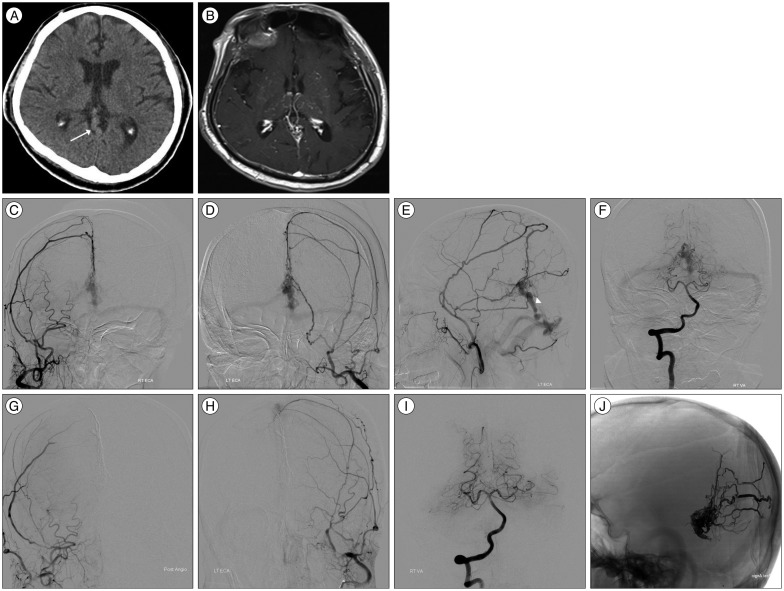
A 74-year-old man presented with progressive headache and dementia symptom for several months. Seven years ago, he had spontaneous hemorrhage in 4th ventricular and been treated for DAVF by transarterial embolization using n-butyl cyanoacrylate (NBCA). Both middle meningeal arteries (using 33 and 50% glue) and transosseus branch of left occipital artery (using 20% glue) were selected for embolization. The posterior choroidal branch of vertebral artery was not embolized due to risk. Although arteriovenous shunting flow was not completely abolished, retrograde cortical flow was remarkably decreased. He refused further treatment and did not seek hospital since then. By this time of visit, he has been well. CT and MR image showed a prominent, tortous vascular structure around medial tentorium and multiple fine vessels engorgements at both thalamic and putamen areas (Fig. 2A, B). Angiogram demonstrated recanalization and recruitment from both middle meningeal arteries and posterior choroidal arterial supply from vertebral artery. The retrograde leptomeningeal drain of infratentorial vermian vein showed dilated and saccular change (Fig. 2C-F). We embolized DAVF only through the right middle meningeal artery and inject Onyx-18 1.0 mg as described above. Multiple fistula points and common draining vein was occluded (Fig. 2G-J). Korea Mini-Mental State Examination (K-MMSE) score was improved from 14 to 28. He was discharged 7 days later with improved condition.
DAVF associated with retrograde leptomeningeal venous drainage exhibit a high incidence of aggressive behavior3912) and those with only leptomeningeal venous drainage was classified type III by Borden et al.2). In tentorial DAVF patients, 22/22 cases (100%)14), 26/31 cases (84%)10) and 13/14 cases (93%)6) were classified Borden type III and needed prompt treatment. The tentorial DAVF is a rare type of DVAF and should be treated even though without remarkable clinical symptoms because natural history is very disappointing. To our knowledge, there has been no report of tentorial DAVF which is resolved spontaneously yet. Tentorial DAVF is located in the tentorial dura mater and fed primarily from branches of the meningohypophyseal trunk, middle meningeal arteries, and occipital artery. The multitude of small dural arteries, a variety of venous pathways, and high flow may prevent spontaneous closure11). DAVF usually has multiple fistula points by multiple feeding arteries but drains into single vein. The aim of the DAVF treatment with retrograde leptomeningeal venous drainage is complete and permanent obliteration of the all arterial supply or occlusion of proximal draining vein. Therapeutic options for treating DAVF include transvenous and/or transarterial embolization and surgical excision of the DAVF nidus, ligation of the draining vein. Usually the transvenous embolization was preferred when the venous anatomic features were open and not too tortuous for catheterization of the draining vein and fistula13). These combinations of transvenous and transarterial embolization results in high obliteration rates for most DAVF, but tentorial DAVF are somewhat different. Transvenous navigation to deeper locations around the tentorium is difficult. More importantly, tentorial DAVF often drain exclusively to subarachnoid veins rather than to their associated sinus (Borden Type III), which prevents transvenous access261011). Huang et al.6), reported complete cure of tentorial DAVF in 78.6% (11/14) by transarterial embolization using Onyx. In case of partial obliteration of the arterial supply, patients with Borden Type II or III lesions should considered surgery because they may experience temporary palliation of their symptoms but cannot provide protection from the risk of hemorrhage or progression of the effects of venous hypertension414). Hwang et al.7) and Lawton et al.10) recommended surgical option for incomplete embolization of tentorial DAVF by simple interruption of draining vein. Surgical interruption of simple venous drainage is analogous to transarterial and/or tranvenous embolization of outlet from the nidus without effect of normal venous drainage. The surgical interruption of proximal venous drain could be considered according to types of tentorial DAVF by location and drain vein.
The tentorial sinuses drain the supra- and infratentorial veins as well as the deep veins of the brain stem. Lasjaunias et al.9), divided tentorial DAVF into torcular, basal tentorium and marginal tentorium by their location and draining veins. Lesions in torcular drain to medial occipital and infratemporal areas. Lesions in basal tentorium drain to superior petrosal sinus and petrosal vein. Lesions in marginal tentorium drain into tentorial vein, vein of Rosenthal, and mesencephalic veins. Picard et al.12), divided tentorial DAVF to 3 groups by draining veins as medial, lateral and marginal tentorial sinus group. Lesions in the medial tentorial sinus group are situated adjacent to the torcular and drain into it or the lateral or straight sinus. They primarily receive venous drainage from the cerebellar hemispheres and vermis (infratentorial drainage). Lesions in the lateral tentorial sinus group lie adjacent to the lateral sinus and receive supratentorial drainage from the lateral and inferior surfaces of the temporal and occipital lobes. Lesions in the marginal tentorial sinus group lie along the free edge of the tentorium and receive venous drainage from the basilar and lateral mesencephalic veins. Fistulae at this location may have infra- or supratentorial drainage or drain into spinal veins. Lawton et al.10), differentiated these fistulae into 6 types (1. Galenic DAVF, 2. Straight sinus DAVF, 3. Torcular DAVF, 4. Tentorial sinus DAVF, 5. Superor petrosal sinus DAVF, 6. Incisural DAVF) and suggested surgical strategies on the basis of these types. Case 1 was torcular type by Lasjaunias et al.9) and Lawton et al.10), and then marginal tentorial sinus group by Picard et al.12) which was located around tocular area and drained to supratentorial cotical vein into basal vein of Rosenthal and causes brain stem hemorrhage. Case 2 was medial tentorial sinus group by Picard et al.12) and straight sinus type by Lawton et al.10) which was located around midline torcular and drained to infratentorial vermian vein and causes venous hypertension. In both cases transvenous approach was too difficult and risky for embolization. Various embolic agents have been used including particles, platinum coils, NBCA and Onyx for arterial approach. In case of NBCA, solidification time of the material should be matched to the local flow velocity and to the angioarchitectural features of the lesion. Although NBCA is usually considered as permanent embolic agent but may result in recanalization as our case in delayed fashion5). Furthemore posterior choroidal artery could not be selected for embolization of complete angiographic cure by NBCA. Recently due to the superior ability of penetration and controllability, Onyx is used as the treatment of choice for transarterial embolic agent of DAVF and very effective for obliteration of multiple fistula point and proximal draining vein by single transarterial access. Contrast to NBCA, in case 2, Onyx could penetrate deeper venous sac and reach posterior choroidal arterial supply from middle meningeal artery and results in complete angiographic cure.
Tentorial DAVF should be treated aggressively and transarterial embolization with Onyx can be prior option when transvenous access is difficult. Transarterial approach using Onyx also can be applied for delayed recanalization after embolization with NBCA. If partially treated tentorial DAVF by embolization procedure, simple surgical interruption of proximal draining vein should be considered according to the location and drain veins.
References
1. Awad IA, Little JR, Akarawi WP, Ahl J. Intracranial dural arteriovenous malformations : factors predisposing to an aggressive neurological course. J Neurosurg. 1990; 72:839–850. PMID: 2140125.

2. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995; 82:166–179. PMID: 7815143.

3. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas : clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995; 194:671–680. PMID: 7862961.

4. Davies MA, Ter Brugge K, Willinsky R, Wallace MC. The natural history and management of intracranial dural arteriovenous fistulae. Part 2 : aggressive lesions. Interv Neuroradiol. 1997; 3:303–311. PMID: 20678361.

5. Gruber A, Mazal PR, Bavinzski G, Killer M, Budka H, Richling B. Repermeation of partially embolized cerebral arteriovenous malformations : a clinical, radiologic, and histologic study. AJNR Am J Neuroradiol. 1996; 17:1323–1331. PMID: 8871719.
6. Huang Q, Xu Y, Hong B, Li Q, Zhao W, Liu J. Use of onyx in the management of tentorial dural arteriovenous fistulae. Neurosurgery. 2009; 65:287–292. discussion 292-293PMID: 19625907.

7. Hwang G, Kang HS, Oh CW, Kwon OK. Surgical obliteration in superior petrosal sinus dural arteriovenous fistula. J Korean Neurosurg Soc. 2011; 49:222–225. PMID: 21607180.

8. Jiang C, Lv X, Li Y, Zhang J, Wu Z. Endovascular treatment of high-risk tentorial dural arteriovenous fistulas : clinical outcomes. Neuroradiology. 2009; 51:103–111. PMID: 18989665.

9. Lasjaunias P, Chiu M, ter Brugge K, Tolia A, Hurth M, Bernstein M. Neurological manifestations of intracranial dural arteriovenous malformations. J Neurosurg. 1986; 64:724–730. PMID: 3701421.

10. Lawton MT, Sanchez-Mejia RO, Pham D, Tan J, Halbach VV. Tentorial dural arteriovenous fistulae : operative strategies and microsurgical results for six types. Neurosurgery. 2008; 62(3 Suppl 1):110–124. discussion 124-125PMID: 18424975.
11. Lewis AI, Tomsick TA, Tew JM Jr. Management of tentorial dural arteriovenous malformations : transarterial embolization combined with stereotactic radiation or surgery. J Neurosurg. 1994; 81:851–859. PMID: 7965115.

12. Picard L, Bracard S, Islak C, Roy D, Moreno A, Marchal JC, et al. Dural fistulae of the tentorium cerebelli. Radioanatomical, clinical and therapeutic considerations. J Neuroradiol. 1990; 17:161–181. PMID: 2286839.
13. Roy D, Raymond J. The role of transvenous embolization in the treatment of intracranial dural arteriovenous fistulas. Neurosurgery. 1997; 40:1133–1141. discussion 1141-1144PMID: 9179885.

14. Tomak PR, Cloft HJ, Kaga A, Cawley CM, Dion J, Barrow DL, et al. Evolution of the management of tentorial dural arteriovenous malformations. Neurosurgery. 2003; 52:750–760. discussion 760-762PMID: 12657170.

Fig. 1
Case 1. Brain CT (A) and MR imaging (B and C) showed acute hemorrhage at 4th ventricle and left tectum of mid brain. Enhanced axial MR imaging (C) showed prominent vessels near the perimesencephalic cistern and tentorial leaflet (white arrows). Right external carotid angiogram demonstrated a DAVF around torcular fed by meningeal branch of ascending pharyngeal artery, transosseus branch of the right occipital artery and drained into cortical vein of left occiput (black arrow) and basal vein of Rosenthal (D and E). Post-embolization angiogram demonstrated Onyx occupying the retrograde drainage of cortical vein and obliteration of DAVF. Onyx was injected through the transosseus branch of the right occipital artery (arrowhead) (F and G : Right external carotid angiogram. H : Skull AP view).
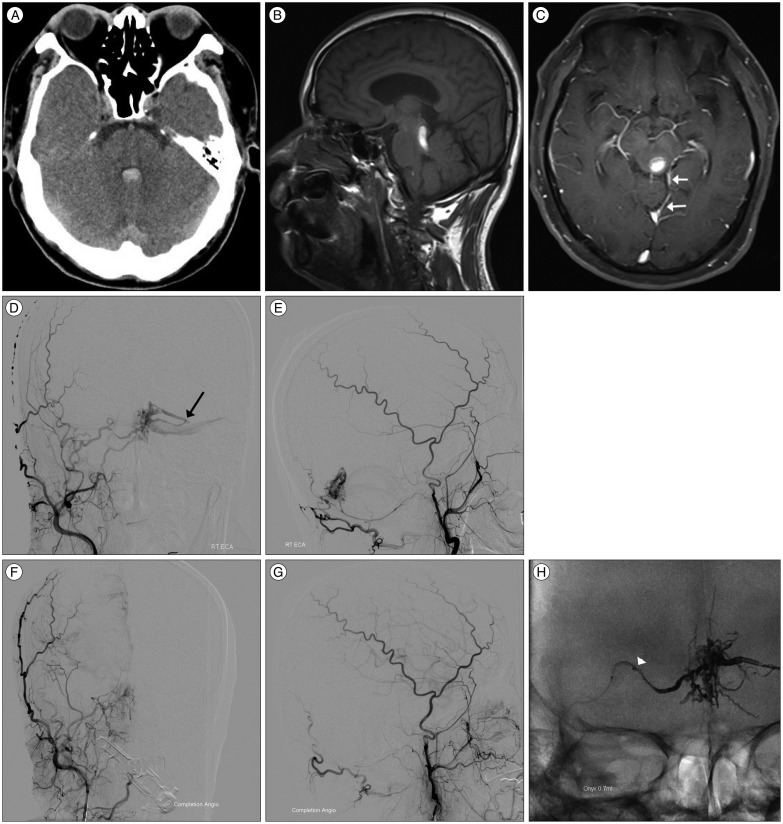
Fig. 2
Case 2. Brain CT image showed a prominent and tortuous vascular structure around medial tentorium (arrow) (A). Brain MR image showed multiple fine vessel engorgements at both thalamic and putamen regions (B). Angiogram demonstrated recanalization and recruitment from right middle meningeal arteries (C) and left middle meningeal arteries (D and E). The retrograde leptomeningeal drain of infratentorial vermian vein showed dilated and saccular change (arrowhead). Vertebral angiogram also showed supply from posterior choroidal artery (F). After embolization of DAVF through the right middle meningeal artery using Onyx, multiple fistula points and common draining vein was occluded and DAVF was obliterated (G : Right external carotid angiogram. H : Left external carotid angiogram. I : Vertebral angiogram. J : Skull lateral view).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download