Abstract
Objective
Methods
Results
Conclusion
References
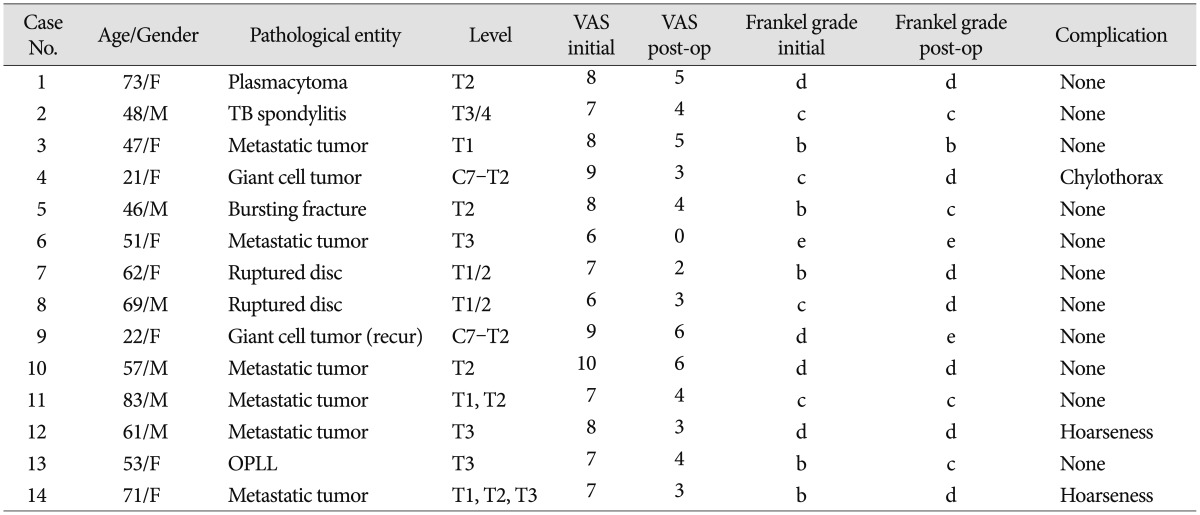
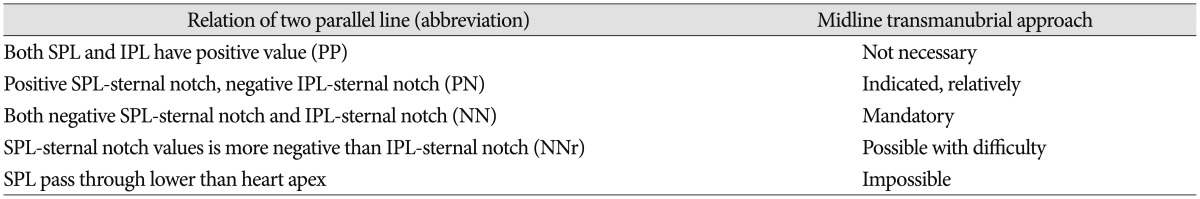
Fig. 1
The superior parallel line (SPL); a straight line parallel to the inferior plateau of the superior healthy vertebrae. The inferior parallel line (IPL); straight line parallel to the superior plateau of the inferior healthy vertebrae. The distances between the sternal notch to the SPL and IPL on the axis of the sternum were measured. * : sternal notch, empty arrow head : point of the SPL meets with sternum, filled arrow head : point of the IPL meets with the sternum.
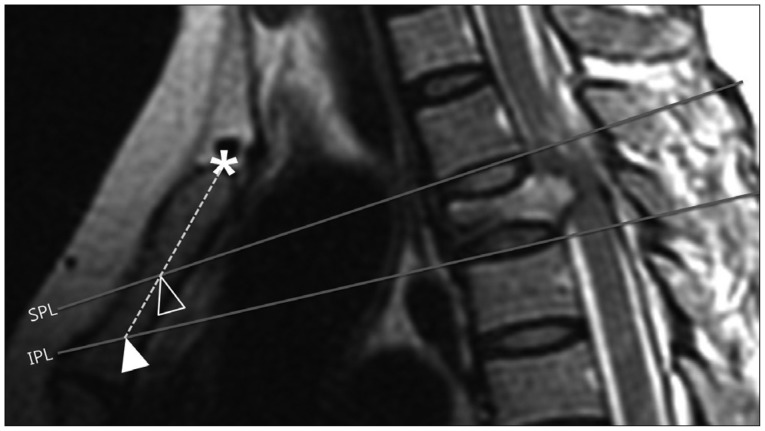
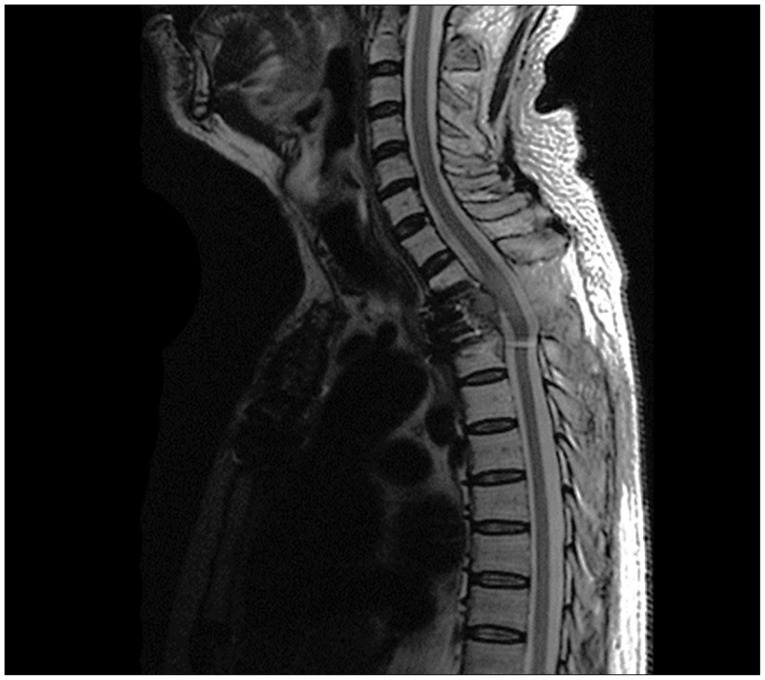
Fig. 2
Schematic illustration of anatomical structure around cervicothoracic junction and inverted Y-shape manubriotomy.
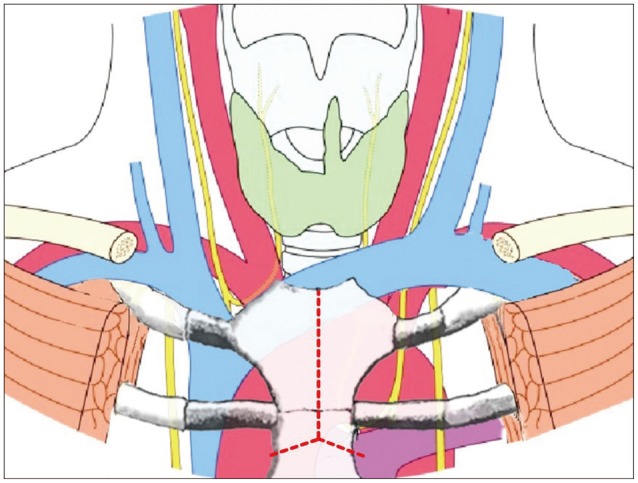
Fig. 3
Intraoperative photograph. A : bisecting manubrium as inverted Y-shaped with oscillating saw. B : Exposure of innominate vein (arrow) after bisecting manubrium after insertion of strong short retractor. C : Innominate vein (arrow) and other anterior visceral structures.
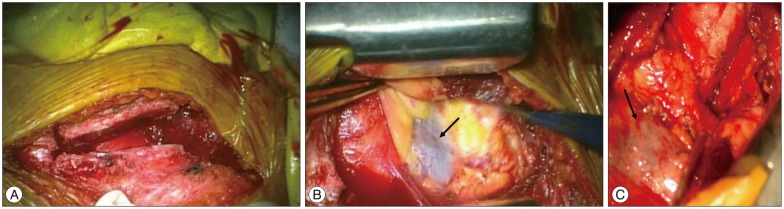
Fig. 4
57 years old man with T2 metastatic tumor. T2 weighted sagittal image shows tumor within T2 vertebral body distorting the cord.
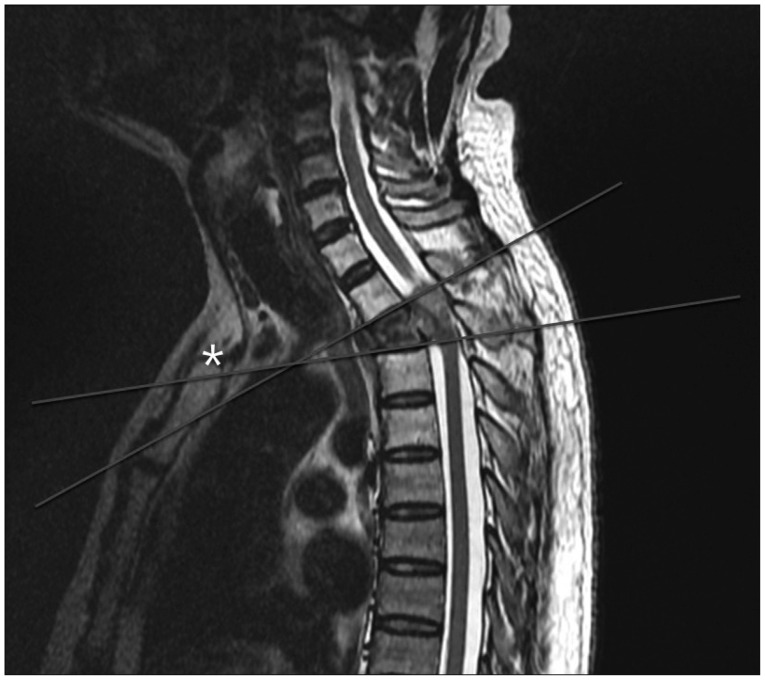
Table 2
Analysis of two parallel line to lesion of CTJ
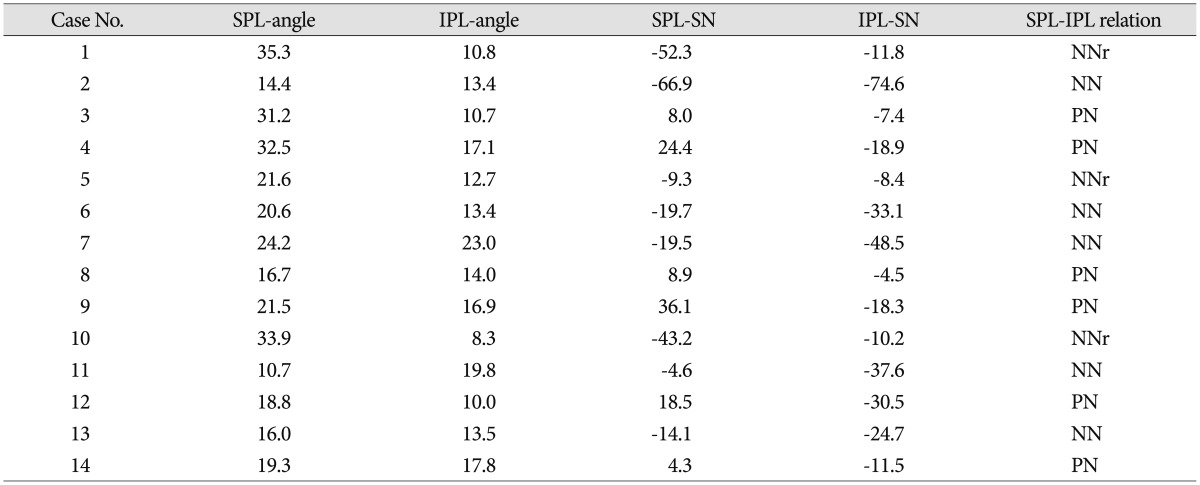
CTJ : cervicothoracic junction, SPL-angle : angle of the horizontal line and superior parallel line (SPL) that define as straight line passing through and parallel to the inferior plateau of the superior healthy vertebrae, IPL-angle : angle of the horizontal line and inferior parallel line (IPL) that define as straight line passing through and parallel to the superior plateau of the inferior healthy vertebrae, SPL-SN : distance from sternal notch (SN) to SPL, IPL-SN : distance from SN to IPL, PN : positive SPL-SN and negative IPL-sternal notch, NN : both negative SPL-SN and IPL-SN, NNr : SPL-SN values is more negative than IPL-SN which means two line is crossing within the mediastinum




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download