Abstract
Objective
Degenerative changes in the cervical spine are commonly accompanied by cervical kyphosis which can cause neck pain. This study examined the relationship between neck pain and cervical alignment.
Methods
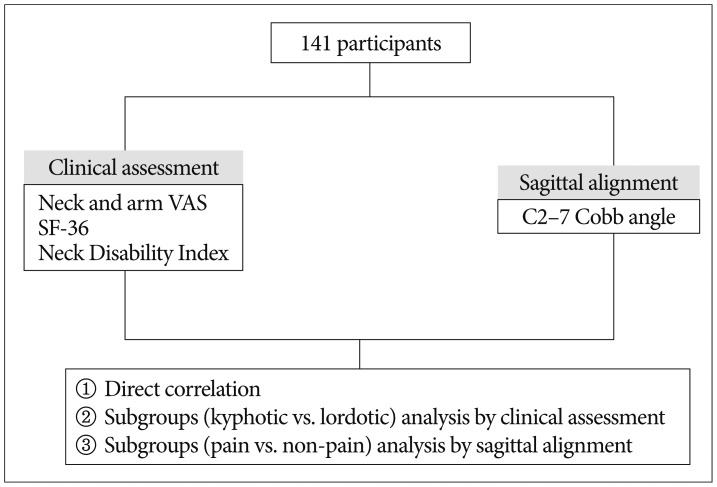
A total of 323 female nursing staff from our hospital were enrolled. Sagittal radiographs of the cervical spine, Body Mass Index (BMI), Visual Analogue Scale (VAS) measures of neck and arm pain, Neck Disability Index (NDI) and the Short Form (36) Health Survey (SF-36 scores) were obtained and reviewed retrospectively. Global lordosis (GL) of the cervical spine was measured on radiograph images. Correlations between GL and questionnaire scores were investigated using the following three methods : 1) correlation between GL and questionnaire scores among the entire sample; 2) subgroup analysis of patients with "kyphosis (KYP) : GL scores<0" vs. those with "lordosis (LOR) : GL scores>0" on questionnaire measures; and 3) subgroup analysis of patients with pain vs. those without pain, on GL and questionnaire measures.
Results
There was no significant correlation between GL and any questionnaire measure. There was a significant difference between the mean GLs of the KYP and LOR groups, but there were no group differences in BMI, age or any questionnaire measures. There was no difference between the pain (n=92) and pain-free (n=231) groups in age, BMI or GL, but there were differences in neck, and arm pain, and physical function and NDI scores.
Normal lordotic curvature represents the ideal state for the cervical spine9), enabling fluid motion and optimal functionality19). During aging, degenerative changes in the cervical spine are commonly accompanied by segmental bone loss or global lordosis, which can cause neck pain516). Although lumbar sagittal alignment has received a considerable amount of attention, cervical sagittal misalignment, and its clinical symptoms, is less understood1819). Several studies have demonstrated that clinical outcomes improve when lordotic curvature is preserved after cervical surgery12), but there is a scarcity of research on patients not undergoing operations.
Our hospital has conducted cervical radiographs, as part of routine physical examinations, for faculty members (e.g., nursing department staff) since 2005. Consequently, a large number of young females with homogenous working conditions are available for analysis. A study by Iizuka et al.11) also assessed neck and shoulder pain among nursing staff, but the relationship between neck pain and cervical alignment was not evaluated. The present study examined the correlation between neck pain and deviations from normal cervical lordosis in young females working under conditions of similar physical intensity who had undergone no previous operation.
Our hospital has conducted cervical radiographs during routine physical examination of faculty members since 2005. Data from 405 nursing staff were collected between 2012 and 2013; 42 retirees, and 40 males, were excluded. Therefore, 323 female nursing staff, working in in- and out-patient departments, were enrolled. No participant had undergone a cervical spine operation previously. The study was approved by the Institutional Review Board of the Human Research Center of our hospital (approval no. KUGH13059-001).
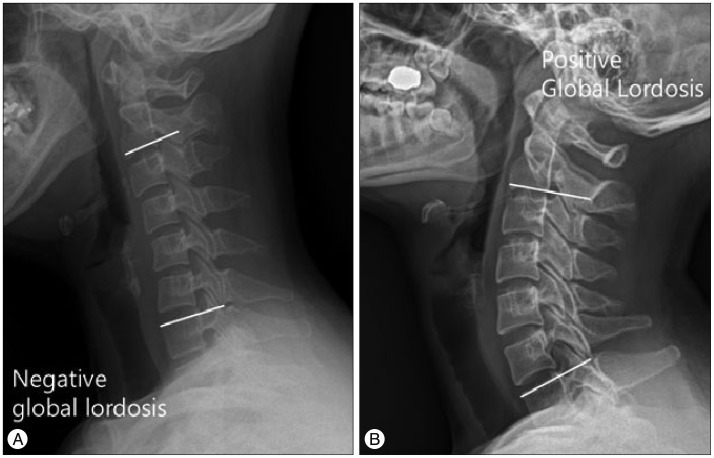
A total of 323 sagittal radiographs of the cervical spine were evaluated. Sagittal alignment was measured using the Cobb method at C2 and C7. Global lordosis (GL) of the cervical spine was defined as the angle between the inferior endplate of C2 and the superior endplate of C7 (Fig. 1)6). Two physicians evaluated the radiographs independently; median values were recorded.
Standardized questionnaires were used to evaluate clinical outcomes, pertaining to age, sex, Body Mass Index (BMI), prior experience of neck and arm pain and cervical surgery and family medical history. Health-related quality of life and functional outcomes were assessed using the Short Form (36) Health Survey (SF-36) questionnaire. Neck Disability Index (NDI) scores indexed chronic disability and activities of daily living. The severity of neck and arm pain was evaluated using Visual Analogue Scales (VASs).
The data were reviewed retrospectively. Correlations between GL and questionnaire measures were investigated using three methods. First, correlations between GL and questionnaire measures were assessed among the entire sample, followed by subgroup analysis of patients with "kyphosis (KYP) : positive GL scores" vs. "lordosis (LOR) : negative GL scores", using the clinical assessment data. In a final analysis, pain and pain-free groups (distinguished according to their response to the question : "Have you ever experienced neck pain?)" were compared. Group differences in sagittal alignment were assessed. Correlation analyses, and independent t-tests for subgroup analyses, were performed using the MedCalc® software package (ver. 14.12.0; MedCalc Software, Oostende, Belgium). The study design is illustrated in Fig. 2.
A total of 323 sagittal plane cervical radiographs were assessed. The GL, defined as the angle between the inferior endplate of C2 and the superior endplate of C7, ranged between -11 and 44 (mean=12.9±11.0).
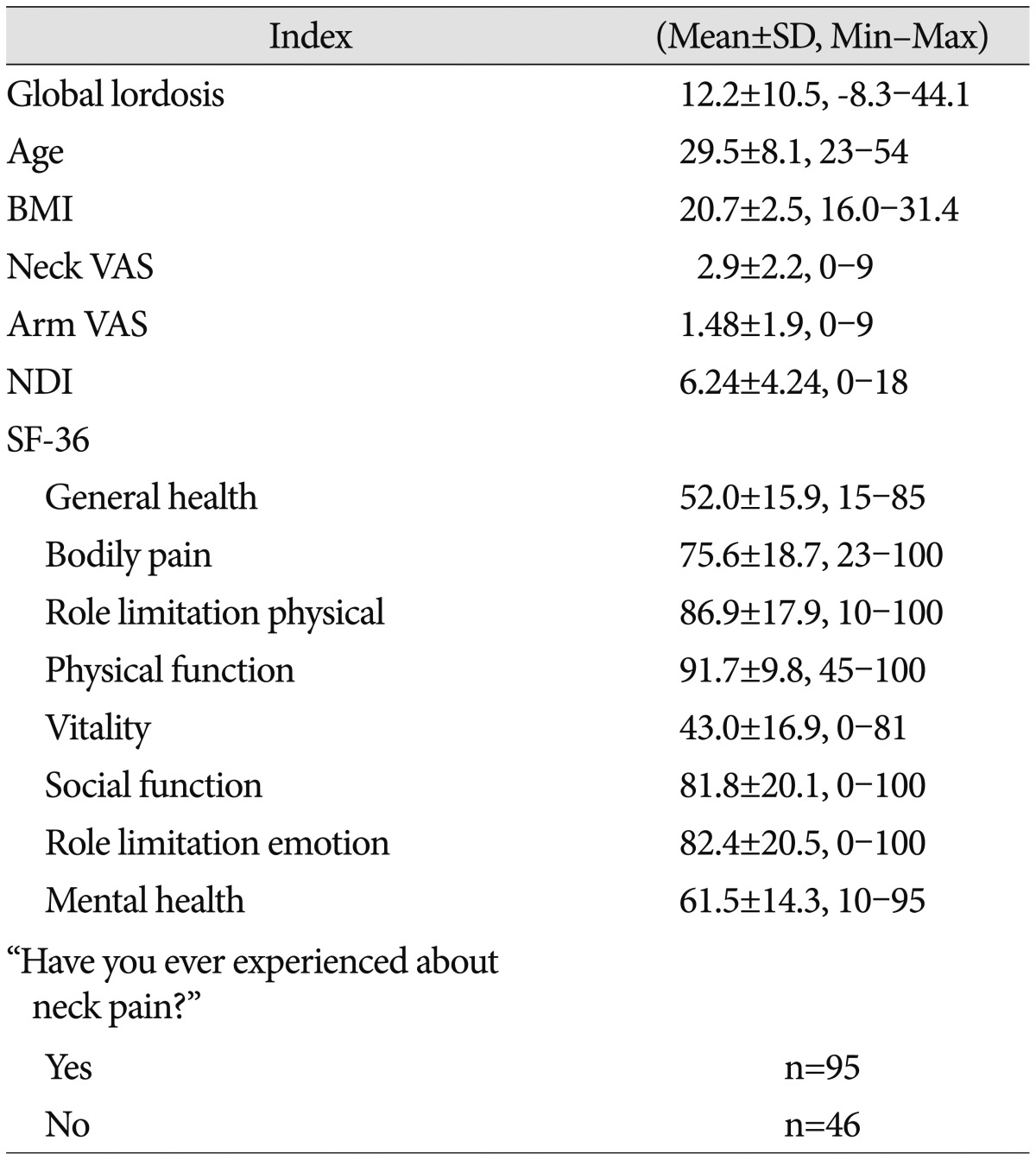
The mean age of the entire sample (n=323) was 30.2±7.7 years (range : 21-55 years). Their mean BMI was 20.6±2.5 (15.6-31.2). Mean VAS neck pain was 3.0±2.2 (0-9) and mean VAS arm pain was 1.7±2.0 (0-9). Patients' mean NDI score was 6.5±4.6. General health, bodily pain, role limitation physical, physical function, vitality, social function, role limitation emotion, and mental health SF-36 subscale scores were 52.6±15.8, (range : 15-100), 75.0±19.2 (23-100), 88.2±16.4 (10-100), 90.0±12.8 (40-100), 42.8±16.9 (0-88), 82.3±18.7 (0-100), 83.3±19.0 (0-100), and 62.2±13.6 (10-95), respectively. A total of 92 participants responded positively to the question : "Have you ever experienced neck pain?" compared to 231 who responded negatively (Table 1).
The 44 patients in whom GL values were negative were included in the kyphotic group; an identical number of those exhaling the greatest degree of lordosis comprised the lordotic group. There was a significant group difference in sagittal alignment (GL value in the kyphotic group=-3.5±2.5 vs. 31.9±5.0 in the lordotic group; p<0.001). However, there were no group differences in age, BMI, neck or arm pain, NDI score or any SF-36 measure.
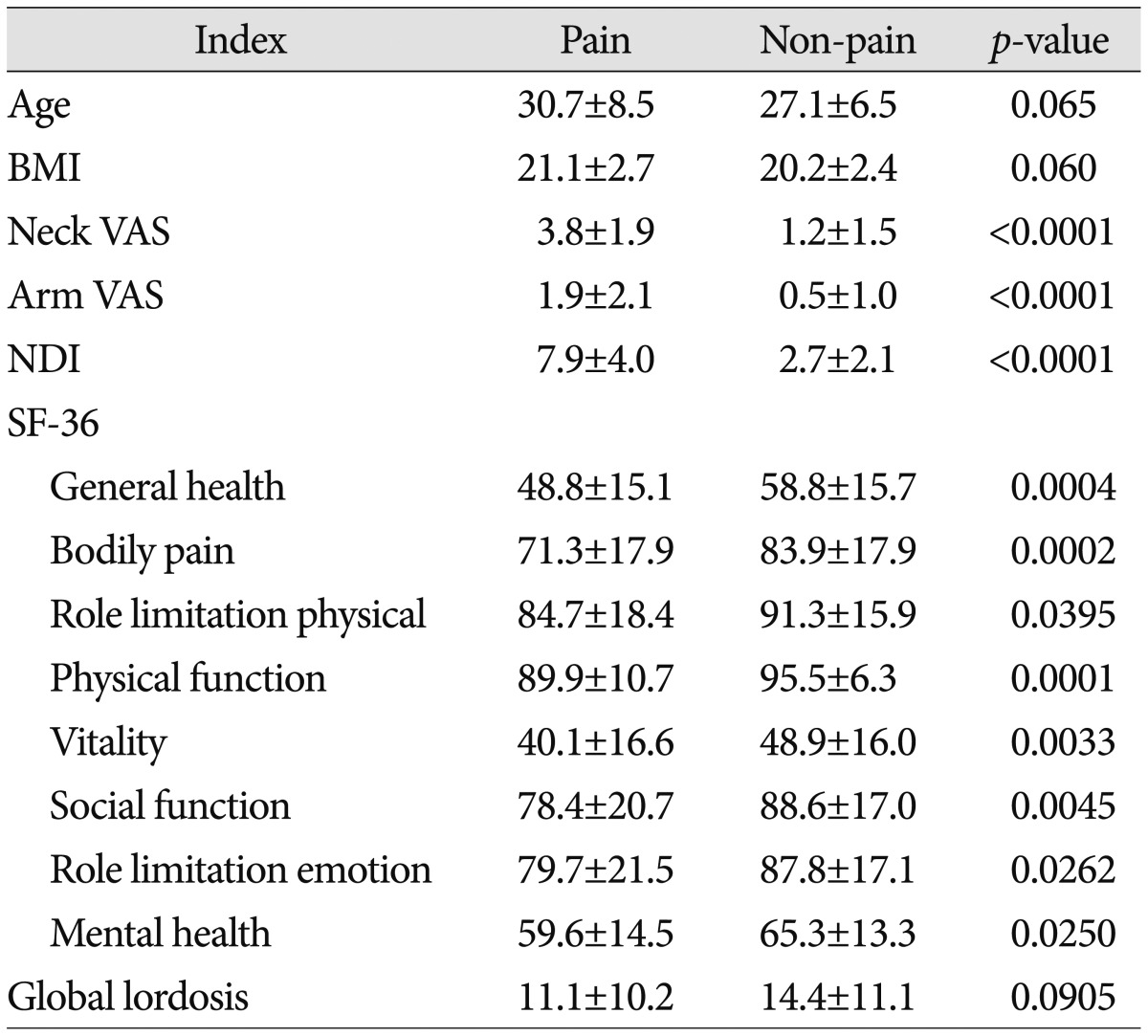
Age and BMI did not differ between the pain (n=92) and pain-free (n=231) groups. VAS neck (3.8±1.9 vs. 1.1±1.5, p=0.004) and arm (2.1±2.1 vs. 0.7±1.4, p<0.001) pain, and physical function (88.5±13.5 vs. 93.9±9.7, p<0.001) and NDI (8.0±4.3 vs. 2.8±2.6, p<0.001) scores, differed between the two groups. However, there was no significant difference in the GL values of the pain (12.5±11.15) and pain-free (14.0±10.7; p=0.684) groups (Table 2).
Commensurate with increases in office-based employment, neck pain, which also affects industrial workers, now represents a highly relevant issue that has received considerable attention17). In Western studies, neck and shoulder pain have been associated with multiple factors, including psychological distress, pain at other bodily sites, smoking, and a range of other medical conditions141314).
This study focused on the relationship between neck pain and cervical alignment. Several previous studies have included similar populations (i.e., nursing staff) : Iizuka et al.11) reported that neck and shoulder pain prevalence in staff at their hospital was 68.1%, which was markedly higher than the figure reported herein (28%; 92 of 323 nurses). Although their study assessed the association between neck and shoulder pain and several factors, cervical sagittal alignment was not among them. Pain is subjective, and its intensity can vary according to multiple factors (e.g., age, sex, personal characteristics, surrounding environment). Furthermore, the scales used to index pain differed between our study and that of Iizuka et al.11); this may account for the marked difference in neck and shoulder pain prevalence. Several studies report neck pain prevalence of approximately 20%, similar to our study, in the general population aged >40 years23). Furthermore, there is general agreement that lordotic curvature of the cervical spine represents its ideal state9), but the relationship between neck pain and cervical lordosis remains poorly understood. During aging, degenerative changes in the cervical spine may include facet joint arthropathy and disc space narrowing, which may result in neck and shoulder pain. The relationship between neck pain and cervical spine kyphosis remains controversial1015). Several studies have demonstrated improved clinical outcomes when lordotic curvature is preserved after cervical surgery : Wu et al.20) reported a correlation between improved Japanese Orthopaedic Association scale scores and C2 and C7 Cobb angles following anterior cervical fusion. Harrison et al.8) suggested that sagittal malalignment after anterior cervical fusion may be related to cervical instability, postoperative axial pain, and progressive neurological detonation, all of which could influence functional recovery. Loss of local cervical lordosis may also alter the dynamic kinematics of the cervical spine and increase biomechanical stress on anterior vertebral elements of neighboring segments, thereby promoting progressive degeneration. Therefore, neurosurgeons should aim for normal cervical lordosis during cervical spine operations.
Patients not undergoing operations are rarely studied. Grob et al.7) reported no association between sagittal alignment of the cervical spine and neck pain. They included 107 volunteers (47 males), with an average age of 68 years (range : 45-90 years) who were undergoing treatment for lower extremity problems, and concluded that, although a degree of lordosis is physiologically normal, the point at which a kyphotic deformity could start to cause problems remains poorly understood. In our study, lordotic curvature of the cervical spine was also unrelated to neck and shoulder pain, suggesting that there is no relationship between cervical kyphosis and neck pain in either young adults or in those aged >45 years.
Our study provides meaningful data on the correlation between pain and cervical alignment, particularly in young, surgically naïve adults. Furthermore, our large sample allowed for subgroup analyses : we assessed the correlation between GL and neck pain among the entire study population, in addition to differences between kyphotic and lordotic groups and pain and pain-free groups. Among all patients, there was no correlation between GL and neck pain. There was also no significant difference between the GL values of the kyphotic vs. lordotic or pain vs. pain-free groups. Neck and shoulder pain may be experienced by patients in whom cervical lordosis is well-preserved; therefore, establishing the etiology of neck pain is important. However, individuals exhibiting marked cervical kyphosis do not always require surgery, because their cervical physiology may remain normal.
This study had several limitations. First, the quality of the sagittal radiographs was not validated. All radiograph images were obtained with patients in a neutral position, but the Cobb angle may have varied among patients. Second, our data lack generalizability because the study was restricted to young, female nursing staff. However, evaluation of neck pain in the general population could be biased by sex, occupation and age differences, such that restricting analyses to a particular group may confer more-reliable data pertaining to the relationship between neck pain and sagittal alignment. Finally, to avoid selection bias a randomized-controlled study design would have been preferable and is recommended for future research.
No difference in the relationship between cervical alignment and clinical questionnaire scores was observed using the three different methods employed herein. Furthermore, our data suggest that kyphotic deformity may not represent the major cause of neck pain, which in turn may not be associated with cervical kyphosis.
References
1. Andersson H, Ejlertsson G, Leden I. Widespread musculoskeletal chronic pain associated with smoking. An epidemiological study in a general rural population. Scand J Rehabil Med. 1998; 30:185–191. PMID: 9782546.

2. Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine (Phila Pa 1976). 1994; 19:1307–1309. PMID: 8066508.

3. Brattberg G, Thorslund M, Wikman A. The prevalence of pain in a general population. The results of a postal survey in a county of Sweden. Pain. 1989; 37:215–222. PMID: 2748195.

4. Bruehl S, Chung OY, Jirjis JN, Biridepalli S. Prevalence of clinical hypertension in patients with chronic pain compared to nonpain general medical patients. Clin J Pain. 2005; 21:147–153. PMID: 15722808.

5. Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons : a ten-year follow-up. Spine (Phila Pa 1976). 2001; 26:2463–2466. PMID: 11707711.

6. Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986; 11:521–524. PMID: 3787320.

7. Grob D, Frauenfelder H, Mannion AF. The association between cervical spine curvature and neck pain. Eur Spine J. 2007; 16:669–678. PMID: 17115202.

8. Harrison DD, Harrison DE, Janik TJ, Cailliet R, Ferrantelli JR, Haas JW, et al. Modeling of the sagittal cervical spine as a method to discriminate hypolordosis : results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine (Phila Pa 1976). 2004; 29:2485–2492. PMID: 15543059.

9. Harrison DD, Troyanovich SJ, Harrison DE, Janik TJ, Murphy DJ. A normal sagittal spinal configuration : a desirable clinical outcome. J Manipulative Physiol Ther. 1996; 19:398–405. PMID: 8864971.
10. Harrison DE, Harrison DD, Janik TJ, William Jones E, Cailliet R, Normand M. Comparison of axial and flexural stresses in lordosis and three buckled configurations of the cervical spine. Clin Biomech (Bristol, Avon). 2001; 16:276–284.

11. Iizuka Y, Shinozaki T, Kobayashi T, Tsutsumi S, Osawa T, Ara T, et al. Characteristics of neck and shoulder pain (called katakori in Japanese) among members of the nursing staff. J Orthop Sci. 2012; 17:46–50. PMID: 22094607.

12. Kawakami M, Tamaki T, Yoshida M, Hayashi N, Ando M, Yamada H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord. 1999; 12:50–56. PMID: 10078950.

13. Linton SJ. A review of psychological risk factors in back and neck pain. Spine (Phila Pa 1976). 2000; 25:1148–1156. PMID: 10788861.

14. Mäkelä M, Heliövaara M, Sievers K, Impivaara O, Knekt P, Aromaa A. Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol. 1991; 134:1356–1367. PMID: 1755449.

15. Marchiori DM, Henderson CN. A cross-sectional study correlating cervical radiographic degenerative findings to pain and disability. Spine (Phila Pa 1976). 1996; 21:2747–2751. PMID: 8979320.

16. Naderi S, Ozgen S, Pamir MN, Ozek MM, Erzen C. Cervical spondylotic myelopathy : surgical results and factors affecting prognosis. Neurosurgery. 1998; 43:43–49. discussion 49-50PMID: 9657187.

17. Sadeghian F, Raei M, Amiri M. Persistent of neck/shoulder pain among computer office workers with specific attention to pain expectation, somatization tendency, and beliefs. Int J Prev Med. 2014; 5:1169–1177. PMID: 25317301.
18. Suzuki H, Endo K, Kobayashi H, Tanaka H, Yamamoto K. Total sagittal spinal alignment in patients with lumbar canal stenosis accompanied by intermittent claudication. Spine (Phila Pa 1976). 2010; 35:E344–E346. PMID: 20375774.

19. Villavicencio AT, Babuska JM, Ashton A, Busch E, Roeca C, Nelson EL, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery. 2011; 68:1309–1316. discussion 1316PMID: 21792113.

20. Wu WJ, Jiang LS, Liang Y, Dai LY. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease : a retrospective study. Eur Spine J. 2012; 21:1374–1382. PMID: 22205113.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download