Abstract
Objective
The clinical outcomes according to the radiological results after cervical total disc replacement (TDR) are not well established. Here, the authors reviewed the clinical results according to the asymmetry in radiographs.
Methods
This retrospective analysis included patients after TDR (Mobi-C® disc) with at least 12 months follow up, and the clinical and radiological data were obtained preoperatively and postoperatively for 12 months. Clinical outcome measures numerical rating scale (NRS) score for neck pain, visual analog scale (VAS) for arm pain, and the Oswestry disability index (ODI) value. The asymmetries of TDRs were evaluated on the anterior-posterior (AP) and the lateral radiographs, and the radiographic adjacent segment degenerations were evaluated for 12 months.
Results
A total of 24 patients (one level cervical TDR; 10 male and 14 female; aged 41.50±8.35 years) were included in this study. The clinical results including NRS for neck pain, VAS for arm pain, and ODIs were similar between the normal and asymmetrized TDRs in AP and lateral radiographs. The radiographic adjacent segment degenerations were significantly increased in deviated TDRs (AP>10 mm asymmetry and lateral>10 mm asymmetry).
Over the last several years, cervical total disc replacement (TDR) surgery has become an increasingly popular alternative to anterior cervical discectomy and fusion (ACDF) in the treatment of refractory cervical spondylosis. Cervical TDR for preserving motions of the operative level has been promoted as a method of decreasing the rate of adjacent segment disease, and lowering the rate of adjacent segment degeneration, compared to ACDF9121415). Cervical TDRs have been gaining popularity, but relatively few studies have been conducted to know the impact of the asymmetry of cervical TDR in correlation to the radiologic and clinical outcome. Herein, the authors conducted this study to evaluate the clinical outcomes and radiological results after cervical TDR with Mobi-C® according to the asymmetry of TDR device in the postoperative anterior-posterior (AP) and the lateral radiographs.
The study included 24 patients who had undergone cervical TDR (Mobi-C® disc; LDR Medical, Troyes, France) with at least 12 months follow-up period at a single university hospital between February, 2008 and May, 2012. The demographic and clinical data were collected after careful review of medical records and radiologic imaging studies with approval of institutional review board. The inclusion criteria in this retrospective series were the patients with TDR due to the radiculopathy and/or myelopathy from disc herniation and other degenerative changes in single level cervical disc disease. The exclusion criteria were multilevel disc operation, hybrid technique, and unsatisfactory follow-up period lesser than 12 months. The age of the patients at the time of surgery was 41.50±8.35 years (range, 24-54 years). All patients had a history of radiculopathy or myelopathy refractory to conservative treatments for a minimum of 6 weeks, with a mean duration of 17.8 months (range, 2-120 months). The preoperative signs and symptoms were radiculopathy in 16 patients (66.7%), myelopathy in 4 patients (16.7%), and combined radiculopathy and myelopathy in 4 patients (16.7%). All operations were conducted by one surgeon with the same surgical protocol.
A standard Smith-Robinson approach was used to expose the treatment levels in all patients11). The cartilaginous endplate was removed with a curette, and care was taken not to damage the bony endplate. The uncovertebral joints were left intact. The arthroplasty used an artificial disc (Mobi-C® disc). The Mobi-C® disc prosthesis is a 3-piece, biarticulating, metal-on-polyethylene, semiconstrained device. It consists of 2 metal base plates with an ultra-high molecular weight polyethylene insert. The insert is considered to have a mobile-bearing technology that allows greater range of motion (ROM)18). There are 2 lateral stops on the inferior endplate that limits the movement of the insert. The Mobi-C® artificial disc has received approval from the Food and Drug Administration to undergo an Investigational Device Exemption trial in the United States. All study patients had prophylactic non-steroidal anti-inflammatory drugs administered. It has an effect of delaying bone formation and reducing incidence of heterotrophic ossification after other total joint replacement procedures7). No patient used a cervical collar after cervical TDR.
Patients were evaluated preoperatively and postoperatively with a period of 1 month, 6 months, and 1 year, with the numeric rating scale (NRS), visual analog scale (VAS), and Oswestry disability index (ODI) score4). Two independent neurosurgeons and one outpatient nurse assessed all clinical outcome data.
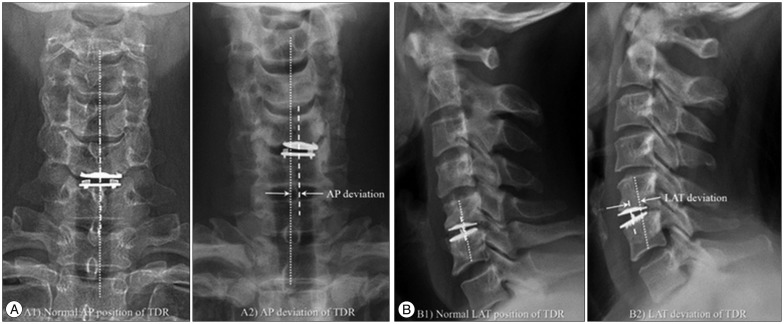
AP, lateral (LAT), flexion, and extension radiographs were obtained preoperatively and postoperatively with a period of 1 month, 6 months, and 1 year. We defined AP asymmetry as a distance from the midline of implant to the midline of cervical spine on AP radiographs and lateral asymmetry as distance from the midline of vertebral body to the midline of device on lateral radiographs (Fig. 1). Upper adjacent angle was measured by using Cobb method drawing a line along the superior endplate of upper level vertebral body and surgical level vertebral body. Lower adjacent angle was measured by drawing a line along the superior endplate of surgical level vertebral body and lower level vertebral body. All angles on all preoperative and postoperative films were checked. The presence of adjacent segment degeneration (ASD) was defined as the pre-established criteria; new anterior osteophyte formation or enlargement of existing osteophytes, new or increased narrowing of a disc space (>30%), new or increased calcification of the anterior longitudinal ligament and the formation of radial osteophytes16). All measurements were performed with picture archival and communication system software (M-view 5.4; Marotech, Seoul, Korea).
Data were expressed as mean±standard deviation. Student t-test analyses were used to compare outcomes between groups. One-way analysis of variance test were performed for some variables. Data were analyzed using a commercially available statistical software package, SPSS 22.0 software for windows (SPSS Inc., Chicago, IL, USA). A p-value<0.05 was considered statistically significant.
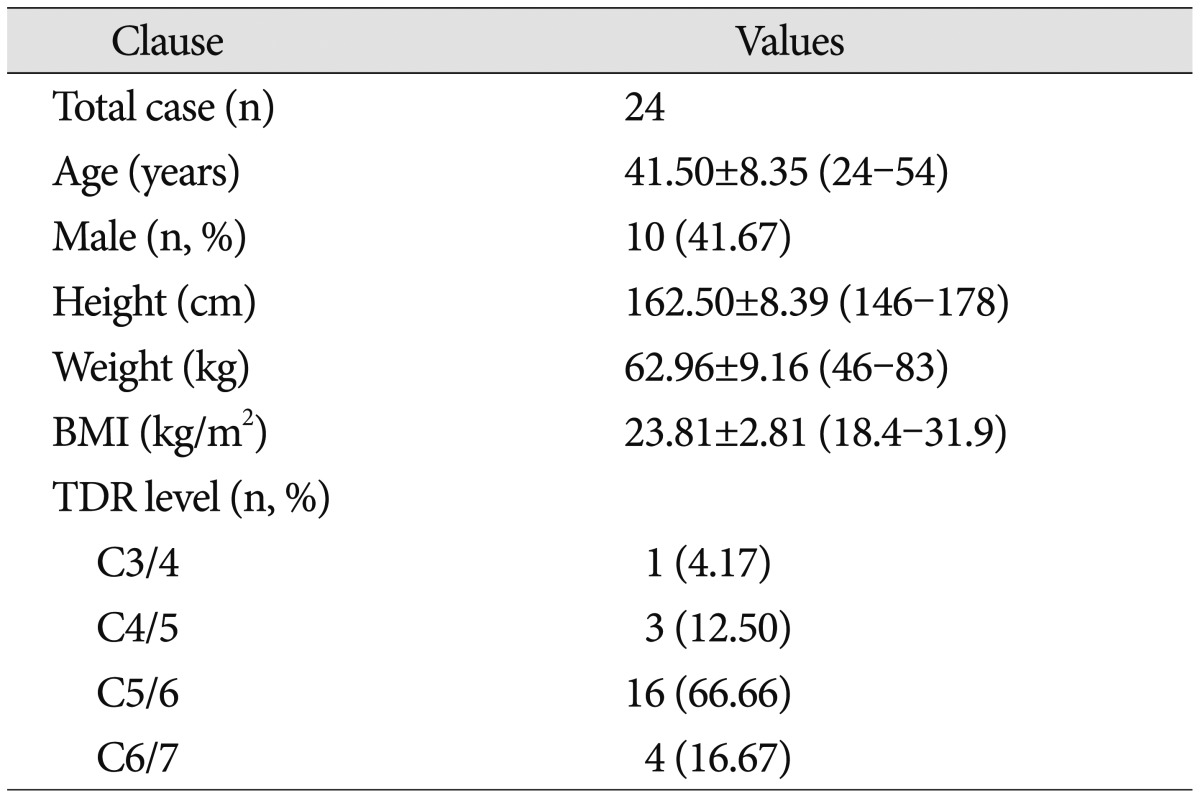
Twenty-four patients (10 men and 14 women) with a mean age of 41.5±8.4 years (range, 24-54 years) were included in this study. The mean follow-up period was 24.4±14 months (range, 12-66 months). All patients underwent a single-level cervical TDR. C5-6 level was most numerous instrumented level (1 patient at C3-4 level, 3 patients at C4-5 level, 16 patients at C5-6 level, and 4 patients at C6-7 level). Table 1 shows demographic characteristics of patients. No patients underwent reoperation in the follow-up period, obvious cervical prosthesis subsidence, excursion or spontaneous fusion of the treated segment.
AP and LAT films were reviewed for AP and LAT asymmetry. The mean AP asymmetry was 0.9±0.7 mm (range, 0.0-2.9 mm). The mean lateral asymmetry was 2.1±1.38 mm [range, -0.8 (posterior asymmetry)-4.3 mm (anterior asymmetry)]. Cases were grouped according to the degree of AP asymmetry (lesser or more than 5 mm or 10 mm) and LAT asymmetry (lesser or more than 10 mm or 20 mm). There were no statistically significant differences in age, sex, smoking, diabetes mellitus, hypertension, estimated surgery blood loss, operation time, and surgery level.
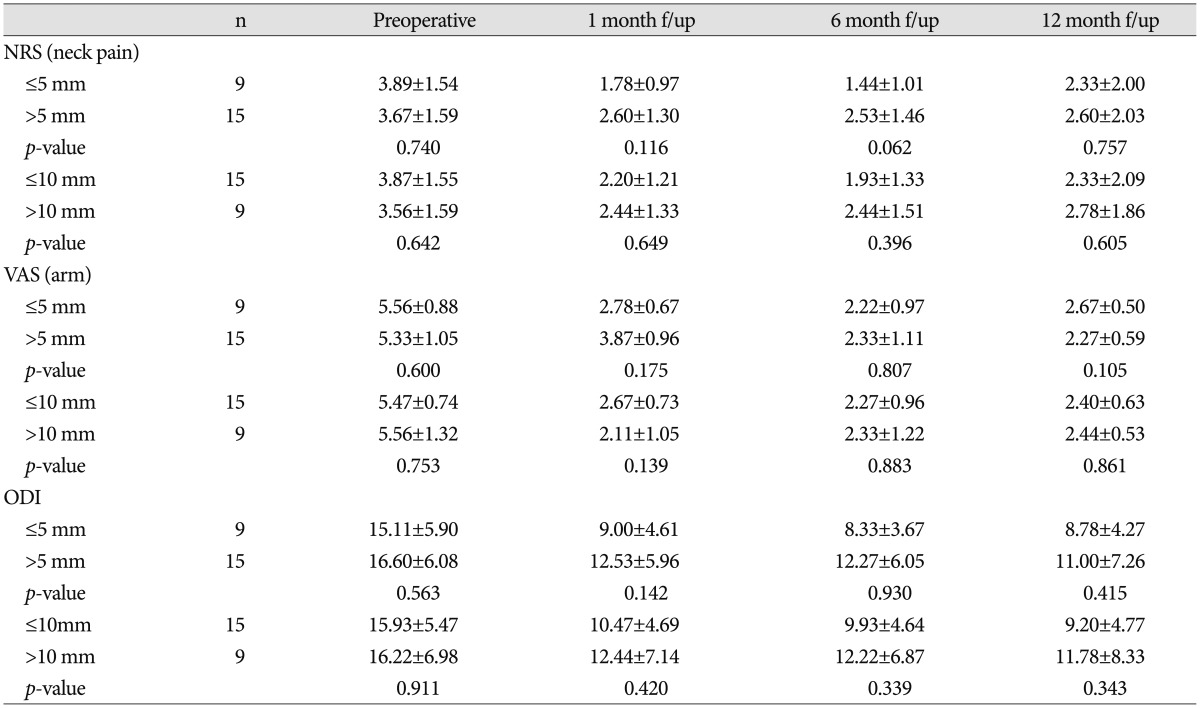
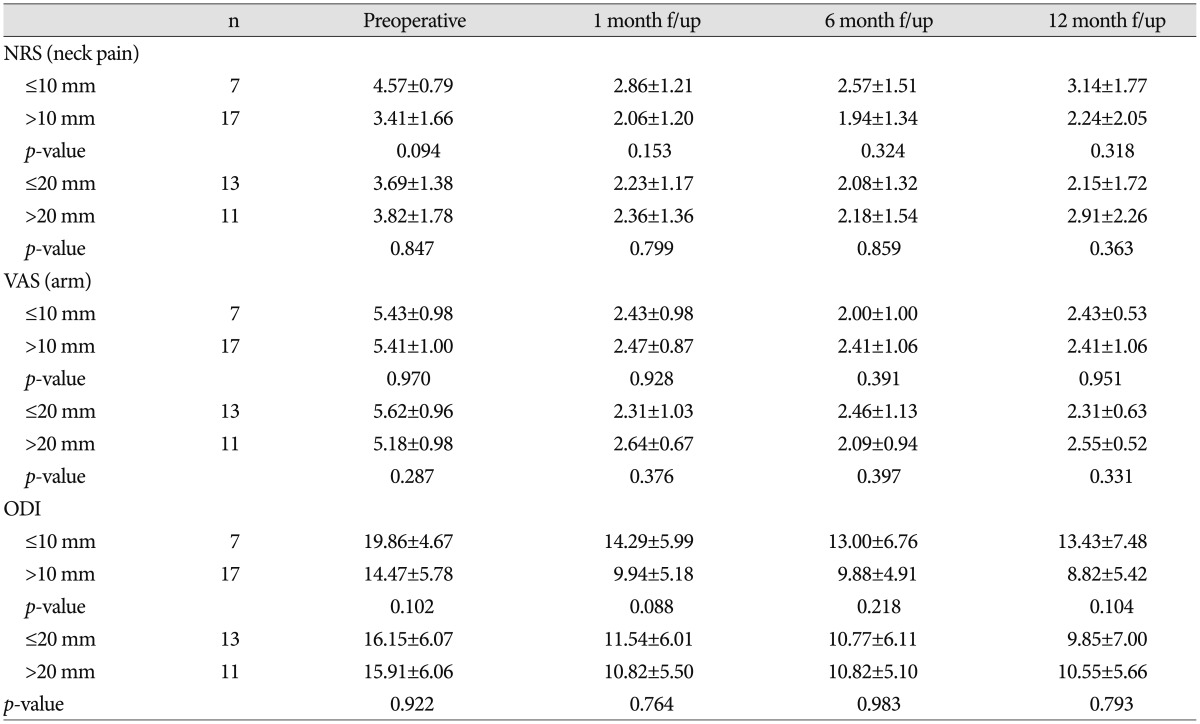
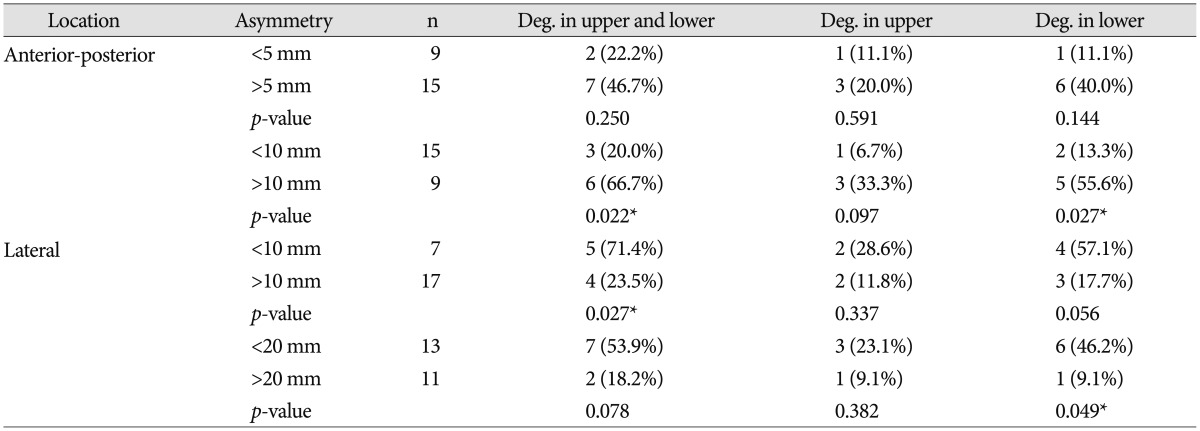
Clinical results such as NRS for neck pain, VAS for arm pain, and ODI according to the asymmetry in AP asymmetry were summarized in Table 2. The degree of AP asymmetry (lesser or more than 5 mm or 10 mm) was not associated with clinical outcomes (NRS, VAS, and ODI) from preoperative status to 12 months follow-up period. Table 3 summarized the clinical results according to the asymmetry in LAT asymmetry, the degrees of LAT asymmetry (lesser or more than 10 mm or 20 mm) were also not associated with clinical outcomes (NRS, VAS, and ODI) from preoperative status to 12 months follow-up period. But, ASDs were checked differently as indicated in Table 4. The AP asymmetry according to the lesser (2 in 7, 22.2%) or more than 5 mm (7 in 15, 46.7%) showed no difference of prevalence of ASD (p=0.250), but the prevalence of ASD was significantly increased in the more than 10 mm AP asymmetry group compared to the lesser than 10 mm AP asymmetry group [3 in 15 (20.0%) vs. 6 in 9 (66.7); p=0.022]. The LAT asymmetry lesser than 10 mm showed significant increase of the ASD prevalence compared to the more than 10 mm LAT asymmetry [5 in 7 (71.4%) vs. 4 in 17 (23.5%), p=0.027], and this inclination also be observed in the comparison of lesser or more than 20 mm in LAT asymmetry [7 in 13 (53.9%) vs. 2 in 11 (18.2%); p=0.078].
For cervical degeneration and cervical disc herniation, ACDF is the standard surgical treatment for symptoms for more than 50 years, with high fusion rate and excellent clinical outcomes3610). However, some studies reported that ACDF also reduces the ROM, and increases adjacent segment degeneration and ossification rate. Over the past decade, cervical TDR emerged as an alternative option for moderate spondylosis and some degree of disc collapse to preserve joint function, reported 1-level and 2-level TDR with overall clinical success rate581315).
During the surgical procedure with TDR, the surgeons obtained the appropriate implant height and position using fluoroscopy and provided trial instruments. However, the technical variation and local anatomic constraints can result the implants failure such as the center positioned off and/or angulated. Clinically, a minimal malposition of implant can be seen occasionally after cervical anterior fusion. We can see that it does not have an effect on clinical and radiological course, but there is no evidence or any systematic study of this idea. However, severe malposition of implants can be associated with direct injury of the sympathetic trunk, vertebral artery, or spinal nerve roots. Most of the related studies were reported in the relationship of ACDF cage implant or plate position and clinical courses. In the study of Ipsen et al.12), there was no significant association between lateralized or rotated plates or plates placed in proximity to adjacent disc spaces, but a worsening short-term clinical outcomes. Yamagata et al.19) also reported that ACDF cage of subsidence resulted in early deterioration of local angle and total alignment of the cervical spine. Amevo et al.1) concluded that the center of rotation at each level of the cervical spine is variable and constantly changing. This conclusion suggests an association between non-centered implant position and the disturbance of the physiologic center of rotation, which can lead to abnormal movement of cervical spine and adjacent degeneration.
Controversy to the result of ACDF studies, only few studies focused on the relationship of TDR implant malposition or angulation and clinical course or vertebral alignment deteriorations21720). Our study focused on the relationship of AP and LAT asymmetry of the implant. The asymmetrical location of TDR is not related to the clinical outcomes, but is related to the risk of radiographic adjacent disc segment degeneration. Interestingly, the ASD prevalence was lower in more than 10 mm LAT asymmetry. This result is similar to the result of Rong et al.17) which reported that the deviated center of rotation in single-level cervical TDR had negative correlation with the flexion-extension ROM. We also agreed with the opinion of single-level cervical TDR restored the natural cervical kinematics with more anteriorly repositioned to preoperative status. Therefore, the change of center of rotation could affect the more favorable ASD result in LAT displaced TDR. Beaurin says the mean center of rotation on lateral X-rays was moved from posterior one third of vertebral body to the posterior half part of the inferior vertebral body after cervical TDR surgery20). So, Mobi-C® implant is originally designed to adapt to the instantaneous axis of rotation through its self-adjusting mobile core1).
In this study, there were few limitations. First of all, this study was designed as retrospective chart and image review, so it is hard to have a precise conclusion between the clinical result and ASD according to the asymmetry of cervical TDR. Secondly, the total number of cases were small and clinical follow-up periods were short, so it could not provide the exact evidence of this topic. The time may have not been sufficient enough to observe the occurrence of symptom since the ASD began. Therefore, well designed large sized controlled study could provide the evidence of this result. However, until now, only this study provides evidence for this interesting topic, what happens when the TDR device is misplaced. The authors considered that this article is the pioneer to explore the unknown medical events.
In conclusion, asymmetrical location of TDR is not related to the clinical outcomes, but related to the risk of radiographic adjacent disc segment degeneration in this retrospective analysis. A large size with long follow-up period is needed to determine the conclusive result of TDR implant asymmetry in clinical outcomes and adjacent segment degeneration.
References
1. Amevo B, Worth D, Bogduk N. Instantaneous axes of rotation of the typical cervical motion segments : a study in normal volunteers. Clin Biomech (Bristol, Avon). 1991; 6:111–117.

2. Barrey C, Champain S, Campana S, Ramadan A, Perrin G, Skalli W. Sagittal alignment and kinematics at instrumented and adjacent levels after total disc replacement in the cervical spine. Eur Spine J. 2012; 21:1648–1659. PMID: 22331142.

3. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993; 75:1298–1307. PMID: 8408151.

4. Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain : the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J. 2010; 10:469–474. PMID: 20359958.

5. Chen J, Wang X, Bai W, Shen X, Yuan W. Prevalence of heterotopic ossification after cervical total disc arthroplasty : a meta-analysis. Eur Spine J. 2012; 21:674–680. PMID: 22134486.

6. Cloward RB. Cervical diskography; technique, indications and use in diagnosis of ruptured cervical disks. Am J Roentgenol Radium Ther Nucl Med. 1958; 79:563–574.
7. Davis RJ, Kim KD, Hisey MS, Hoffman GA, Bae HW, Gaede SE, et al. Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease : a prospective, randomized, controlled multicenter clinical tria l : clinical article. J Neurosurg Spine. 2013; 19:532–545. PMID: 24010901.

8. Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976). 2002; 27:2431–2434. PMID: 12435970.

9. Garrido BJ, Taha TA, Sasso RC. Clinical outcomes of Bryan cervical disc arthroplasty a prospective, randomized, controlled, single site trial with 48-month follow-up. J Spinal Disord Tech. 2010; 23:367–371. PMID: 20087223.

10. Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004; 17:79–85. PMID: 15260088.

11. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999; 81:519–528. PMID: 10225797.

12. Ipsen BJ, Kim DH, Jenis LG, Tromanhauser SG, Banco RJ. Effect of plate position on clinical outcome after anterior cervical spine surgery. Spine J. 2007; 7:637–642. PMID: 17998122.

13. Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976). 1999; 24:670–675. PMID: 10209796.

14. Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion : a randomized controlled clinical trial. J Neurosurg Spine. 2007; 6:198–209. PMID: 17355018.

15. Park JH, Roh KH, Cho JY, Ra YS, Rhim SC, Noh SW. Comparative analysis of cervical arthroplasty using mobi-c(r) and anterior cervical discectomy and fusion using the solis(r) -cage. J Korean Neurosurg Soc. 2008; 44:217–221. PMID: 19096680.

16. Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty : a prospective 2-year study. J Neurosurg Spine. 2005; 3:417–423. PMID: 16381202.

17. Rong X, Gong Q, Liu H, Hong Y, Lou J, Wu W, et al. The effect of deviated center of rotation on flexion-extension range of motion after single-level cervical arthroplasty : an in vivo study. Spine (Phila Pa 1976). 2014; 39(26 Spec No.):B12–B18. PMID: 25271518.
18. Vital JM, Guérin P, Gille O, Pointillart V, Aurouer N, Obeid I. The Mobi-C® cervical disc prosthesis : indications, technique and results. Interact Surg. 2008; 3:181–186.

19. Yamagata T, Takami T, Uda T, Ikeda H, Nagata T, Sakamoto S, et al. Outcomes of contemporary use of rectangular titanium stand-alone cages in anterior cervical discectomy and fusion: cage subsidence and cervical alignment. J Clin Neurosci. 2012; 19:1673–1678. PMID: 23084624.

20. Yue JJ, Bertagnoli R, McAfee PC, An HS. Motion preservation surgery of the spine : advanced techniques and controversies. Philadelphia: Saunders Elsevier;2008. p. 231–237.
Fig. 1
Normal position and anterior-posterior (AP)/lateral (LAT) asymmetry of total disc replacement (TDR). A : AP asymmetry was measured as the distance between the midline of cervical spine and the midline of implant on AP radiographs. B : LAT asymmetry was measured as the distance between the midline of cervical spine and the midline of implant on lateral radiographs.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download