Abstract
A Schmorl's node is defined as a simple endplate intravertebral herniation resulting from trauma or idiopathic causes. Although Schmorl's nodes have been considered clinically insignificant, they might indicate an active symptomatic process or cause serious complications. In this study, we report an interesting case of complete separation of a vertebral body caused by an untreated Schmorl's node accompanying severe osteoporosis. To our knowledge, this is the first clinical report in the published literature to evaluate the complete separation of a vertebral body associated with a Schmorl's node.
The vertebral body may be influenced by herniated intervertebral disc tissue protruding into the vertebral column via fenestrated endplates, forming ectopic deposits of nucleus pulposus material. These deposits are called Schmorl's nodes, and they are regarded as an incidental observation on magnetic resonance imaging (MRI) or plain X-rays of the thoracolumbar spine910). Schmorl's nodes are frequent and incidental findings in persons without back pain, and typically, they are usually asymptomatic and do not require surgical treatment4). However, in some cases, they might denote an active symptomatic process and cause serious complications.
In this study, we report a rare case of an untreated Schmorl's node that resulted delayed in complete separation of the vertebral body with a review of the literature.
A 67-year-old female was admitted to our emergency room. She sustained a lower back pain injury after falling from the bed. She had immediate enduring lower back pain, and in the straight leg raising test (free/free), mild stroke tenderness was noted in the lower lumbar area and a slight limitation of postural change occurred because of pain. The pain was relieved when she rested in bed. No sensory or motor deficits of her lower extremities were noticeable. Plain radiographs revealed moderate scoliosis and right hip joint total replacement with an artificial joint. There was a suspicious bony defect at the L4 upper margin (Fig. 1A). Initial dual energy X-ray absorptiometry bone mineral densitometry disclosed severe osteoporotic change (T-score=-4.0). MRI revealed a Schmorl's node at the L4 level with surrounding edematous change (Fig. 1B, C, D). The patient was treated with bed rest, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy for pain relief for 6 months with mild improvement.
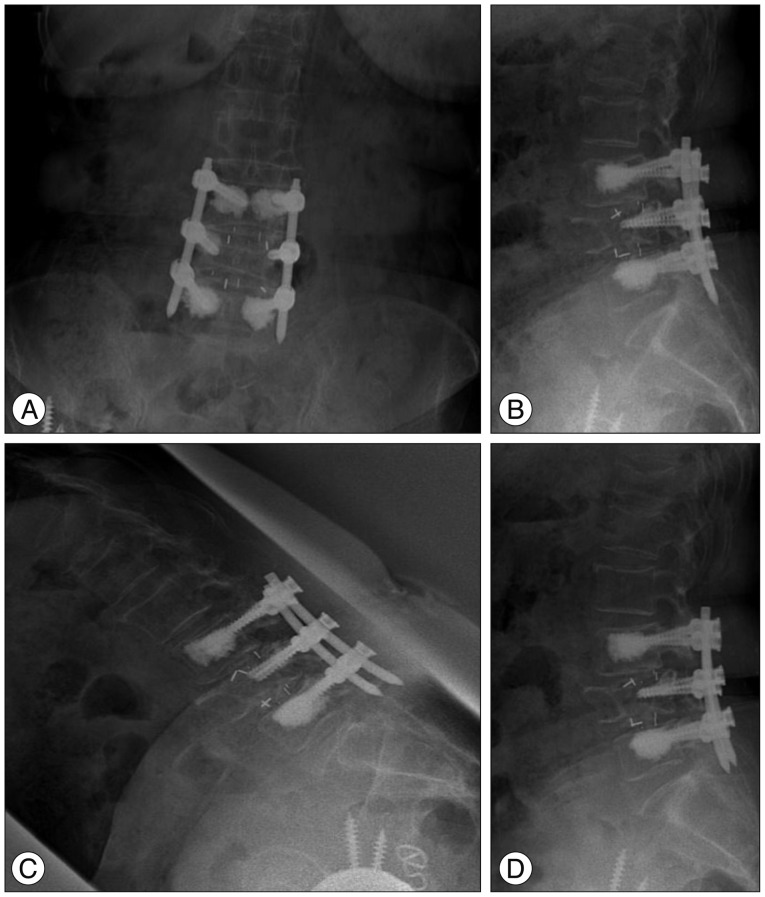
Eighteen months later from her initial hospitalization, she visited our institute again due to severe back pain and immobilization. Against our advice, she had taken oral bisphosphonate drug (FOSAMAX®, MSD Pharma Ceutical Co. Ltd., Korea) irregularly. There was no limitation on bilateral straight leg raising with no loss of motor, sensory, or bowel and bladder function. At this time, radiographs of the lumbar spine revealed a loss of lumbar lordosis and schisis of the L4 vertebral body (Fig. 2A). The spinal canal was severely compressed compared with the initial plain film. Repeated MRI disclosed progression of the Schmorl's node, which caused massive protrusion of the L3-4 disc into the vertebral body of L4, spinal stenosis, and near complete separation of the L4 vertebral body (Fig. 2B, C). A subsequent computed tomography scan revealed a complete separation of the vertebral body (Fig. 2D). She was treated with conservative management including NSAIDs, physical therapy, bracing, and mild narcotics without avail. Due to the patient's severe symptoms and serious radiologic findings, she underwent a bone cement augmented percutaneous posterior lumbar interbody fusion in which the fractured L4 body was not filled with bone cement on concerns of leakage (Fig. 3). Her mechanical low back pain was greatly improved immediately after surgery. She was able to stand straight by postoperative day 2 and discharged 10 days after surgery. On the final follow-up 2 years after surgery, she did not complain of any difficulty with household activities.
Complete separation of the vertebral body associated with a Schmorl's node12). The underlying pathologic lesion is usually a breach in the endplate that permits herniation of disc material into the spongiosa. Theories concerning the pathologic origin of Schmorl's nodes include developmental, degenerative, pathologic, and traumatic causes. Although it is generally accepted that Schmorl's nodes may occur due to minor trauma, to our knowledge, there are no reports in the literature that clearly delineate the cause to be traumatic3).
In our case, the patient had severe osteoporosis and history of a recent fall. Although Schmorl's nodes are relatively common findings in persons without back pain, are typically asymptomatic, and generally do not require treatment, they are sometimes related to spinal tenderness. Symptomatic Schmorl's nodes represent a fresh fracture of the vertebral endplate, frequently in the posterior portion, which allows vertical disc herniation and nuclear migration, and this might cause the diffuse lower back pain without associated radicular findings often observed in transverse-type herniation12). Patients with symptomatic Schmorl's nodes may have pain on percussion and manual compression of the vertebra similar to that of a traumatic compression fracture. In a study by Hamanish et al.5) Schmorl's nodes, which showed abnormal signal intensity on MRI were found to be more frequently in patients with back pain.
Additionally, Takahashi et al.11) recently discovered an interrelation of MRI findings for patients with symptomatic and asymptomatic Schmorl's nodes. They observed a similar appearance in the two groups on plain radiographs, but on MRI, the vertebral body bone marrow surrounding the invaginated node was characterized by a low-intensity signal on T1-weighted sequences and a high-intensity signal on T2-weighted images in symptomatic patients, which were reflective of the bone marrow edema and inflammation often observed in cases of compression fracture.
Clinically, Schmorl's nodes are usually considered asymptomatic. However, in symptomatic patients, such as our patient, the first therapeutic approach should be conservative treatment with pain control (e.g., medication, physical therapy, bracing). If the conservative treatment is ineffective, then surgical treatment should be considered.
Masala et al.8) reported that vertebroplasty, a minimally invasive percutaneous injection of acrylic cement within the vertebral body, can be a possible alternative approach to treating a painful Schmorl's node refractory to conservative therapy such as that associated with a chronic symptomatic osteoporotic compression fracture7).
Hasegawa et al.6) also reported the complete eradication of an intervertebral disc containing a Schmorl's node and lumbar interbody fusion to resolve the painful Schmorl's node. In our case, despite the presence of a symptomatic Schmorl's node, only conservative treatment was applied initially as requested by the patient. Unfortunately, the symptomatic Schmorl's node consequently caused complete separation of the vertebral body over the following year. The patient required surgery because of incapacitating lower back pain and concurrent spinal stenosis that led to progressive neurologic dysfunction.
References
1. Coventry MB, Ghormley RK, Kernohan JW. The intervertebral disc : its microscopic anatomy and pathology : part II. changes in the intervertebral disc concomitant with age. J Bone Joint Surg Am. 1945; 27:233–247.
2. Coventry MB, Ghormley RK, Kernohan JW. The intervertebral disc : its microscopic anatomy and pathology : part III. pathological changes in the intervertebral disc. J Bone Joint Surg Am. 1945; 27:460–474.
3. Dimar JR 2nd, Nathan ST, Glassman SD. The spectrum of traumatic Schmorl's nodes : identification and treatment options in 3 patients. Am J Orthop (Belle Mead NJ). 2012; 41:427–431. PMID: 23365812.
4. Fahey V, Opeskin K, Silberstein M, Anderson R, Briggs C. The pathogenesis of Schmorl's nodes in relation to acute trauma. An autopsy study. Spine (Phila Pa 1976). 1998; 23:2272–2275. PMID: 9820905.
5. Hamanishi C, Kawabata T, Yosii T, Tanaka S. Schmorl's nodes on magnetic resonance imaging. Their incidence and clinical relevance. Spine (Phila Pa 1976). 1994; 19:450–453. PMID: 8178234.
6. Hasegawa K, Ogose A, Morita T, Hirata Y. Painful Schmorl's node treated by lumbar interbody fusion. Spinal Cord. 2004; 42:124–128. PMID: 14765146.

7. Kim HS, Kim SH, Ju CI, Kim SW, Lee SM, Shin H. The role of bone cement augmentation in the treatment of chronic symptomatic osteoporotic compression fracture. J Korean Neurosurg Soc. 2010; 48:490–495.

8. Masala S, Pipitone V, Tomassini M, Massari F, Romagnoli A, Simonetti G. Percutaneous vertebroplasty in painful schmorl nodes. Cardiovasc Intervent Radiol. 2006; 29:97–101. PMID: 16328689.

9. Möller A, Maly P, Besjakov J, Hasserius R, Ohlin A, Karlsson MK. A vertebral fracture in childhood is not a risk factor for disc degeneration but for Schmorl's nodes : a mean 40-year observational study. Spine (Phila Pa 1976). 2007; 32:2487–2492. PMID: 18090090.

10. Resnick D, Niwayama G. Intravertebral disk herniations : cartilaginous (Schmorl's) nodes. Radiology. 1978; 126:57–65. PMID: 339268.

11. Takahashi K, Miyazaki T, Ohnari H, Takino T, Tomita K. Schmorl's nodes and low-back pain. Analysis of magnetic resonance imaging findings in symptomatic and asymptomatic individuals. Eur Spine J. 1995; 4:56–59. PMID: 7749909.
12. Takahashi K, Takata K. A large painful Schmorl's node : a case report. J Spinal Disord. 1994; 7:77–81. PMID: 8186593.
Fig. 1
A symptomatic Schmorl's node arising after a trivial injury in a 67-year-old woman. A : Simple lateral radiograph at the time of initial injury reveals minimal bony change at the middle and posterior endplate of L4. B, C and D : Sagittal T2, fat suppression, and axial T2 magnetic resonance images present a minimal Schmorl's node at L4 and surrounding edematous change.
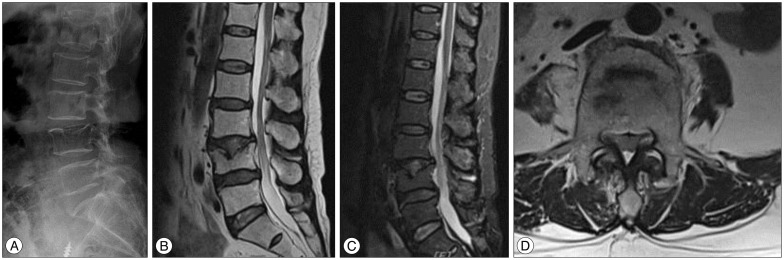
Fig. 2
A developed Schmorl's node with complete separation of the vertebral body after 18 months. A : Simple lateral radiograph shows separation of the vertebral body at L4. B and C : Follow-up magnetic resonance images reveal a large defect and fragmentation within the vertebral body with concurrent spinal stenosis. D : Computed tomography reveals complete separation of the vertebral body at L4.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download