Abstract
We report a 10-year-old boy with supratentorial cortical ependymoma that rapidly grew in the course of 3 years. He suffered generalized seizures when he was 5 years old; MRI showed a small cortical lesion in the right postcentral gyrus. MRI performed 2 years later revealed no changes. For the next 3 years he was free of seizures. However, at the age of 10 he again suffered generalized seizures and MRI disclosed a large parietal tumor. It was resected totally and he remains free of neurological deficits. The histopathological diagnosis was ependymoma. Pediatric supratentorial cortical ependymomas are extremely rare. We recommend including cortical ependymoma as a differential diagnosis in pediatric patients with cortical mass lesions presenting with seizures and careful follow-up even in the absence of symptoms because these tumors may progress.
Along with malformations in the cortical development or cortical dysplasia, hippocampal sclerosis, and remote ischemic damage, in pediatric patients tumors are among the more commonly identifiable causes of seizures. In children with supratentorial cortical mass lesions presenting with seizures, the differential diagnosis usually includes ganglioglioma, dysembryoplastic neuroepithelial tumor (DNT), low-grade glioma, and cortical dysplasia but not ependymoma. Most ependymomas arise from the wall of the ventricles, only few originate at sites distal to the ventricular system where the normal ependymal layer is absent. They rarely arise within the cerebral cortex where they are known as cortical ependymomas (CEs) and often present with seizures. Pediatric supratentorial CEs are extremely rare; only 17 pediatric patients, including ours, have been reported to date2345678911172021232728). We encountered a 10-year-old body with CE presenting with seizures and discuss its clinicopathological features.
This 10-year-old boy first suffered seizures in 2007 when he was 5 years old. They started on the left side of his face and became generalized. Cranial magnetic resonance imaging (MRI) showed a 14-mm diameter cortical lesion in the right postcentral gyrus (Fig. 1A, B). It was slightly hypointense on T1-weighted MRI, hyperintense on fluid-attenuated inversion recovery images and not Gd-contrast-enhanced. The preliminary differential diagnosis included DNT, ganglioglioma, low-grade glioma, and cortical dysplasia but not ependymoma. He was placed under observation because the tumor was thought to be benign. No anticonvulsants were prescribed because his electroencephalogram was normal. Repeat MRI studies performed 2 years later revealed no changes in the size and radiological features of the tumor. He was not seen in the next 3 years because he suffered no further seizures. However, in 2012 when he was 10 years old he again had generalized seizures. MRI showed a 40 mm diameter parietal tumor that was heterogeneously Gd enhanced (Fig. 1C, D). As there was radiographic evidence suggestive of malignant transformation we chose to remove the tumor.
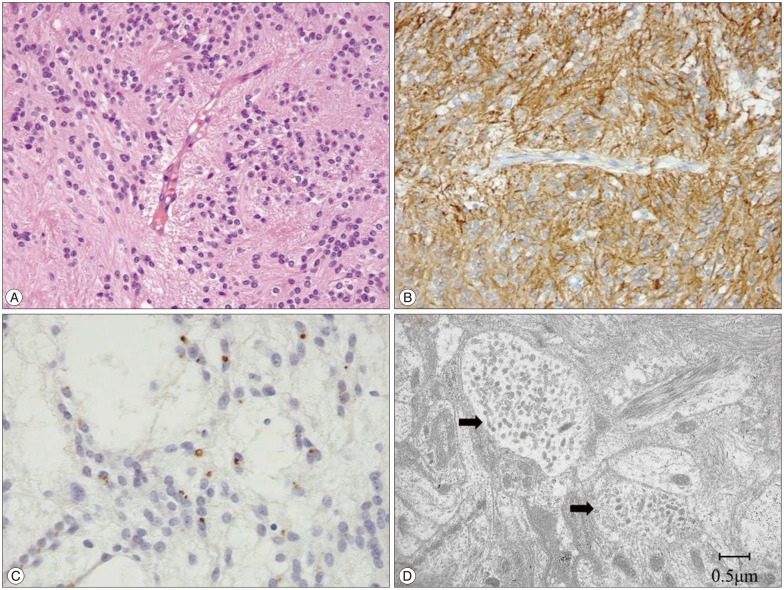
After right frontoparietal craniotomy we observed a reddish-gray tumor on the surface of the postcentral gyrus; it was not covered by brain parenchyma (Fig. 2). It was well demarcated from surrounding brain tissue, had no attachment to the lateral ventricle, and was gross-totally removed. Histologically, the tumor cells were arranged around vessels. Their radially-oriented cell processes were directed at the vessels, thereby producing the perivascular pseudorosettes typical of ependymoma (Fig. 3A). In some areas there were oligodendroglioma-like cells with round nuclei and clear cytoplasm. No true ependymal rosettes were observed. We noted the intermingling of an increased number of abnormal vessels but no other anaplastic features. Immunohistochemically the tumor cells were positive for glial fibrillary acidic protein (GFAP) (Fig. 3B), S-100 protein, and epithelial membrane antigen (EMA) (Fig. 3C). The MIB-1 labeling index was 6.4%. Electron microscopy confirmed the typical presence of microvilli (Fig. 3D). These additional findings confirmed our histopathological diagnosis of ependymoma, World Health Organization (WHO) grade II.
The patient made a good recovery and manifested no neurological deficits. We prescribed carbamazepine and he suffered no further seizures. On follow-up brain MRI scans there was no evidence of residual tumor. Neither adjuvant radiotherapy nor chemotherapy was delivered because the tumor had been resected gross-totally and exhibited no anaplastic features on histopathologic study. Follow-up brain MRI performed 6 and 12 months after the operation yielded no evidence of tumor recurrence.
Tumors are commonly the cause of seizures in pediatric patients. Prayson18) reported that the most common tumors encountered in this population included ganglioglioma (37.2%), DNT (13.2%), low-grade fibrillary astrocytoma (11.6%), and oligoastrocytoma (6.2%); he identified coexisting malformations of cortical development or cortical dysplasia in one-third of patients with these tumors. When we encounter pediatric supratentorial cortical mass lesions presenting with seizures, our differential diagnosis usually includes ganglioglioma, DNT, low-grade glioma, and cortical dysplasia but not ependymoma.
Ependymomas comprise 2-9% of all neuroepithelial neoplasms13), 40% are supratentorial and the others are infratentorial15). Posterior fossa ependymomas are seen mostly in children, supratentorial ependymomas (STEs) tend to arise in older age groups. Ependymomas tend to arise in the lateral or fourth ventricles1). Ectopic ependymomas at sites distant to the ventricular system are relatively rare and they are seldomly seen in the cerebral cortex where they are known as CEs16). Hypotheses for the ectopic origin of ependymomas suggest their development from a heterotopic ependymal nest due to anomalous migration from the germinal matrix; glial cells with progenitor cell properties have also been proposed as the source of these tumors2324).
Pediatric supratentorial cortical mass lesions presenting with seizures are often diagnosed radiographically as ganglioglioma, DNT, low-grade glioma, or cortical dysplasia. It is difficult to differentiate CEs from these tumors because CEs are extremely rare and their radiological features are non-specific except that, unlike those neoplasms, CEs are usually not located in the temporal lobe. Frontal and parietal regions are the most common locations for CEs11). Wang et al.26) reported a new entity, angiocentric glioma (AG), as a neoplasm with features similar to CEs. AGs are superficial tumors occurring in children and young adults; they account for 2.3% in tumor-induced epilepsy in children18). They are epileptogenic and generally characterized by their indolent behavior. Radiologically, they are hyperintense on T2-weighted sequences and not contrast-enhanced on T1-weighted MRI. Lellouch-Tubiana et al.10) and Preusser et al.19) observed a cortical rim of hyperintensity on T1-weighted images. They also reported stalk-like extensions to the adjacent ventricle on T2 images, findings they suggested to be pathognomonic of angiocentric glioma. Histologically, the constituent cells are monophorous and angiocentric with perivascular pseudorosettes and they demonstrate a characteristic dot-like EMA staining pattern. The existence of common features in CEs and angiocentric gliomas has been debated in the neuropathological literature12). We did not observe the non-radial, circumferential and longitudinal angiocentric growth pattern and bipolar spindle cells that are typically seen in AG. Moreover, the tumor progression and changed radiological features in our case are very unusual in AG. Consequently, we did not diagnose our tumor as AG.
Pediatric supratentorial cortical mass lesions presenting with seizures are often followed without resection because they rarely progress. However, as evidenced in our patient, CEs must be followed carefully to alert to tumor progression. Ohwaki et al.17) reported a child with a parietal cortical mass measuring 8 mm in diameter whose size remained stable for 16 months and then grew to 4 cm in the course of 8 months. The histological diagnosis was ependymoma (WHO grade II) although the MIB-1 labeling index was high at 27.5%. Takeshima et al.22) encountered an adult with a small cortical mass in the frontal lobe whose size remained stable for 2 years before turning into a huge tumor during the subsequent 18 months. The histological diagnosis was anaplastic ependymoma; the MIB-1 labeling index was 20%. They concluded that the rapid tumor growth was due to malignant transformation. Although CEs may progress, compared to other STEs their prognosis is relatively favorable, possibly because of their early detection due to the elicitation of seizures, the possibility of complete resection facilitated by their superficial location, their distinct tumor margin, and their tendency to be histologically benign14212325).
We reported a pediatric patient with supratentorial CE. In the differential diagnosis of pediatric supratentorial cortical mass lesions presenting with seizures, ependymoma should be considered and these tumors must be followed carefully because they may progress. The prognosis of these tumors is favorable if they are diagnosed early and accurately and if they are addressed properly.
References
1. Afra D, Müller W, Slowik F, Wilcke O, Budka H, Turoczy L. Supratentorial lobar ependymomas : reports on the grading and survival periods in 80 cases, including 46 recurrences. Acta Neurochir (Wien). 1983; 69:243–251. PMID: 6650239.

2. Fujimoto K, Ohnishi H, Koshimae N, Ida Y, Kanemoto Y, Motoyama Y, et al. [Brain surface clear cell ependymoma : case report]. No Shinkei Geka. 1999; 27:843–846. PMID: 10478346.
3. Ghani AR, Abdullah JM, Ghazali M, Ahmad F, Ahmad KA, Madhavan M. Recurrent paediatric supratentorial extraventricular ependymoma associated with genetic mutation at exon 4 of p53 gene. Singapore Med J. 2008; 49:e192–e194. PMID: 18695856.
4. Grajkowska W, Matyja E, Pronicki M, Daszkiewicz P, Roszkowski M, Perek D, et al. Papillary ependymoma with unique superficial cortical location : immunohistochemical and ultrastructural studies. A case report. Folia Neuropathol. 2009; 47:354–361. PMID: 20054788.
5. Hamano E, Tsutsumi S, Nonaka Y, Abe Y, Yasumoto Y, Saeki H. Huge supratentorial extraventricular anaplastic ependymoma presenting with massive calcification-case report. Neurol Med Chir (Tokyo). 2010; 50:150–153. PMID: 20185883.

6. Hiniker A, Lee HS, Chang S, Berger M, Perry A. Cortical ependymoma with unusual histologic features. Clin Neuropathol. 2013; 32:318–323. PMID: 23458270.

7. Lee SK, Lim DJ, Kim SD. Supratentorial cortical ependymoma in a 21-month-old boy. J Korean Neurosurg Soc. 2011; 50:244–247. PMID: 22102957.

8. Lehman NL. Patterns of brain infiltration and secondary structure formation in supratentorial ependymal tumors. J Neuropathol Exp Neurol. 2008; 67:900–910. PMID: 18716554.

9. Lehman NL, Jorden MA, Huhn SL, Barnes PD, Nelson GB, Fisher PG, et al. Cortical ependymoma. A case report and review. Pediatr Neurosurg. 2003; 39:50–54. PMID: 12784079.
10. Lellouch-Tubiana A, Boddaert N, Bourgeois M, Fohlen M, Jouvet A, Delalande O. Angiocentric neuroepithelial tumor (ANET) : a new epilepsy-related clinicopathological entity with distinctive MRI. Brain Pathol. 2005; 15:281–286. PMID: 16389940.

11. Liu Z, Li J, Liu Z, Wang Q, Famer P, Mehta A, et al. Supratentorial cortical ependymoma : case series and review of the literature. Neuropathology. 2014; 34:243–252. PMID: 24354554.

12. Lum DJ, Halliday W, Watson M, Smith A, Law A. Cortical ependymoma or monomorphous angiocentric glioma? Neuropathology. 2008; 28:81–86. PMID: 18021197.

13. Massimino M, Buttarelli FR, Antonelli M, Gandola L, Modena P, Giangaspero F. Intracranial ependymoma : factors affecting outcome. Future Oncol. 2009; 5:207–216. PMID: 19284379.
14. Miyazawa T, Hirose T, Nakanishi K, Uozumi Y, Tsuzuki N, Shima K. Supratentorial ectopic cortical ependymoma occurring with intratumoral hemorrhage. Brain Tumor Pathol. 2007; 24:35–40. PMID: 18095143.

15. Molina OM, Colina JL, Luzardo GD, Mendez OE, Cardozo D, Velasquez HS, et al. Extraventricular cerebral anaplastic ependymomas. Surg Neurol. 1999; 51:630–635. PMID: 10369231.

16. Nakamizo S, Sasayama T, Kondoh T, Inoue S, Shiomi R, Tanaka H, et al. Supratentorial pure cortical ependymoma. J Clin Neurosci. 2012; 19:1453–1455. PMID: 22898199.

17. Ohwaki K, Tanishima T, Yoshimasu N, Hojo S, Fujimaki T, Kirino T. [Rapidly enlarging supratentorial ependymoma in a child presenting initially with a small calcified lesion : case report]. No Shinkei Geka. 1997; 25:713–718. PMID: 9266564.
18. Prayson RA. Tumours arising in the setting of paediatric chronic epilepsy. Pathology. 2010; 42:426–431. PMID: 20632818.

19. Preusser M, Hoischen A, Novak K, Czech T, Prayer D, Hainfellner JA, et al. Angiocentric glioma : report of clinico-pathologic and genetic findings in 8 cases. Am J Surg Pathol. 2007; 31:1709–1718. PMID: 18059228.
20. Rigante L, Novello M, Massimi L, Caldarelli M. A cortical cystic epileptogenic lesion : tanycytic ependymoma. Acta Neurol Belg. 2013; 113:523–525. PMID: 23160807.

21. Roncaroli F, Consales A, Fioravanti A, Cenacchi G. Supratentorial cortical ependymoma : report of three cases. Neurosurgery. 2005; 57:E192. discussion E192. PMID: 15987557.
22. Takeshima H, Kawahara T, Uchida H, Hirano H, Nakazato Y, Kuratsu J. Brain surface ependymoma with repeated episodes of intratumoral hemorrhage-case report. Neurol Med Chir (Tokyo). 2002; 42:166–169. PMID: 12013669.

23. Van Gompel JJ, Koeller KK, Meyer FB, Marsh WR, Burger PC, Roncaroli F, et al. Cortical ependymoma : an unusual epileptogenic lesion. J Neurosurg. 2011; 114:1187–1194. PMID: 21235315.
24. Vernet O, Farmer JP, Meagher-Villemure K, Montes JL. Supratentorial ectopic ependymoma. Can J Neurol Sci. 1995; 22:316–319. PMID: 8599779.

25. Vinchon M, Soto-Ares G, Riffaud L, Ruchoux MM, Dhellemmes P. Supratentorial ependymoma in children. Pediatr Neurosurg. 2001; 34:77–87. PMID: 11287807.

26. Wang M, Tihan T, Rojiani AM, Bodhireddy SR, Prayson RA, Iacuone JJ, et al. Monomorphous angiocentric glioma : a distinctive epileptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol. 2005; 64:875–881. PMID: 16215459.

27. Yadav YR, Neha , Chandrakar SK. Pure cortical supratentorial extraventricular ependymoma. Neurol India. 2009; 57:213–215. PMID: 19439861.

28. Yurt A, Selçuki M, Ertürk AR, Küpelioglu A. Large supratentorial cortical ependymoma in a child. Clin Med Res. 2010; 8:25–27. PMID: 20305147.

Fig. 1
A and B : MRI scan obtained in 2007 showing a small 14 mm diameter cortical lesion in the right postcentral gyrus. It was hyperintense on the FLAIR image (A), and not gadolinium enhanced (B). C and D : FLAIR image obtained in 2012 showing a large 4 cm diameter parietal tumor (C). It was heterogeneously gadolinium-enhanced (D). FLAIR : fluid-attenuated inversion recovery.
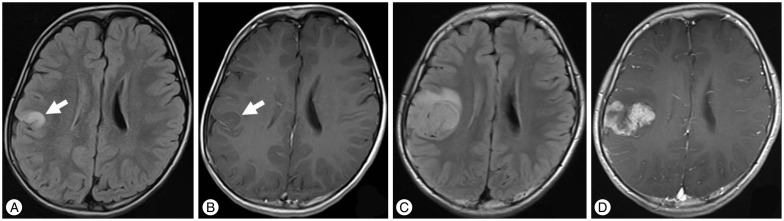
Fig. 2
Intraoperative photograph demonstrating a reddish-gray tumor on the surface of the parietal lobe. It is clearly demarcated from the surrounding brain tissue.

Fig. 3
A : Photomicrographs showing tumor cell proliferation in perivascular pseudorosettes. (HE stain, original magnification ×200). B : Immunohistochemically the tumor cells were positive for glial fibrillary acidic protein (original magnification ×200). C : Ring-like and dot-like epithelial membrane antigen positivity (original magnification ×200). D : Electron micrograph of a tumor cell with a cluster of microvilli (arrow).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download