Abstract
We wish to show our experiance with threating a rare congenital brain malformation-encephalocele. It is a protusion of brain matter with greater incidence in the Far East. Our case is even more curious because of the site of occurrence-frontobasal. Most of encephalocele occur in the occipital region. In this article we report a case of a 57-year-old woman, without deformations on the face, which had epileptic seizures and in spite of receiving antiepileptic drug. She was also frequently treated for sinusitis. She never had rhinoliquorrhea, nor was she diagnosed to have meningitis. In the last few years she had difficulty breathing on her right nostril. After she was diagnosed with encephalocele and treated surgically her recovery was complete and she is without the seizures.
Among the most infrequent anomalies of the central nervous system is protrusion of intracranial masses throughout a defect in the cranium. Encephalocele is one form of neural tube defect. It arise from inadequate closure of neural tube during the first month of embryonic development4). Regarding the tissue protruding through the cranial defect several forms can be distinguished : meningocele represent protrusion of meninges containing cerebrospinal fluid alone, encephalocele denotes protrusion of brain matter, encephalomeningocele consist of brain matter with meninges and CSF, and hidroencephalomeningocele contains brain matter, meninges, CSF and cerebral ventricles. Incidence of encephaloceles is 1 of 3000 live births in countries of the Far East, to 1 of 10000 live births in the Western Hemisphere. They occur in one of 5000 births worldwide. The most common site (75%) of occurrence is occiput, and 90% of the cases involve the midline3). Along with occipital, encephaloceles are anatomically classified as cranial vault, frontoethmoidal and basal ones1). Frontobasal encephaloceles can be classified as anterior type accompanied by visible facial anomalies, hypertelorism and visible and palpable mass in the forehead6), middle type without facial deformities but present rinoliquorrhea, nasal polypes, or meningitis, posterior type often with coloboma, corpus callosum agenesis, cleft lip or palate or both7).
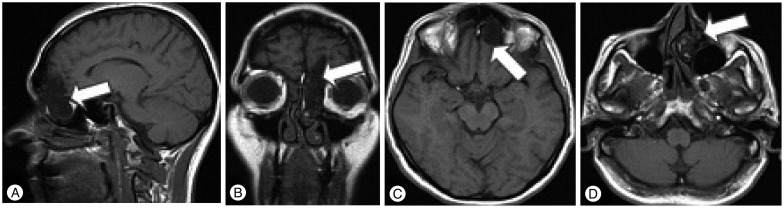
In this article we report a case of a 57-year-old woman who at the age of 24 had her first epileptic seizure, and in spite of receiving antiepileptic drug (Phemiton 200 mg; Pliva Hirvatska d.o.o., Zagreb, Croatia) twice a day she had rare epileptic seizures and headaches of unknown origin. She was also frequently treated for sinusitis. She never had rhinoliquorrhea, nor was she diagnosed to have meningitis. In the last few years she had difficulty breathing on her right nostril. Initial computed tomography (CT) scan of the neurocranium, done 33 years ago and which original scans regretfully are not in our possession, was described by a radiologist to show a shaded paranasal sinuses. The scent of smell is preserved in both nostrils all the time. Throughout the years she had three normal pregnancies and gave birth to three children. Despite antiepileptic therapy, in the last year she had few cases of loss of consciousness, and the headaches became more frequent. She was admitted to do a control neuroradiological exam, and to eventually have her antiepileptic therapy corrected. Initial magnetic resonance imaging (MRI) of the neurocranium was done to show a mass situated partially beneath and partially above the basis of the anterior cranial fossa as shown on Fig. 1.
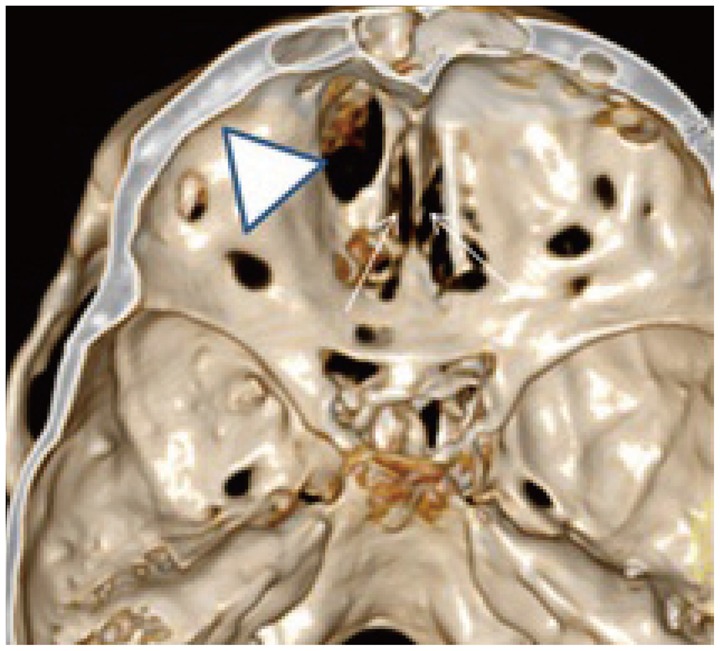
According to the MRI, since she had no facial abnormalities (Fig. 2) she was primarily diagnosed, consistent with neuroradiologist's description, to have either mucocele or aggressive polyposis or fungal infection. She was scheduled for operation prior to which a transnasal preoperative biopsy of the mass was done. The preoperative transnasal biopsy surprisingly caused rhinoliquorrhea and the mass was proven to be brain tissue herniating through a defect in the cranium. Therefore a CT scan with 3D reconstruction of the neurocranium was done. It displayed massive intracranial collection of air and a defect in the anterior cranial fossa, in the paramedial line, lateral to the right lamina cribrosa, as it was shown with CT reconstruction in bone "window", done immediately after transnasal biopsy (Fig. 3).
Transcranial operative approach presented an anterior cranial fossa defect with herniating brain tissue. It showed undamaged olfactory nerve, which explains preserved scent of smell in our patient's right nostril. Protruding brain tissue was removed and the defect was patched with a free musculofascial graft of fascia lata and muscle taken from her right thigh. The graft was sutured on surrounding dasal dura mater with prolen 4-0 (Ethicon, Somerville, NJ, USA) monofilament, polypropylene suture material and then sealed with fibrin adhesive (Duraseal-COVIDIEN, Mansfield OH, USA). Frontal sinuses opened during the operation were stripped of mucosa and sealed with muscle tissue taken from the her right thigh. Sealed frontal sinuses were covered with a vital periostal graft which cranial part was sutured on frontobasal dura mater posterior to defects of the cranium basis. After closing the frontal sinuses and cranium basis the wound was sealed in a regular manner. Thereafter the remaining brain tissue was removed by a transnasal endoscopic procedure by an otorhinolaryngologist. Postoperative MR shows a distinctive delineation between the endocranium and paranasal sinuses.
Our patient has recovered well, has preserved scent of smell on both nostrils, and, with her daily antiepileptic therapy with Phenitoin 2×200 mg, had no epileptic seizures.
Neural tube defects (NTDs) are one of the most common types of birth defects, affecting approximately 1 of every 1000 pregnancies in the United States and an estimated 300000 newborns worldwide each year. The incidence of cranial dysraphism (encephalocele) is far less common than its spinal counterpart, that is, myelomeningocele, accounting for 8% to 19% of all dysraphisms5). Occipital encephaloceles are the most frequent ones occurring in about 75% of all cases. Parietal encephaloceles occur in 10% of all encephaloceles, and the most unfrequent ones are basal occurring in just 1.5% of all encephaloceles2) mostly protruding through cranial sutures or nerve exits. Regarding that 90% of encephaloceles herniate throughout a defect in the midline16) our patient with an encephalocele herniating throughout a paramedial bone defect in anterior cranial fossa is a reason to produce this case report as a presentation of an anatomically extremely rare localisation of this defect and according to literature an extremely rare clinical manifestation of the latter. Of all infants born with NTDs 20.5% have associated malformations. They are more frequently associated with encephalocele (37.5%) than with anencephaly (11.8%) or spina bifida (23.7%). Associated malformations are most commonly ones of the face (oral clefts), of the musculoskeletal and the cardiovascular system. Accompanying neurological pathology may include hydrocephalus, microcephaly, ataxia, developmental delay, vision problems, mental and growth retardation, and seizures. There are some records in literature of epileptic seizures etiologically related to encephaloceles primarily in the middle skull base fossa associated with ipsilateral temporal lobe epilepsy discovered in adulthood successfully treated by surgical procedure. Other abnormalities such as micrognathia, polydactyly, spina bifida, vertebral abnormalities, renal agenesis, pulmonary hypoplasia, dextrocardia, patent ductus arteriosus, septal defects, retinal detachment, vitreous degeneration, agenesis of the corpus callosum, Chiari II malformation, and Dandy-Walker malformation have been noted. Anterior frontobasal encephaloceles are commonly accompanied by hypertelorism, visible and palpable masses in the forehead, medial frequently come with rhinoliquorrhea and nasal polypes, and posterior with coloboma, corpus callosum agenesis and oral clefts. Our patient had none of the above listed accompanying malformations, except for epileptic seizures. She has a face of normal proportion, no visible or palpable forehead masses, no facial clefts, and her rhinoliquorrhea was iatrogenic. So her accompanying pathology was frequent headaches, vague epileptic seizures and mildly obstructed right nostril. She carried out three normal pregnancies. Misdiagnosis of her MRI findings was mucucele, aggressive polyposis and fungal infection. Rhinoliquorrhea caused by transnasal diagnostic biopsy of the protruding mass in the right nostril, and histological finding of brain matter validated that it was an encephalocele.
Encephaloceles can also etiologically be posttraumatic, postoperative or secondary to an erosion of the cranium basis by an inflammatory process, tumor or Wegener's granulomatosis. Rare cause of secondary encephalocele can be cocaine abuse. All secondary causes of a defect in the cranium basis and following encephalocele have been excluded. Conclusively, our patient had a congenital paramedial defect in the anterior cranium fossa with herniating brain tissue in the right nostril causing sinusitis and being an anatomical trigger point for rare epileptic seizures.
With this case report we aimed to indicate to take in consideration an encephalocele when a herniating mass in paranasal sinuses is found, despite lack of rhinoliquorrhea, facial abnormalities or meningitis. A multidisciplinary approach, both transcranial and transnasal assures complete resection of the mass, and optimally ensures defect closure.
References
1. Cho BK, Baek SH, Kim ES, Chung YS, Wang GC, Han DH. The clinical analysis of 22 cases of encephalocele. J Korean Neurosurg Soc. 1991; 20:1040–1047.
2. Elster AD, Branch CL Jr. Transalar sphenoidal encephaloceles : clinical and radiologic findings. Radiology. 1989; 170(1 Pt 1):245–247. PMID: 2909104.

3. Mahajan C, Rath GP, Dash HH, Bithal PK. Perioperative management of children with encephalocele : an institutional experience. J Neurosurg Anesthesiol. 2011; 23:352–356. PMID: 21633311.
4. Rampersaud E, Melvin EC, Speer MC. Nonsyndromic neural tube defects : genetic basis and genetic investigations. In : Wyszynsk DF, editor. Neural Tube Defects : from Origin to Treatment. New York: Oxford University Press;2006. p. 165–175.
5. Shilpakar SK, Sharma MR. Surgical management of encephaloceles. J Neuroscience. 2008; 1:45–48.
6. Suh MS, Hong SK, Kim HJ, Han YP. Sincipital encephalocele : report of 3 operative cases. J Korean Neurosurg Soc. 1987; 16:897–903.
7. Yamashita H, Kurihara M, Kawano T, Mori K, Kunimura M. [Basal encephalomeningocele in an adult-a case report and clinico-anatomical classification]. No Shinkei Geka. 1985; 13:425–431. PMID: 4022246.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download