Abstract
Bone cement augmentation procedures have been getting more position as a minimally invasive surgical option for osteoporotic spinal fractures. However, complications related to these procedures have been increasingly reported. We describe a case of bone cement dislodgement following cement augmentation procedure for osteoporotic spinal fracture by reviewing the patient's medical records, imaging results and related literatures. A 73-year-old woman suffering back and buttock pain following a fall from level ground was diagnosed as an osteoporotic fracture of the 11th thoracic spine. Percutaneous kyphoplasty was performed for this lesion. Six weeks later, the patient complained of a recurrence of back and buttock pain. Radiologic images revealed superior dislodgement of bone cement through the 11th thoracic superior endplate with destruction of the lower part of the 10th thoracic spine. Staged anterior and posterior fusion was performed. Two years postoperatively, the patient carries on with her daily living without any significant disability. Delayed bone cement dislodgement can occur as one of complications following bone cement augmentation procedure for osteoporotic spinal fracture. It might be related to the presence of intravertebral cleft, lack of interdigitation of bone cement with the surrounding trabeculae, and possible damage of endplate during ballooning procedure.
Percutaneous bone cement augmentation procedures including vertebroplasty and kyphoplasty have been performed for painful spinal pathologic fractures such as osteoporotic spinal fractures and other pathologic fractures1). Effective immediate pain relief, less invasive and less morbidity has enhanced its clinical applications. However, this procedure has also limitations and complications by bone cement leakage and embolism2). Higher incidence of subsequent fracture is also suspected to be related to these procedures by alteration of stiffness in the procedure vertebra8). As one of complications following bone cement augmentation for painful osteoporotic spinal fracture, bone cement dislodgement has been rarely reported1112). With a report of this rare complication, we suggest possible causes of this complication through literatures review.
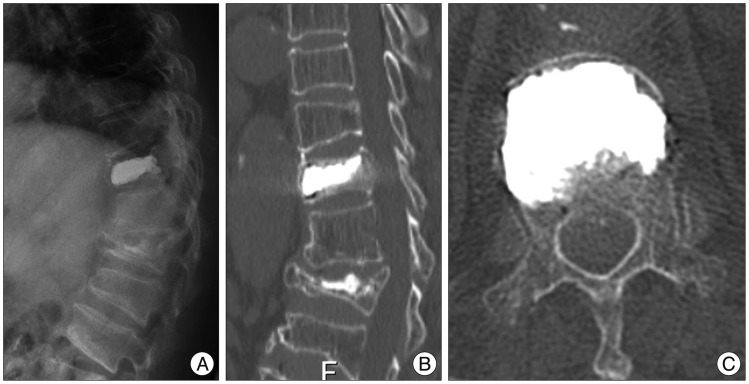
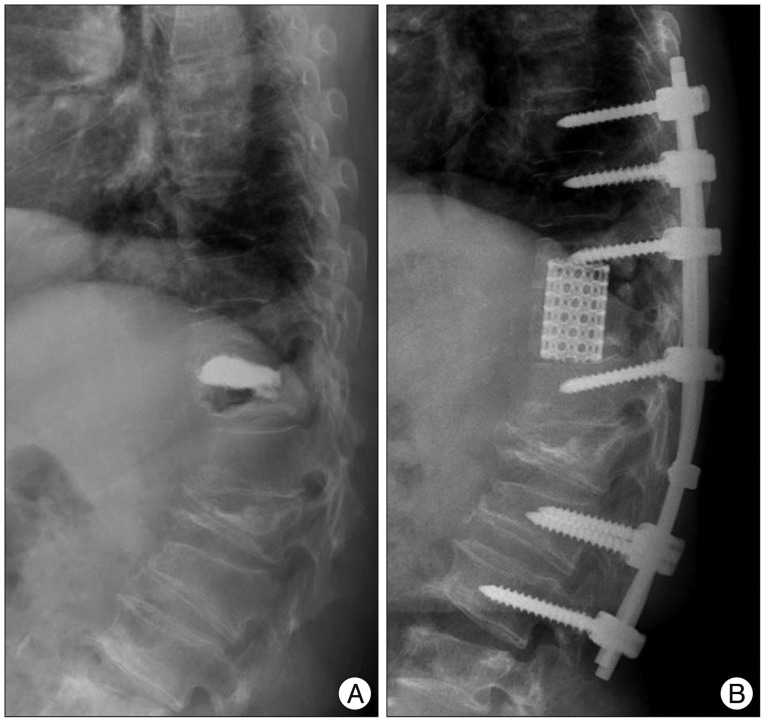
A 73-year-old woman was presented with back and buttock pain following a fall from level ground 1 month ago. She denied the history of medical treatment for osteoporosis. On physical examination, tenderness was noted over the thoraco-lumbar spine. There was no neurological deterioration. On radiological examinations, multi-level height loss of the vertebral body was noted, and there was an intravertebral cleft sign (IVC) at the 11th thoracic spine. Standing and supine cross table lateral radiologic examinations for fracture instability revealed dynamic instability at the fractured lesion. Magnetic resonance images showed signal changes at the fractured vertebra involving mid-column and an IVC (Fig. 1). Dual energy X-ray absorptiometry revealed a bone mineral density T-score -3.4 at the spine. Because of the intractable back pain, which had not been controlled by other conservative treatment, kyphoplasty was performed under diagnosis of osteoporotic spinal fracture with IVC. During the procedure, successful reduction of the fracture was obtained by postural reduction and ballooning. A total of 6 cc polymethylmethacrylate bone cement was injected by bipedicular approach under image intensifier. Postoperative radiographs including CT scan revealed restoration of the fractured vertebra and no cement leakage (Fig. 2). Preoperative Visual Analog Scale (VAS) was 9 and Oswestry Disability Index (ODI) was 78 and both were improved postoperatively to VAS 3 and ODI 25. She discharged without any special event. Six weeks later, she visited our clinics with a recurrence of the back and buttock pain. She stated that her pain was aggravated one week ago without any significant trauma history. Follow-up radiographs showed dislodgement of injected cement through the upper endplate of the 11th thoracic spine and erosion of the lower endplate of the 10th thoracic spine (Fig. 3). Serologic tests done to rule out an infectious condition were normal (WBC 4500; N 4000-10000, ESR 12 mm/h; N 0-20, CRP 0.03 mg/dL; N 0.01-0.47). Staged anterior and posterior fusion was performed. During the anterior surgery through trans-thoracic approach, superiorly migrated bone cement and erosion of the lower endplate of the upper segment was found. After complete removal of bone cement, anterior interbody fusion was performed using mesh cage and autogenous iliac bone. Two weeks later, additional posterior stabilization and posterior fusion was done. Two years postoperatively, the patient was asymptomatic without any episode of metallic failure or subsequent fracture.
Bone cement augmentation procedures (CAP) including vertebroplasty and kyphoplasty are attractive procedures for limited cases of painful osteoporotic and malignant spinal fracture1). Even though there are many advantages including its being less invasive, having less morbidity, and being a relative simple procedure with effective results, these procedures are not free of complications. Moreover, since Kallmes et al.6) presented similar clinical results following conservative treatment for osteoporotic vertebral compression fractures comparing to the bone cement augmentation. This procedure is being faced with challenges regarding its clinical usefulness. In addition, various complications of cement leakage including cement embolism and neurological complications have been reported2). Besides these complications, some authors suggested that subsequent fractures at the adjacent segment might be related to biomechanical alteration of the affected vertebra by bone cement8). For these failed CAP, revision surgeries have been reported313). Bone cement dislodgement has rarely been reported as one of complications following CAP (Table 1)91112). In these reports, IVC sign and fracture instability were among the common findings, and the authors described the lack of inter-digitation of bone cement into the surrounding trabeculae and thermal damage during the polymeralization as potential factors for dislodgement. Even though dislodgement of bone cement following kyphoplasty has not occurred, aseptic necrosis of the surrounding bone has also been reported9). The authors described that the total volume of injected bone cement except for the abovementioned factors might be related to aseptic osteonecrosis based on other biomechanical data. Too much bone cement resulted in an insufficient bone cement contact interface by distraction of the fractured vertebra. As these reports revealed, an IVC in osteoporotic spinal fracture is associated with a deteriorated healing process. The presence of IVC is also related to poor surgical results following CAP through recollapse or progressive kyphosis5710). However, as Hashidate et al.4) reported in their prospective observation of IVC, disappearance of IVC can be also observed during the follow-ups. And they insisted that observation of IVC on radiographs does not always correlate with a clinical significance. Therefore, in these days, many authors agree that both the presence of IVC and instability at the affected vertebra are significant factors for these complicated osteoporotic spinal fractures. In these aspects, this case might have resulted from misleading application of CAP. Other reported cases causing revision surgery following CAP showed a relative large portion of IVC and dynamic instability on radiographs including this case. Therefore, more attention should be paid to performing the CAP for the complicated osteoporotic spinal fractures with significant IVC and dynamic instability.
Unlike the other reported cases, dislodgement of bone cement occurred through the upper endplate of the affected vertebra. The endplate is known to be the strongest part of the vertebral body. Although we are not able to verify disruption of the endplate through retrospective review of pre- and post-operative radiographs, damage of endplate during intraoperative ballooning might be one of possible mechanisms of upward dislodgement of bone cement.
Even though CAP is a simple and effective procedure for management of painful osteoporotic spinal fractures, delayed cement dislodgement can still occur, and this rare complication might be related to IVC, lack of inter-digitation of bone cement with the surrounding trabeculae, and possible damage of endplate during ballooning procedure.
Acknowledgements
This research was supported by Seoul St. Mary's Clinical Medicine Research Program year of 2011 through the Catholic University of Korea.
References
1. Boonen S, Wahl DA, Nauroy L, Brandi ML, Bouxsein ML, Goldhahn J, et al. Balloon kyphoplasty and vertebroplasty in the management of vertebral compression fractures. Osteoporos Int. 2011; 22:2915–2934. PMID: 21789685.

2. Chen HL, Wong CS, Ho ST, Chang FL, Hsu CH, Wu CT, et al. A lethal pulmonary embolism during percutaneous vertebroplasty. Anesth Analg. 2002; 95:1060–1062. PMID: 12351294.

3. Ha KY, Kim KW, Kim YH, Oh IS, Park SW. Revision surgery after vertebroplasty or kyphoplasty. Clin Orthop Surg. 2010; 2:203–208. PMID: 21119935.

4. Hashidate H, Kamimura M, Nakagawa H, Takahara K, Uchiyama S. Pseudoarthrosis of vertebral fracture : radiographic and characteristic clinical features and natural history. J Orthop Sci. 2006; 11:28–33. PMID: 16437345.

5. He SC, Teng GJ, Deng G, Fang W, Guo JH, Zhu GY, et al. Repeat vertebroplasty for unrelieved pain at previously treated vertebral levels with osteoporotic vertebral compression fractures. Spine (Phila Pa 1976). 2008; 33:640–647. PMID: 18344858.

6. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009; 361:569–579. PMID: 19657122.

7. Matsumoto T, Hoshino M, Tsujio T, Terai H, Namikawa T, Matsumura A, et al. Prognostic factors for reduction of activities of daily living following osteoporotic vertebral fractures. Spine (Phila Pa 1976). 2012; 37:1115–1121. PMID: 22158062.

8. Mudano AS, Bian J, Cope JU, Curtis JR, Gross TP, Allison JJ, et al. Vertebroplasty and kyphoplasty are associated with an increased risk of secondary vertebral compression fractures : a population-based cohort study. Osteoporos Int. 2009; 20:819–826. PMID: 18797812.

9. Mueller M, Daniels-Wredenhagen M, Besch L, Decher C, Seekamp A. Postoperative aseptic osteonecrosis in a case of kyphoplasty. Eur Spine J. 2009; 18(Suppl 2):213–216. PMID: 19089465.

10. Oka M, Matsusako M, Kobayashi N, Uemura A, Numaguchi Y. Intravertebral cleft sign on fat-suppressed contrast-enhanced MR : correlation with cement distribution pattern on percutaneous vertebroplasty. Acad Radiol. 2005; 12:992–999. PMID: 16087094.
11. Tsai TT, Chen WJ, Lai PL, Chen LH, Niu CC, Fu TS, et al. Polymethylmethacrylate cement dislodgment following percutaneous vertebroplasty : a case report. Spine (Phila Pa 1976). 2003; 28:E457–E460. PMID: 14624094.
12. Wang HS, Kim HS, Ju CI, Kim SW. Delayed bone cement displacement following balloon kyphoplasty. J Korean Neurosurg Soc. 2008; 43:212–214. PMID: 19096648.

13. Yang SC, Chen WJ, Yu SW, Tu YK, Kao YH, Chung KC. Revision strategies for complications and failure of vertebroplasties. Eur Spine J. 2008; 17:982–988. PMID: 18446385.

Fig. 1
Standing (A) and trans-table lateral (B) radiographs show dynamic instability at the fractured site. Low signal within high signal on T2-weighted magnetic resonance images (C) represent the intravertebral cleft consisting of air and fluid components. Arrow indicates the 11th thoracic spine.
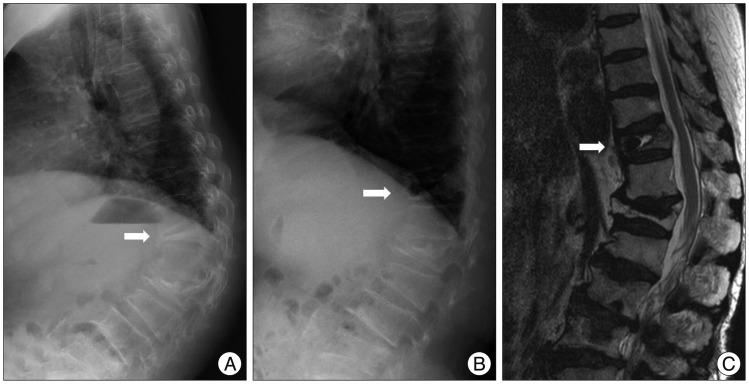
Fig. 2
Postoperative plain radiographs (A) and CT scans (B and C) demonstrate restoration of height of the vertebra body and filled bone cement without significant leakage.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download