Abstract
Chiari type I malformation is a tonsillar herniation more than 3 mm from the level of foramen magnum, with or without concurrent syringomyelia. Different surgical treatments have been developed for syringomyelia secondary to Chiari's malformations: craniovertebral decompression with or without plugging of the obex, syringo-subarachnoid, syringo-peritoneal, and theco-peritoneal shunt placement. Shunt placement procedures are useful for neurologically symptomatic large-sized syrinx. In this paper, authors define the first successful treatment of a patient with syringomyelia due to Chiari type I malformation using a pre-defined new technique of syringo-subarachnoid-peritoneal shunt with T-tube system.
Hans Chiari, an Austrian pathologist (1851-1916), described Chiari malformations and classified them into 4 types13). According to this classification; Chiari type I is at least 3 mm downward displacement of cerebellar tonsils below the foramen magnum, Chiari type II is related with downward displacement of posterior fossa elements with accompanying myelomeningocele, Chiari type III is herniation of posterior fossa elements into an occipital or a cervical encephalocele, the last one is type IV seen in cerebellar hypoplasia event14). Syringomyelia may accompany Chiari type I malformation as in the other Chiari malformation types. In the literature, craniovertebral decompression (CVD) and/or syringo-subarachnoid/syringo-peritoneal/syringo-cisternostomy have been justified as the method(s) of treatment for syringomyelia associated with Chiari type I malformation9,12,14).
In this paper, authors define the first successful treatment of a patient with syringomyelia due to Chiari type I malformation using a pre-defined new technique of syringo-subarachnoid-peritoneal shunt with T-tube, described by Kim et al.11).
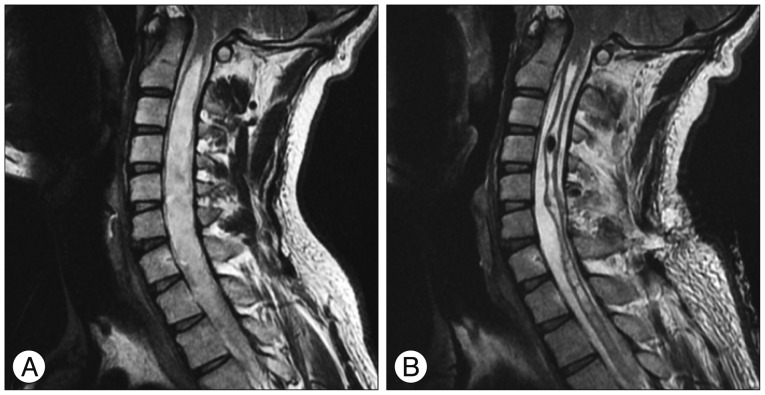
A 34-year-old man presented to our outpatient clinic with a 3-month history of an increasing numbness and weakness in his four extremities. He also mentioned having difficulties in walking, which started a month ago. There was no trauma or infection history. Neurologic examination revealed decreased proprioception, pain and temperature sensations in all extremities. There was 1/5 loss of motor function on his right body part. Magnetic resonance imaging revealed a tonsillar herniation with a large syringomyelia in the spinal cord starting from just below the foramen magnum level and ending at the level of T5 vertebral body. The spinal cord was thinned at these levels (Fig. 1A). There was no spinal dysraphism. Laboratory test results were normal. Somatosensory evoked potentials (SEP) were abnormal (increased N13-20 interval, reduced cortical amplitude from posterior tibial nerve).
We planned syringo-subarachnoid-peritoneal shunt insertion using a conventional lumbo-peritoneal shunt and a T-tube (Medtronic Neurosurgery, Goleta, CA, USA). After induction of general anesthesia, we turned the patient in prone position. In an attempt to explore the widest portion of syrinx, we made laminectomy at the 6th and 7th cervical levels. Following the incision of dura and arachnoid membranes, we made a small dorsal myelotomy. The T-tube side arms, which have many holes on it, are designated long enough for a desired length. While we inserted one side arm of T-tube into the syrinx, we placed the other side arm into the subarachnoid space. We sutured the side arm in the subarachnoid space to the dura and surrounding ligaments. We made the connection between the T-tube and lumbo-peritoneal shunt system. We passed the other free side end of the lumbo-peritoneal shunt to the left flank region through subcutaneous way. After positioning the patient in a lateral decubitus position for the second stage of the procedure, we rechanneled the shunt system to the left para-umbilical area and inserted the distal end into the peritoneal cavity using the standard shunt technique (Fig. 2).
The surgery was uneventful. On his follow-up, the global strength of the right upper extremity and whole sensory function in four extremities, especially proprioception, significantly improved. Postoperative magnetic resonance (MR) image one year after the surgery showed that tonsillar herniation level was the same as before the surgery; however a significant reduction in syringomyelia size was noticed. His SEP test turned to normal (Fig. 1B) and he was in well condition.
Chiari malformation was described by Han Chiari in his prestigious monograph "Ueber Veränderungen des Kleinhirns infolge von Hydrocephalie des Grosshirns" in 18913). He described Chiari's type I malformation as "peg-like elongation of tonsils and medial divisions of the inferior lobes of the cerebellum into cone-shaped projections, which accompany the medulla oblongata into the spinal canal"3,13). Later on, he described the other variants of this malformation as type II, III, and IV13). In 1998, Iskandar et al.10) defined a new type of Chiari malformation as type 0. Our patient had no previous trauma or infection history. His MR showed a tonsillar herniation compatible with Chiari type I malformation and there was also an accompanying cervico-thoracic syringomyelia.
Syringomyelia is a pathological state of a longitudinal cavity extending in the vertical axis of the spinal cord1). It was first defined in 1688 by Johann Conrad Brunner (1653-1727) as "a large cavity in the spinal cord extending from the fourth ventricle to the dorsal vertebrae". Charles Prosper Ollivier d'Angers (1796-1845) is the scientist who gave the name of "syringomyelia"2).
Different surgical treatments have been imposed for syringomyelia secondary to Chiari's malformations : CVD with or without plugging of the obex; syringo-subarachnoid, syringo-peritoneal and theco-peritoneal shunt placement8,9). Some papers found CVD effective, and some others depicted shunt procedures as effective. In a study of Hida et al.9), they treated 70 symptomatic syringomyelia patients with Chiari type I malformation (age range 3-59 years; median, 29.4 years) either with CVD or syringo-subarachnoid shunt placement procedure. They preferentially treated patients with lower cranial nerve palsy or nystagmus and small syrinx cavity via CVD procedure (33 patients); patients with large syringomyelia (syrinx width more than 70% of the spinal cord width at the same level) with shunt method (37 patients). The results depicted that neurological improvement was gained in 82% of patients operated with CVD, in 97% of the patients treated with syringo-subarachnoid shunt. Syringomyelia diminished in size faster with shunt procedures (1.8 weeks vs. 6.3 weeks)9). Complications related with shunt procedures are mainly due to technical issues such as shunt malfunction, shunt migration, arachnoiditis that leads to fibrosis around shunt tube openings, increase of tonsillar descent8,9). A failure rate between 0-40% has been reported for CVD procedures in the literature4,7,17,19,21,23). There are some described failure reasons in CVD procedures as inadequate bone removal at the foramen magnum, residual C1 lamina, arachnoid web, suture involving obex, pseudomeningocele, intradural and/or extradural adhesion, meningitis7,9,16). In our case, syringomyelia cavity was large and there were no lower cranial nerve palsy or nystagmus; so we preferred a shunt procedure instead of CVD. To overcome some disadvantages of conventional syringo-subarachnoid shunt we used the new shunt system described by Kim et al.11), who used syringo-subarachnoid-peritoneal shunt with T-tube for treatment of syringomyelia secondary to trauma. In this technique a conventional T-tube and lumbo-peritoneal shunt are used together. After making a small dorsal myelotomy incision at the widest level of the syrinx, one side arm of T-tube is inserted into the cavity in rostral direction. The other side arm is anchored into the subarachnoid space with a stich to the dura and surrounding ligaments. T-tube is connected to the lumbo-peritoneal shunt system and the rest of the procedure is completed like in a standard shunt procedure11). After the procedure, the patient in our case got better and normalized in 6 months' time. In the last control, 1 year after the procedure, he was still well and his control MRI depicted that level of tonsillar descent was the same as before the surgery; however the syrinx size had dramatically collapsed (Fig. 1B).
Neurologically symptomatic large syringomyelia cavities secondary to Chiari type I malformations should be treated surgically. Authors demonstrated the first successful application of syringo-subarachnoid-peritoneal shunt with T-tube system in a Chiari type I malformation patient. However, more clinical series with long follow-up are needed to make a general assessment of the success of this procedure in this patient population.
Acknowledgements
Murat Şakir Ekşi, M.D. was supported by a grant from Tubitak (The Scientific and Technological Research Council of Turkey), Grant number : 1059B191400255.
References
1. Ataizi S, Canakçi Z, Baloğlu M, Cerezci A. Spontaneously resorbed idiopathic syringomyelia : a case report. Turk Neurosurg. 2007; 17:247–250. PMID: 18050066.
2. Bosmia AN, Tubbs RI, Clapp DC, Batzdorf U, Loukas M, Tubbs RS. Johann Conrad Brunner (1653-1727) and the first description of syringomyelia. Childs Nerv Syst. 2014; 30:193–196. PMID: 24481626.

3. Chiari H. Ueber Veränderungen des Kleinhirns infolge von Hydrocephalie des Grosshirns. Dtsch Med Wochenschr. 1891; 17:1172–1175.

4. Depreitere B, Van Calenbergh F, van Loon J, Goffin J, Plets C. Posterior fossa decompression in syringomyelia associated with a Chiari malformation : a retrospective analysis of 22 patients. Clin Neurol Neurosurg. 2000; 102:91–96. PMID: 10817895.

5. Feldstein NA, Choudhri TF. Management of Chiari I malformations with holocord syringohydromyelia. Pediatr Neurosurg. 1999; 31:143–149. PMID: 10708356.

6. Gardner WJ, Goodall RJ. The surgical treatment of Arnold-Chiari malformation in adults; an explanation of its mechanism and importance of encephalography in diagnosis. J Neurosurg. 1950; 7:199–206. PMID: 15415776.
7. Heiss JD, Suffredini G, Smith R, DeVroom HL, Patronas NJ, Butman JA, et al. Pathophysiology of persistent syringomyelia after decompressive craniocervical surgery. Clinical article. J Neurosurg Spine. 2010; 13:729–742. PMID: 21121751.

8. Hida K, Iwasaki Y. Syringosubarachnoid shunt for syringomyelia associated with Chiari I malformation. Neurosurg Focus. 2001; 11:E7. PMID: 16724817.

9. Hida K, Iwasaki Y, Koyanagi I, Sawamura Y, Abe H. Surgical indication and results of foramen magnum decompression versus syringosubarachnoid shunting for syringomyelia associated with Chiari I malformation. Neurosurgery. 1995; 37:673–678. discussion 678-679. PMID: 8559295.

10. Iskandar BJ, Hedlund GL, Grabb PA, Oakes WJ. The resolution of syringohydromyelia without hindbrain herniation after posterior fossa decompression. J Neurosurg. 1998; 89:212–216. PMID: 9688115.

11. Kim SH, Choi SW, Youm JY, Kwon HJ. Syringo-subarachnoid-peritoneal shunt using T-tube for treatment of post-traumatic syringomyelia. J Korean Neurosurg Soc. 2012; 52:58–61. PMID: 22993681.

12. Klekamp J. Neurological deterioration after foramen magnum decompression for Chiari malformation type I : old or new pathology? J Neurosurg Pediatr. 2012; 10:538–547. PMID: 23039841.

13. Loukas M, Noordeh N, Shoja MM, Pugh J, Oakes WJ, Tubbs RS. Hans Chiari (1851-1916). Childs Nerv Syst. 2008; 24:407–409. PMID: 18066558.

14. Markunas CA, Tubbs RS, Moftakhar R, Ashley-Koch AE, Gregory SG, Oakes WJ, et al. Clinical, radiological, and genetic similarities between patients with Chiari Type I and Type 0 malformations. J Neurosurg Pediatr. 2012; 9:372–378. PMID: 22462700.

15. Milhorat TH, Miller JI, Johnson WD, Adler DE, Heger IM. Anatomical basis of syringomyelia occurring with hindbrain lesions. Neurosurgery. 1993; 32:748–754. discussion 754. PMID: 8492850.

16. Naftel RP, Tubbs RS, Menendez JY, Wellons JC 3rd, Pollack IF, Oakes WJ. Worsening or development of syringomyelia following Chiari I decompression : case report. J Neurosurg Pediatr. 2013; 12:351–356. PMID: 23931767.

17. Navarro R, Olavarria G, Seshadri R, Gonzales-Portillo G, McLone DG, Tomita T. Surgical results of posterior fossa decompression for patients with Chiari I malformation. Childs Nerv Syst. 2004; 20:349–356. PMID: 15022006.

18. Oldfield EH, Muraszko K, Shawker TH, Patronas NJ. Pathophysiology of syringomyelia associated with Chiari I malformation of the cerebellar tonsils. Implications for diagnosis and treatment. J Neurosurg. 1994; 80:3–15. PMID: 8271018.

19. Tubbs RS, Webb DB, Oakes WJ. Persistent syringomyelia following pediatric Chiari I decompression : radiological and surgical findings. J Neurosurg. 2004; 100(5 Suppl Pediatrics):460–464. PMID: 15287455.

20. Van den Bergh R. Pathogenesis and treatment of delayed post-traumatic syringomyelia. Acta Neurochir (Wien). 1991; 110:82–86. PMID: 1882724.

21. Wetjen NM, Heiss JD, Oldfield EH. Time course of syringomyelia resolution following decompression of Chiari malformation Type I. J Neurosurg Pediatr. 2008; 1:118–123. PMID: 18352779.

22. Williams B. On the pathogenesis of syringomyelia : a review. J R Soc Med. 1980; 73:798–806. PMID: 7017117.
23. Zhang ZQ, Chen YQ, Chen YA, Wu X, Wang YB, Li XG. Chiari I malformation associated with syringomyelia : a retrospective study of 316 surgically treated patients. Spinal Cord. 2008; 46:358–363. PMID: 18026173.

Fig. 2
First patient is in prone position and after C6-7 laminectomy, incision of dura and arachnoid membrane, we made a small dorsal myelotomy; while we inserted one arm of the T-tube into the syrinx, we placed the other arm in the subarachnoid space and tunneled distal part to the subcutaneous space at left flank region where the catheter was taken outside and carefully wrapped to provide the sterility. After positioning the patient in a lateral decubitus position, we rechanneled the catheter to the left para-umbilical area and inserted the distal part into the peritoneal cavity using the standard technique.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download